Asia Pac Allergy.
2012 Apr;2(2):149-160. 10.5415/apallergy.2012.2.2.149.
Management of chronic urticaria in Asia: 2010 AADV consensus guidelines
- Affiliations
-
- 1The KL Skin Centre, Pantai Hospital Kuala Lumpur, Kuala Lumpur, 59100, Malaysia. drstevenchow@gmail.com
- KMID: 2397369
- DOI: http://doi.org/10.5415/apallergy.2012.2.2.149
Abstract
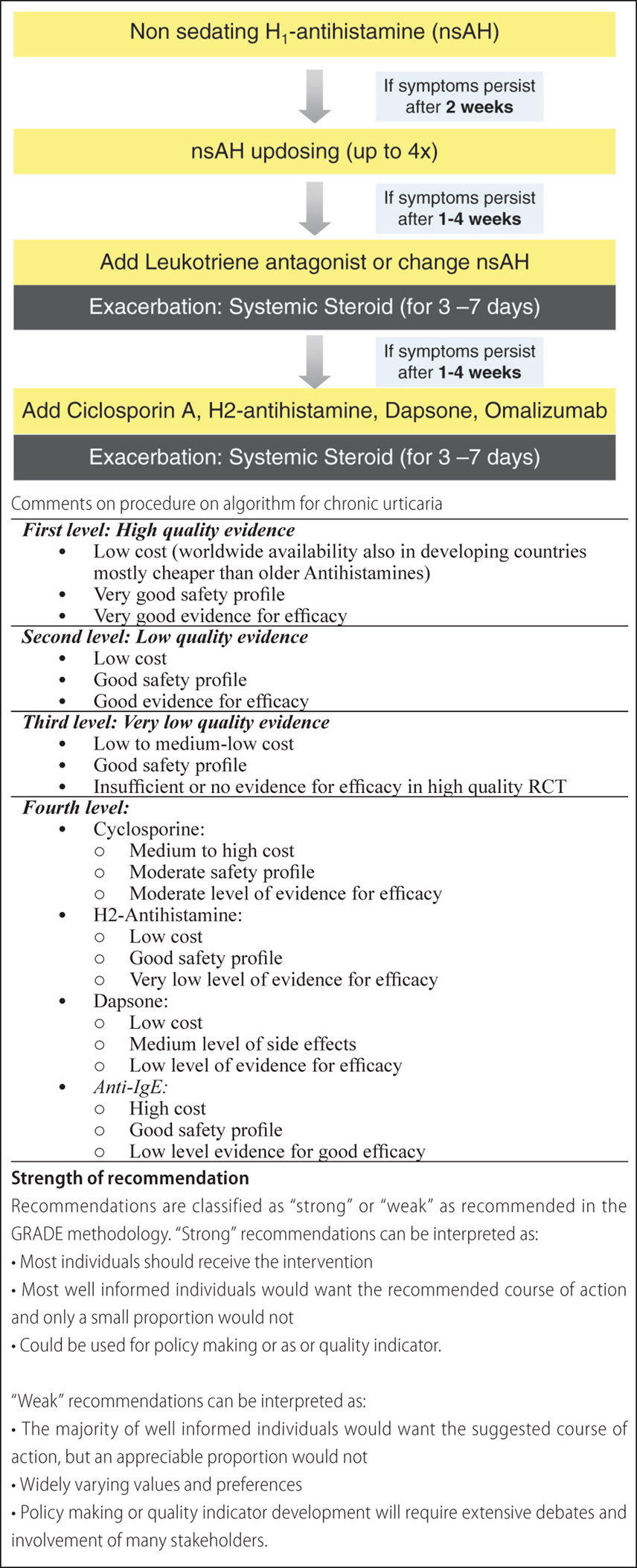
- This guideline is a result of a consensus reached during the 19th Asian-Australasian Regional Conference of Dermatology by the Asian Academy of Dermatology and Venereology Study Group in collaboration with the League of Asian Dermatological Societies in 2010. Urticaria has a profound impact on the quality of life in Asia and the need for effective treatment is required. In line with the EAACI/GA2LEN/EDF/WAO guideline for the management of urticaria the recommended first-line treatment is new generation, non-sedating H1-antihistamines. If standard dosing is ineffective, increasing the dosage up to four-fold is recommended. For patients who do not respond to a four-fold increase in dosage of non-sedating H1-antihistamines, it is recommended that therapies such as H2-antihistamine, leukotriene antagonist, and cyclosporine A should be added to the antihistamine treatment. In the choice of second-line treatment, both their costs and risk/benefit profiles are the most important considerations.
