Infect Chemother.
2017 Dec;49(4):262-267. 10.3947/ic.2017.49.4.262.
Response of Vancomycin according to Steroid Dosage in Pediatric Patients with Culture-Proven Bacterial Meningitis
- Affiliations
-
- 1Department of Pediatrics, Chonbuk National University Medical School, Jeonju, Korea. sunjun@jbnu.ac.kr
- 2Research Institute of Clinical Medicine, Chonbuk National University Medical School, Jeonju, Korea.
- KMID: 2399193
- DOI: http://doi.org/10.3947/ic.2017.49.4.262
Abstract
- BACKGROUND
This study aimed to evaluate the efficacy of combined vancomycin and steroid therapy for the treatment of culture-proven bacterial meningitis in pediatric patients.
MATERIALS AND METHODS
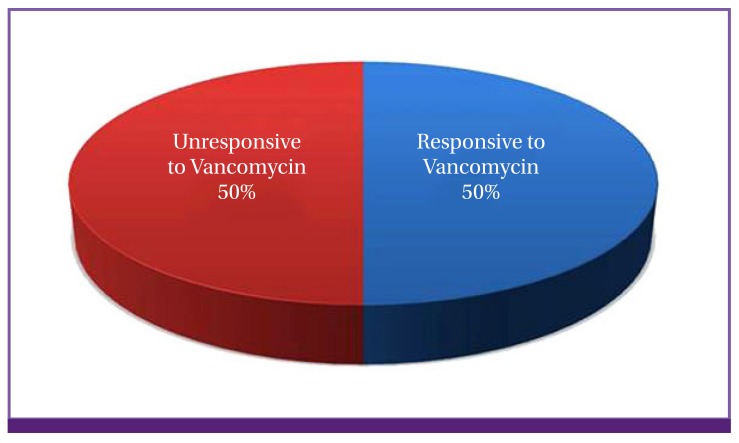
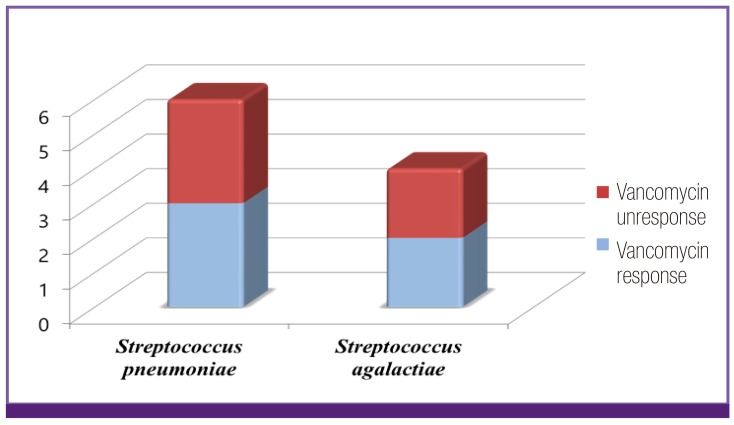
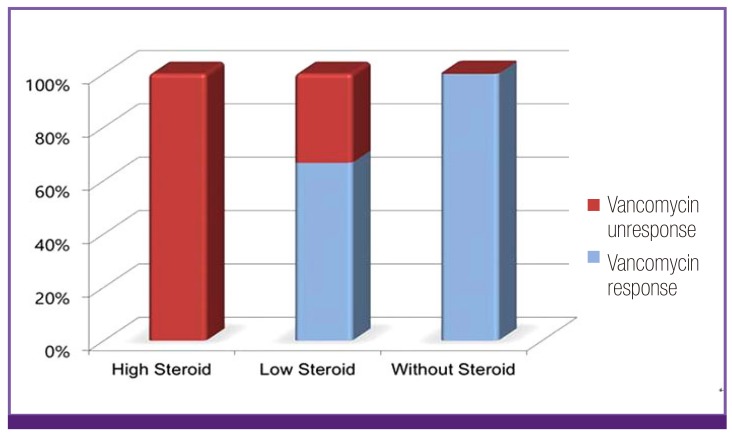
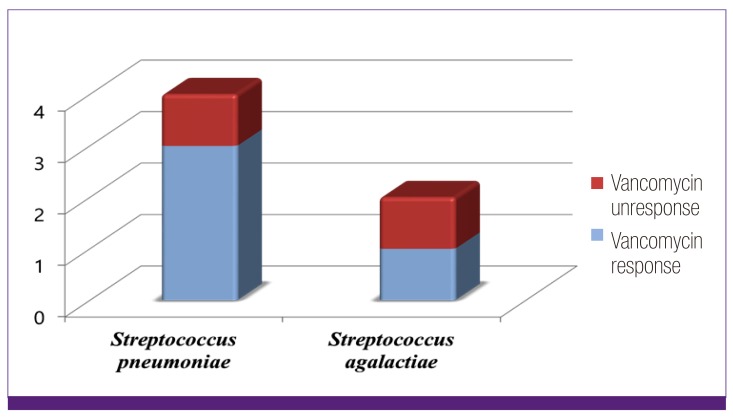
We identified a total of 86 pediatric patients with culture-positive cerebrospinal fluid who were treated at our facility between 2005 and 2015. Ten of these patients (5 boys and 5 girls) received first-line treatment with vancomycin as the initial form of therapy. All cultured bacteria were sensitive to vancomycin. We retrospectively analyzed these cases to examine the relationship between concomitant steroid dosage and antibiotic treatment effectiveness.
RESULTS
Nine of the 10 patients included in our analysis received steroid treatment. Of these, 3 received high-dose steroid therapy and 6 received low-dose steroid therapy. Five patients did not respond to vancomycin, including all 3 patients in the high-dose steroid group and 2 patients in the low-dose steroid group. Our analysis confirmed that the response rate to vancomycin treatment was significantly reduced in accordance with steroid dosage (P = 0.035). Patients who did not to respond to vancomycin with concomitant high-dose steroid administration improved clinically after the substitution of vancomycin with teicoplanin.
CONCLUSION
