Changing the paradigm for cough: does 'cough hypersensitivity' aid our understanding?
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul 110-799, Korea.
- 2Institute of Allergy and Clinical Immunology, Seoul National University Medical Research Center, Seoul 110-799, Korea.
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam 463-707, Korea.
- 4Cardiovascular and Respiratory Studies, Castle Hill Hospital, University of Hull, Hull York Medical School, Cottingham HU16 5JQ, UK. a.h.morice@hull.ac.uk
- KMID: 2397119
- DOI: http://doi.org/10.5415/apallergy.2014.4.1.3
Abstract
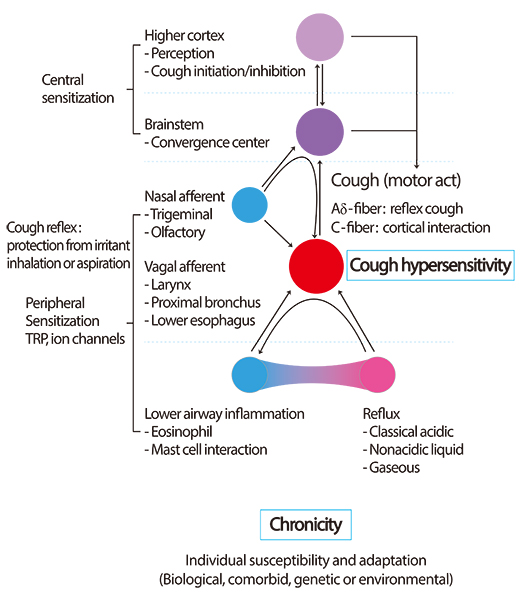
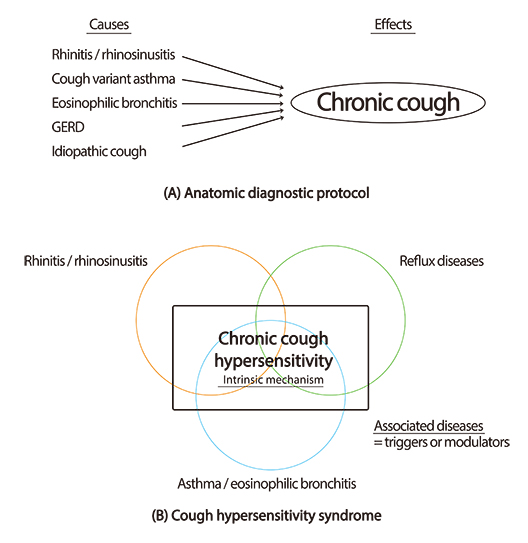
- Chronic cough is a common reason for patients to seek medication attention. Over the last few decades, we have experienced significant clinical success by applying the paradigm of 'evaluating and treating the causes for chronic cough'. However, we still ask ourselves 'what underlies chronic cough. Indeed in a considerable proportion of patients cough is idiopathic, or unexplained despite vigorous evaluation. Commonly associated conditions such as rhinitis, eosinophilic bronchitis, asthma, or gastroesophageal acidic reflux may not be fundamental to cough, and thus may be triggers rather than causes. The cardinal feature of chronic cough is persistent upregulation the cough reflex, which may be driven by complex interactions between biologic, neurologic, immunologic, genetic, comorbid, and environmental factors. We suggest the new paradigm 'cough hypersensitivity syndrome' should finally bring us further advances in understanding and management of chronic cough.
Keyword
MeSH Terms
Figure
Cited by 6 articles
-
Asia Pacific, and beyond
Yoon-Seok Chang, Sang-Il Lee
Asia Pac Allergy. 2014;4(1):1-2. doi: 10.5415/apallergy.2014.4.1.1.Chronic cough: an Asian perspective. Part 1: Epidemiology
Woo-Jung Song, Shoaib Faruqi, Jettanong Klaewsongkram, Seung-Eun Lee, Yoon-Seok Chang
Asia Pac Allergy. 2015;5(3):136-144. doi: 10.5415/apallergy.2015.5.3.136.Greetings from Asia Pacific Allergy
Yoon-Seok Chang
Asia Pac Allergy. 2016;6(4):195-197. doi: 10.5415/apallergy.2016.6.4.195.Chronic cough in Korean adults: a literature review on common comorbidity
Sung-Yoon Kang, Gun-Woo Kim, Woo-Jung Song, Yoon-Seok Chang, Sang-Heon Cho
Asia Pac Allergy. 2016;6(4):198-206. doi: 10.5415/apallergy.2016.6.4.198.KAAACI Evidence-Based Clinical Practice Guidelines for Chronic Cough in Adults and Children in Korea
Dae Jin Song, Woo-Jung Song, Jae-Woo Kwon, Gun-Woo Kim, Mi-Ae Kim, Mi-Yeong Kim, Min-Hye Kim, Sang-Ha Kim, Sang-Heon Kim, Sang Hyuck Kim, Sun-Tae Kim, Sae-Hoon Kim, Ja Kyoung Kim, Joo-Hee Kim, Hyun Jung Kim, Hyo-Bin Kim, Kyung-Hee Park, Jae Kyun Yoon, Byung-Jae Lee, Seung-Eun Lee, Young Mok Lee, Yong Ju Lee, Kyung-Hwan Lim, You Hoon Jeon, Eun-Jung Jo, Young-Koo Jee, Hyun Jung Jin, Sun Hee Choi, Gyu Young Hur, Sang-Heon Cho, Sang-Hoon Kim, Dae Hyun Lim
Allergy Asthma Immunol Res. 2018;10(6):591-613. doi: 10.4168/aair.2018.10.6.591.Cough Hypersensitivity Syndrome: A Few More Steps Forward
Woo-Jung Song, Alyn H. Morice
Allergy Asthma Immunol Res. 2017;9(5):394-402. doi: 10.4168/aair.2017.9.5.394.