MeSH Terms
Figure
Cited by 3 articles
-
Asia Pacific Allergy: a successful first year and the future
Yoon-Seok Chang
Asia Pac Allergy. 2012;2(2):91-92. doi: 10.5415/apallergy.2012.2.2.91.Role of bilastine in the management of allergic rhinitis and urticaria: an Asia-Pacific consensus statement
Ralph Mösges, Dennis Lip Yen Lee, Jovilia Abong, Bella Siasoco, Steven KW Chow, Jern-Lin Leong, Harvinder Singh, S Kuljit, Benjamin Campomanes
Asia Pac Allergy. 2016;6(1):56-66. doi: 10.5415/apallergy.2016.6.1.56.Chronic urticaria and use of statins
Sujoy Khan
Asia Pac Allergy. 2012;2(3):227-229. doi: 10.5415/apallergy.2012.2.3.227.
Reference
-
1. Zuberbier T, Asero R, Bindslev-Jensen C, Walter Canonica G, Church MK, Giménez-Arnau AM, Grattan CE, Kapp A, Maurer M, Merk HF, Rogala B, Saini S, Sánchez-Borges M, Schmid-Grendelmeier P, Schünemann H, Staubach P, Vena GA, Wedi B. EAACI/GA2LEN/EDF/WAO guideline: management of urticaria. Allergy. 2009. 64:1427–1443.2. Zuberbier T, Greaves MW, Juhlin L, Merk H, Stingl G, Henz BM. Management of urticaria: a consensus report. J Investig Dermatol Symp Proc. 2001. 6:128–131.
Article3. Zuberbier T, Greaves MW, Juhlin L, Kobza-Black A, Maurer D, Stingl G, Henz BM. Definition, classification, and routine diagnosis of urticaria: a consensus report. J Investig Dermatol Symp Proc. 2001. 6:123–127.4. Yadav MK, Rishi JP, Nijawan S. Chronic urticaria and Helicobacter pylori. Indian J Med Sci. 2008. 62:157–162.5. Godse KV. Can worms cause chronic urticaria? Indian J Dermatol. 2006. 51:153–154.
Article6. Yadav S, Upadhyay A, Bajaj AK. Chronic uricaria: an overview. Indian J Dermatol. 2006. 51:171–177.7. Zuberbier T. The role of allergens and pseudoallergens in urticaria. J Investig Dermatol Symp Proc. 2001. 6:132–134.
Article8. Yadav S, Bajaj AK. Management of difficult urticaria. Indian J Dermatol. 2009. 54:275–279.
Article9. Grattan CE, Sabroe RA, Greaves MW. Chronic Urticaria. J Am Acad Dermatol. 2002. 46:645–657.
Article10. Stevenson DD. Aspirin and NSAID sensitivity. Immunol Allergy Clin North Am. 2004. 24:491–505. vii
Article11. Kasperska-Zajac A, Brzoza Z, Rogala B. Sex hormones and urticaria. J Dermatol Sci. 2008. 52:79–86.
Article12. Poole JA, Rosenwasser LJ. Chronic idiopathic urticaria exacerbated with progesterone therapy treated with novel desensitization protocol. J Allergy Clin Immunol. 2004. 114:456–457.13. André F, Veysseyre-Balter C, Rousset H, Descos L, André C. Exogenous oestrogen as an alternative to food allergy in the aetiology of angioneurotic oedema. Toxicology. 2003. 185:155–160.
