J Rhinol.
2017 Nov;24(2):118-122. 10.18787/jr.2017.24.2.118.
A Case of Primary Ciliary Dyskinesia
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Korea University College of Medicine, Seoul, Korea. doctorth@korea.ac.kr
- KMID: 2398830
- DOI: http://doi.org/10.18787/jr.2017.24.2.118
Abstract
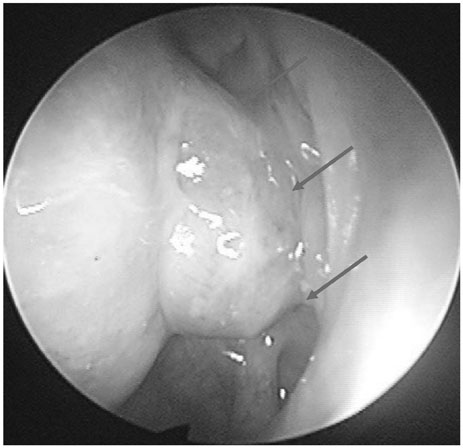
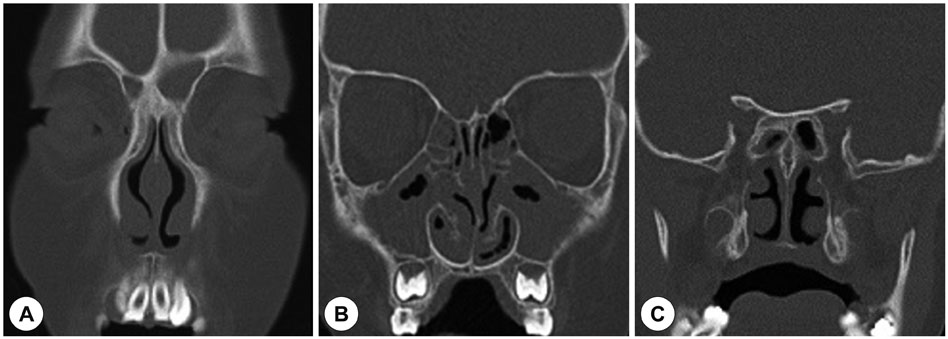
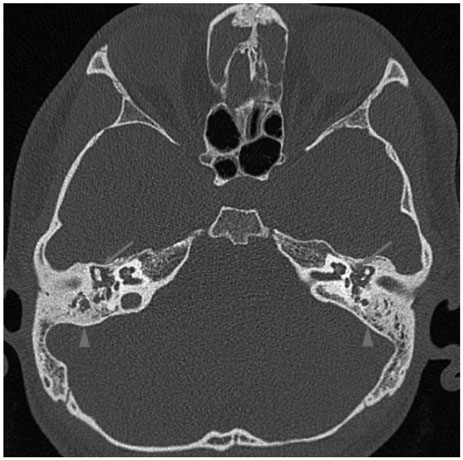
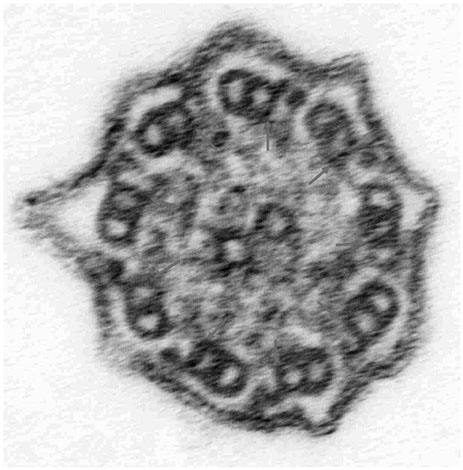
- Primary ciliary dyskinesia is a disease characterized by unexplained neonatal respiratory distress, otitis media, chronic sinusitis, and chronic bronchiectasis. In approximately half of cases, situs inversus totalis or other laterality defects are found. The incidence ranges from 1 in 4,000 to 1 in 40,000 live births. Early diagnosis is important and the disease is finally confirmed by electron microscopic biopsy. The treatment of primary ciliary dyskinesia is based on appropriate procedures. We present a rare case of a 20-year-old male with bronchiectasis, chronic otitis media and chronic sinusitis.