The use of steroids, especially in high doses, may impair the effectiveness of vancomycin for treating bacterial meningitis in pediatric patients. Physicians should be cautious when administering concomitant steroid therapy and should carefully monitor the steroid dosage.
Keyword
MeSH Terms
Figure
Reference
-
1. Chávez-Bueno S, McCracken GH Jr. Bacterial meningitis in children. [vii.]. Pediatr Clin North Am. 2005; 5:795–810.
Article2. van de Beek D, de Gans J, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med. 2004; 351:1849–1859. PMID: 15509818.
Article3. Brouwer MC, McIntyre P, Prasad K, van de Beek D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst Rev. 2015; 12:CD004405.
Article4. Wubbel L, McCracken GH Jr. Management of bacterial meninigitis: 1998. Pediatr Rev. 1998; 19:78–84. PMID: 9509854.5. Brady MT, Kaplan SL, Taber LH. Association between persistence of pneumococcal meningitis and dexamethasone administration. J Pediatr. 1981; 99:924–926. PMID: 7310585.
Article6. Scheld WM, Brodeur JP. Effect of methylprednisolone on entry of ampicillin and gentamicin into cerebrospinal fluid in experimental pneumococcal and Escherichia coli meningitis. Antimicrob Agents Chemother. 1983; 23:108–112. PMID: 6338816.7. Pfausler B, Schmutzhard E. Controversies in neurology, Vienna, 2012: steroids in bacterial meningitis. J Neural Transm (Vienna). 2013; 120:343–346. PMID: 23263539.8. Spapen H, Van Berlaer G, Moens M, Hubloue I. Adjunctive steroid treatment in acute bacterial meningitis, “To do or not to do: that is the question. Acta Clin Belg. 2011; 66:42–45. PMID: 21485762.9. Viladrich PF. Management of meningitis caused by resistant Streptococcus pneumoniae. In : Gillespie SH, editor. Management of multiple drug-resistance infections. Totowa, NJ: Humana Press;2004. p. 31–48.10. Täuber MG, Moser B. Cytokines and chemokines in meningeal inflammation: biology and clinical implications. Clin Infect Dis. 1999; 28:1–11. PMID: 10028061.