Article14. Mahesh PA, Kushalappa PA, Holla AD, Vedanthan PK. House dust mite sensitivity is a factor in chronic urticaria. Indian J Dermatol Venereol Leprol. 2005. 71:99–101.
Article15. Stadler BM, Pachlopnik J, Vogel M, Horn M, Dahinden M, Miescher S. Conditional autoantibodies in urticaria patients: a unifying hypothesis. J Investig Dermatol Symp Proc. 2001. 6:150–152.
Article16. Stöckli SS, Bircher AJ. Generalized pruritus in a patient sensitized to tobacco and cannabis. J Dtsch Dermatol Ges. 2007. 5:303–304.
Article17. Plaza T, Nist G, Stetter C, von den Driesch P. Angioedema due to type I allergy to snuff tobacco. J Dtsch Dermatol Ges. 2007. 5:300–302.
Article18. Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surg Am. 2001. 83:428–436.
Article19. Axéll T. Hypersensitivity of the oral mucosa: clinics and pathology. Acta Odontol Scand. 2001. 59:315–319.
Article20. Malhotra SK, Mehta V. Role of stressful life events in induction or exacerbation of psoriasis and chronic urticaria. Indian J Dermatol Venereol Leprol. 2008. 74:594–599.
Article21. Reich A, Wójcik-Maciejewicz A, Slominski AT. Stress and the skin. G Ital Dermatol Venereol. 2010. 145:213–219.22. Yang HY, Sun CC, Wu YC, Wang JD. Stress, insomnia, and chronic idiopathic urticaria--a case-control study. J Formos Med Assoc. 2005. 104:254–263.23. Kulthanan K, Jiamton S, Thumpimukvatana N, Pinkaew S. Chronic idiopathic urticaria: prevalence and clinical course. J Dermatol. 2007. 34:294–301.
Article24. Merk HF. Standard treatment: the role of antihistamines. J Investig Dermatol Symp Proc. 2001. 6:153–156.
Article25. Staevska M, Popov TA, Kralimarkova T, Lazarova C, Kraeva S, Popova D, Church DS, Dimitrov V, Church MK. The effectiveness of levocetirizine and desloratadine in up to 4 times conventional doses in difficult-to-treat urticaria. J Allergy Clin Immunol. 2010. 125:676–682.
Article26. Siebenhaar F, Degener F, Zuberbier T, Martus P, Maurer M. High-dose desloratadine decreases wheal volume and improves cold provocation thresholds compared with standard-dose treatment in patients with acquired cold urticaria: a randomized, placebo-controlled, crossover study. J Allergy Clin Immunol. 2009. 123:672–679.
Article27. Mahesh PA, Pudupakkam VK, Holla AD, Dande T. Effect of warfarin on chronic idiopathic urticaria. Indian J Dermatol Venereol Leprol. 2009. 75:187–189.
Article28. Juhlin L. Alternative treatments for severely affected patients with urticaria. J Investig Dermatol Symp Proc. 2001. 6:157–159.
Article29. Kobza-Black A. Delayed pressure urticaria. J Investig Dermatol Symp Proc. 2001. 6:148–149.
Article30. Stone KD, Prussin C, Metcalfe DD. IgE, mast cells, basophils, and eosinophils. J Allergy Clin Immunol. 2010. 125:S73–S80.
Article31. Church MK, Maurer M, Simons FE, Bindslev-Jensen C, van Cauwenberge P, Bousquet J, Holgate ST, Zuberbier T. Risk of first-generation H1-antihistamines: a GA2LEN position paper. Allergy. 2010. 65:459–466.32. Godse KV. Chronic urticaria and treatment options. Indian J Dermatol. 2009. 54:310–312.
Article33. Goh CL, Tan KT. Chronic autoimmune urticaria: where we stand? Indian J Dermatol. 2009. 54:269–274.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chronic urticaria and use of statins
- Guideline of Chronic Urticaria Beyond
- Role of bilastine in the management of allergic rhinitis and urticaria: an Asia-Pacific consensus statement
- A study of treatment adherence and quality of life among adults with chronic urticaria in Singapore
- Dermographism ( III ): Dermographism in Acute and Chronic Urticaria