MeSH Terms
Figure
Reference
-
1. Horani A, Ferkol TW. Primary ciliary dyskinesia and associated sensory ciliopathies. Expert Rev Respir Med. 2016; 10(5):569–576.
Article2. Lewis WR, Malarkey EB, Tritschler D, Bower R, Pasek RC, Porath JD, et al. Mutation of Growth Arrest Specific 8 Reveals a Role in Motile Cilia Function and Human Disease. PLoS Genet. 2016; 12(7):e1006220.
Article3. Mitchison HM, Valente EM. Motile and non-motile cilia in human pathology: from function to phenotypes. J Pathol. 2017; 241(2):294–309.
Article4. Lucas JS, Burgess A, Mitchison HM, Moya E, Williamson M, Hogg C. Diagnosis and management of primary ciliary diskynesia. Arch Dis Child. 2014; 99:850–856.5. Park CW, Koh JS, Kim KR, Lee HS. A Clinical Study on Primary Ciliary Dyskinesia. Korean J Otolaryngol-Head Neck Surg. 1997; 40:1079–1084.6. Shin SA, Yang S, Oh JW, Lee HB, Park CE, Kwan JK. Ultrastructure of nasal cilia in children with recurrent or persistent respiratory diseases. Korean J Pediatr. 2006; 49:410–416.
Article7. Hogg C. Primary ciliary dyskinesia: when to suspect the diagnosis and how to confirm it. Paediatr Respir Rev. 2009; 10:44–50.
Article8. Popatia R, Haver K, Casey A. Primary Ciliary Dyskinesia: An Update on New Diagnostic Modalities and Review of the Literature. Pediatr Allergy Immunol Pulmonol. 2014; 27(2):51–59.
Article9. Storm van's Gravesande K, Omran H. Primary Ciliary Dyskinesia: clinical presentation, diagnosis and genetics. Ann Med. 2005; 37(6):439–449.10. Ryu JS, Jeong DW, Park YK, Kim KS. A Case of Kartagener's Syndrome Combined with Congenital Nystagmus. Korean J Otolaryngol-Head Neck Surg. 2001; 44:657–661.11. Leigh MW, O'Callaghan C, Knowles MR. The challenges of diagnosing primary ciliary dyskinesia. Proc Am Thorac Soc. 2011; 8(5):434–437.
Article12. Walker WT, Jackson CL, Lackie PM, Hogg C, Lucas JS. Nitric oxide in primary ciliary dyskinesia. Eur Respir J. 2012; 40(4):1024–1032.
Article13. Corbelli R, Bringolf-Isler B, Amacher A, Sasse B, Spycher M, Hammer J. Nasal nitric oxide measurements to screen children for primary ciliary dyskinesia. Chest. 2004; 126(4):1054–1059.
Article14. Jackson CL, Behan L, Collins SA, Goggin PM, Adam EC, Coles JL, et al. Accuracy of diagnostic testing in primary ciliary dyskinesia. Eur Respir J. 2016; 47(3):837–848.
Article15. Knowles MR, Daniels LA, Davis SD, Zariwala MA, Leigh MW. Primary Ciliary Dyskinesia. Recent Advances in Diagnostics, Genetics, and Characterization of Clinical Disease. Am J Respir Crit Care Med. 2013; 188(8):913–922.
Article16. Bush A, Cole P, Hariri M, Mackay I, Phillips G, O'Callaghan C, et al. Primary ciliary dyskinesia: diagnosis and standards of care. Eur Respir J. 1998; 12:982–988.
Article17. el-Sayed Y, al-Sarhani A, al-Essa AR. Otological manifestations of primary ciliary dyskinesia. Clin Otolaryngol Allied Sci. 1997; 22(3):266–270.
Article