Asia Pac Allergy.
2014 Jan;4(1):42-47. 10.5415/apallergy.2014.4.1.42.
Age of onset as a risk factor of renal involvement in Henoch-Schönlein purpura
- Affiliations
-
- 1Division of Allergy-Immunology, Department of Child Health, Faculty of Medicine, Universitas Padjadjaran, Bandung 40161, Indonesia. renighrahani@yahoo.com
- KMID: 2397125
- DOI: http://doi.org/10.5415/apallergy.2014.4.1.42
Abstract
- BACKGROUND
Henoch-Schönlein purpura (HSP) is the most common vasculitis in children, characterized by triad of symptoms; palpable purpura without thrombocytopenia, abdominal pain, and arthritis. Renal involvement often occur in children with HSP. No data on the renal involvement of children with HSP in Indonesia, especially West Java.
OBJECTIVE
To evaluate renal involvement in children with HSP.
METHODS
Retrospective study was conducted in children with HSP in Department of Child Health, Hasan Sadikin Hospital, from 2006 to 2011. Characteristics and clinical manifestations was reviewed from medical record. HSP was diagnosed by American College of Rheumatology 1990 criteria or European League Against Rheumatism/Pediatric Rheumatology International Trials Organization/Pediatric Rheumatology European Society 2008.
RESULTS
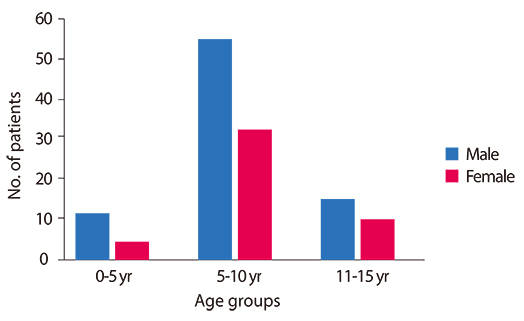
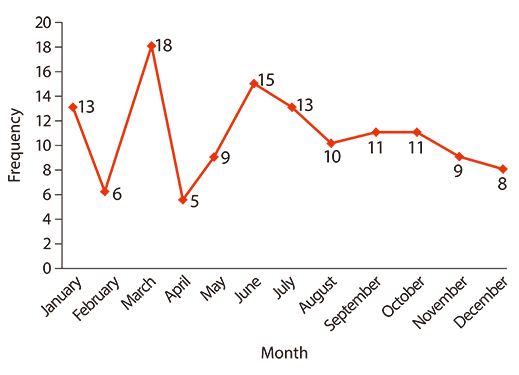
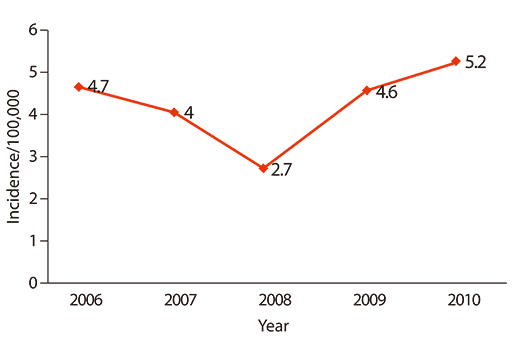
There were 128 patients, consisting of 82 male (64.9%) and 46 female (35.1%) with ratio 1.8:1. Mean age was 7.9 ± 2.9 years old which range from 6 month to 15 years. Peak morbidity was between 5-10 years old. Prevalence of HSP in Hasan Sadikin Hospital tend to raise from 2.7/100,000 in 2008 to 5.2/100,000 in 2010. In most patients (71%) purpura was the first symptom. Seventy-one patients (44.5%) had arthritis and 89 patients (69.5%) had abdominal pain, while renal involvement was in 28 patients (21.8%). Gastrointestinal manifestations tend to manifest in patients less than 5 years old (p = 0.267), while renal involvement tend to manifest in age group 11-15 years old (p = 0.015) with odds ratio 3.1 (95% confidence interval, 1.2-8.1).
CONCLUSION
Renal involvement in children with HSP is more common in age group 11 to 15 years old.