Reference
-
1. Voorsanger WC, Firestone F. Etiological factors in chronic cough: an analysis of one hundred cases-preliminary report. Cal West Med. 1927; 26:48–50.2. Brooks SM. Perspective on the human cough reflex. Cough. 2011; 7:10.
Article3. Morice AH. Epidemiology of cough. Pulm Pharmacol Ther. 2002; 15:253–259.
Article4. Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet. 2008; 371:1364–1374.
Article5. Song WJ, Morice AH, Kim MH, Lee SE, Jo EJ, Lee SM, Han JW, Kim TH, Kim SH, Jang HC, Kim KW, Cho SH, Min KU, Chang YS. Cough in the elderly population: relationships with multiple comorbidity. PLoS One. 2013; 8:e78081.
Article6. Birring SS, Prudon B, Carr AJ, Singh SJ, Morgan MD, Pavord ID. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax. 2003; 58:339–343.
Article7. McGarvey L. The difficult-to-treat, therapy-resistant cough: why are current cough treatments not working and what can we do? Pulm Pharmacol Ther. 2013; 26:528–531.
Article8. Phillips AM, Phillips RW, Thompson JL. Chronic cough: analysis of etiologic factors in a survey of 1,274 men. Ann Intern Med. 1956; 45:216–231.
Article9. Irwin RS, Corrao WM, Pratter MR. Chronic persistent cough in the adult: the spectrum and frequency of causes and successful outcome of specific therapy. Am Rev Respir Dis. 1981; 123(4 Pt 1):413–417.10. Irwin RS, Rosen MJ, Braman SS. Cough. A comprehensive review. Arch Intern Med. 1977; 137:1186–1191.
Article11. Morice AH, Fontana GA, Sovijarvi AR, Pistolesi M, Chung KF, Widdicombe J, O'Connell F, Geppetti P, Gronke L, De Jongste J, Belvisi M, Dicpinigaitis P, Fischer A, McGarvey L, Fokkens WJ, Kastelik J. ERS Task Force. The diagnosis and management of chronic cough. Eur Respir J. 2004; 24:481–492.12. McGarvey LP. Does idiopathic cough exist? Lung. 2008; 186:Suppl 1. S78–S81.
Article13. O'Hara J, Jones NS. "Post-nasal drip syndrome": most patients with purulent nasal secretions do not complain of chronic cough. Rhinology. 2006; 44:270–273.14. Jaspersen D, Kulig M, Labenz J, Leodolter A, Lind T, Meyer-Sabellek W, Vieth M, Willich SN, Lindner D, Stolte M, Malfertheiner P. Prevalence of extra-oesophageal manifestations in gastro-oesophageal reflux disease: an analysis based on the ProGERD Study. Aliment Pharmacol Ther. 2003; 17:1515–1520.
Article15. Irwin RS, Madison JM. The diagnosis and treatment of cough. N Engl J Med. 2000; 343:1715–1721.
Article16. Morice AH. The cough hypersensitivity syndrome: a novel paradigm for understanding cough. Lung. 2010; 188:Suppl 1. S87–S90.
Article17. Chung KF. Chronic 'cough hypersensitivity syndrome': a more precise label for chronic cough. Pulm Pharmacol Ther. 2011; 24:267–271.
Article18. Morice AH, McGarvey LP, Dicpinigaitis PV. Cough hypersensitivity syndrome is an important clinical concept: a pro/con debate. Lung. 2012; 190:3–9.
Article19. Dicpinigaitis PV, Fontana GA, Lee LY, Tatar M. Summary of papers presented at the 2012 seventh international cough symposium. Cough. 2013; 9:13.