Article11. Täuber MG, Khayam-Bashi H, Sande MA. Effects of ampicillin and corticosteroids on brain water content, cerebrospinal fluid pressure, and cerebrospinal fluid lactate levels in experimental pneumococcal meninigits. J Infect Dis. 1985; 151:528–534. PMID: 3973406.12. Mai NT, Tuan TV, Wolbers M, Hoang DM, Nga TV, Chau TT, Chuong LV, Sinh DX, Nghia HD, Phong ND, Phu NH, Diep TS, Hang HT, Chau Nv, Farrar J, Schultsz C, Hien TT, Simmons CP. Immunological and biochemical correlates of adjunctive dexamethasone in Vietnamese adults with bacterial meningitis. Clin Infect Dis. 2009; 49:1387–1392. PMID: 19814625.
Article13. Gerber J, Nau R. Mechanisms of injury in bacterial meningitis. Curr Opin Neurol. 2010; 23:312–318. PMID: 20442574.
Article14. Esposito S, Semino M, Picciolli I, Principi N. Should corticosteroids be used in bacterial meningitis in children? Eur J Paediatr Neurol. 2013; 17:24–28. PMID: 22789668.
Article15. Gerber J, Tauber SC, Armbrecht I, Scchmidt H, Brück W, Nau R. Increased neuronal proliferation in human bacterial meningitis. Neurology. 2009; 73:1026–1032. PMID: 19786694.
Article16. Leib SL, Heimgartner C, Bifrare YD, Loeffler JM, Täauber MG. Dexamethasone aggravates hippocampal apoptosis and learning deficiency in pneumococcal meningitis in infant rates. Pediatr Res. 2003; 54:353–357. PMID: 12788989.17. Viladrich PF, Gudiol F, Liñares J, Pallarés R, Sabaté I, Rufí G, Ariza J. Evaluation of vancomycin for therapy of adult pneumococcal meningitis. Antimicrob Agents Chemother. 1991; 35:2467–2472. PMID: 1810180.
Article18. París MM, Hickey SM, Uscher MI, Shelton S, Olsen KD, McCracken GH Jr. Effect of dexamethasone on therapy of experimental penicillin and cephalosporin resistant pneumococcal meningitis. Antimicrob Agents Chemother. 1994; 38:1320–1324. PMID: 8092832.19. Cabellos C, Martinez-Lacasa J, Martos A, Tubau F, Fernández A, Viladrich PF, Gudiol F. Influence of dexamethasone on efficacy of ceftriaxone and vancomycin therapy in experimental pneumococcal meningitis. Antimicrob Agents Chemother. 1995; 39:2158–2160. PMID: 8540738.
Article20. Kaal EC, Vecht CJ. The management of brain edema in brain tumors. Curr Opin Oncol. 2004; 16:593–600. PMID: 15627023.
Article21. Lee SW, Kim WJ, Choi YK, Song HS, Son MJ, Gelman IH, Kim YJ, Kim KW. SSeCKS regulates angiogenesis and tight junction formation in blood-brain barrier. Nat Med. 2003; 9:900–906. PMID: 12808449.
Article22. Hori S, Ohtsuki S, Hosoya K, Nakashima E, Terasaki T. A pericyte-derived angiopoietin-1 multimeric complex induces occluding gene expression in brain capillary endothelial cells through Tie-2 activation in vitro. J Neurochem. 2004; 89:503–513. PMID: 15056293.23. Nag S, Papneja T, Venuqopalan R, Stewart DJ. Increased angiopoietin2 expression is associated with endothelial apoptosis and blood brain barrier breakdown. Lab Invest. 2005; 85:1189–1198. PMID: 16056241.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Value of Urine Latex Test In Bacterial Meningitis
- Clinical Study of Treatment of Group B Streptococcal Meningitis in Neonates
- A clinical study on neonatal bacterial meningitis
- Treatment and Prognosis according to Causative Organisms in Neonatal Bacterial Meningitis
- Causative Organisms and Antibiotic Susceptibility of Bacterial Meningitis in Children: Experience of a Single Center