MeSH Terms
Figure
Cited by 2 articles
-
Asia Pacific, and beyond
Yoon-Seok Chang, Sang-Il Lee
Asia Pac Allergy. 2014;4(1):1-2. doi: 10.5415/apallergy.2014.4.1.1.Overview of childhood vasculitis
Jong Gyun Ahn
J Rheum Dis. 2024;31(3):135-142. doi: 10.4078/jrd.2024.0045.
Reference
-
1. Gardner-Medwin JM, Dolezalova P, Cummins C, Southwood TR. Incidence of Henoch-Schönlein purpura, Kawasaki disease, and rare vasculitides in children of different ethnic origins. Lancet. 2002; 360:1197–1202.2. Aalberse J, Dolman K, Ramnath G, Pereira RR, Davin JC. Henoch Schonlein purpura in children: an epidemiological study among Dutch paediatricians on incidence and diagnostic criteria. Ann Rheum Dis. 2007; 66:1648–1650.
Article3. Reamy BV, Williams PM, Lindsay TJ. Henoch-Schönlein purpura. Am Fam Physician. 2009; 80:697–704.4. Lau KK, Suzuki H, Novak J, Wyatt RJ. Pathogenesis of Henoch-Schönlein purpura nephritis. Pediatr Nephrol. 2010; 25:19–26.
Article5. Sinclair P. Henoch-schönlein purpura: a review. Curr Allergy Clin Immunol. 2010; 23:116–120.6. Ozen S, Pistorio A, Iusan SM, Bakkaloglu A, Herlin T, Brik R, Buoncompagni A, Lazar C, Bilge I, Uziel Y, Rigante D, Cantarini L, Hilario MO, Silva CA, Alegria M, Norambuena X, Belot A, Berkun Y, Estrella AI, Olivieri AN, Alpigiani MG, Rumba I, Sztajnbok F, Tambic-Bukovac L, Breda L, Al-Mayouf S, Mihaylova D, Chasnyk V, Sengler C, Klein-Gitelman M, Djeddi D, Nuno L, Pruunsild C, Brunner J, Kondi A, Pagava K, Pederzoli S, Martini A, Ruperto N. Paediatric Rheumatology International Trials Organisation (PRINTO). EULAR/PRINTO/PRES criteria for Henoch-Schönlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008 Part II: Final classification criteria. Ann Rheum Dis. 2010; 69:798–806.7. Trapani S, Micheli A, Grisolia F, Resti M, Chiappini E, Falcini F, De Martino M. Henoch Schonlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005; 35:143–153.
Article8. Peru H, Soylemezoglu O, Bakkaloglu SA, Elmas S, Bozkaya D, Elmaci AM, Kara F, Buyan N, Hasanoglu E. Henoch Schonlein purpura in childhood: clinical analysis of 254 cases over a 3-year period. Clin Rheumatol. 2008; 27:1087–1092.
Article9. Nakaseko H, Uemura O, Nagai T, Yamakawa S, Hibi Y, Yamasaki Y, Yamamoto M. High prevalence of sinusitis in children with henoch-schönlein purpura. Int J Pediatr. 2011; 2011:562638.
Article10. Islek I, Muslu A, Totan M, Gok F, Sanic A. Henoch-Schonlein purpura and pulmonary tuberculosis. Pediatr Int. 2002; 44:545–546.
Article11. Ballinger S. Henoch-Schonlein purpura. Curr Opin Rheumatol. 2003; 15:591–594.
Article12. Davin JC. Henoch-Schonlein purpura nephritis: pathophysiology, treatment, and future strategy. Clin J Am Soc Nephrol. 2011; 6:679–689.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Usefulness of Neutrophil-Lymphocyte Ratio as a Predictor of Henoch–Schönlein Nephritis
- A Case of Henoch-Schönlein Purpura Associated with Mycoplasma Pneumoniae Pneumonia
- A Case of Pulmonary Infarction Probably Related with Henoch-Schönlein Purpura
- Henoch-Schönlein Purpura Presenting as Intussusception
- Henoch-Schönlein Purpura with Concurrent Cytomegalovirus Duodenitis