Article20. Morice AH. Chronic cough hypersensitivity syndrome. Cough. 2013; 9:14.
Article21. Morice AH. Rebuttal: cough is an expiratory sound. Lung. 2008; 186:Suppl 1. S7–S9.
Article22. Mazzone SB, McGovern AE, Yang SK, Woo A, Phipps S, Ando A, Leech J, Farrell MJ. Sensorimotor circuitry involved in the higher brain control of coughing. Cough. 2013; 9:7.
Article23. Grace MS, Dubuis E, Birrell MA, Belvisi MG. Pre-clinical studies in cough research: role of Transient Receptor Potential (TRP) channels. Pulm Pharmacol Ther. 2013; 26:498–507.
Article24. Canning BJ, Mazzone SB, Meeker SN, Mori N, Reynolds SM, Undem BJ. Identification of the tracheal and laryngeal afferent neurones mediating cough in anaesthetized guinea-pigs. J Physiol. 2004; 557(Pt 2):543–558.
Article25. Canning BJ, Mori N, Mazzone SB. Vagal afferent nerves regulating the cough reflex. Respir Physiol Neurobiol. 2006; 152:223–242.
Article26. Morice AH, Geppetti P. Cough. 5: The type 1 vanilloid receptor: a sensory receptor for cough. Thorax. 2004; 59:257–258.27. Birrell MA, Belvisi MG, Grace M, Sadofsky L, Faruqi S, Hele DJ, Maher SA, Freund-Michel V, Morice AH. TRPA1 agonists evoke coughing in guinea pig and human volunteers. Am J Respir Crit Care Med. 2009; 180:1042–1047.
Article28. Canning BJ. Functional implications of the multiple afferent pathways regulating cough. Pulm Pharmacol Ther. 2011; 24:295–299.
Article29. Song WJ, Kim JY, Jo EJ, Lee SE, Kim MH, Yang MS, Kang HR, Park HW, Chang YS, Min KU, Cho SH. Capsaicin cough sensitivity is related to the older female predominant feature in chronic cough patients. Allergy Asthma Immunol Res Forthcoming. 2014.
Article30. Lee LY. Respiratory sensations evoked by activation of bronchopulmonary C-fibers. Respir Physiol Neurobiol. 2009; 167:26–35.
Article31. Davenport PW, Bolser DC, Vickroy T, Berry RB, Martin AD, Hey JA, Danzig M. The effect of codeine on the Urge-to-Cough response to inhaled capsaicin. Pulm Pharmacol Ther. 2007; 20:338–346.
Article32. Hilton EC, Baverel PG, Woodcock A, Van Der Graaf PH, Smith JA. Pharmacodynamic modeling of cough responses to capsaicin inhalation calls into question the utility of the C5 end point. J Allergy Clin Immunol. 2013; 132:847–855. e1–e5.
Article33. Corrao WM, Braman SS, Irwin RS. Chronic cough as the sole presenting manifestation of bronchial asthma. N Engl J Med. 1979; 300:633–637.
Article34. Brightling CE, Ward R, Goh KL, Wardlaw AJ, Pavord ID. Eosinophilic bronchitis is an important cause of chronic cough. Am J Respir Crit Care Med. 1999; 160:406–410.
Article35. Brightling CE, Bradding P, Symon FA, Holgate ST, Wardlaw AJ, Pavord ID. Mast-cell infiltration of airway smooth muscle in asthma. N Engl J Med. 2002; 346:1699–1705.
Article36. Fujimura M, Ogawa H, Yasui M, Matsuda T. Eosinophilic tracheobronchitis and airway cough hypersensitivity in chronic non-productive cough. Clin Exp Allergy. 2000; 30:41–47.
Article37. Birring SS, Parker D, Brightling CE, Bradding P, Wardlaw AJ, Pavord ID. Induced sputum inflammatory mediator concentrations in chronic cough. Am J Respir Crit Care Med. 2004; 169:15–19.
Article38. Ternesten-Hasseus E, Farbrot A, Lowhagen O, Millqvist E. Sensitivity to methacholine and capsaicin in patients with unclear respiratory symptoms. Allergy. 2002; 57:501–507.
Article39. Haldar P, Brightling CE, Hargadon B, Gupta S, Monteiro W, Sousa A, Marshall RP, Bradding P, Green RH, Wardlaw AJ, Pavord ID. Mepolizumab and exacerbations of refractory eosinophilic asthma. N Engl J Med. 2009; 360:973–984.
Article40. Niimi A, Brightling CE, Dicpinigaitis PV. Cough in asthma Is due to eosinophilic airway inflammation: a Pro/Con Debate. Lung. 2013; 12. 14. [Epub]. http://dx.doi.org/10.1007/s00408-013-9543-8.
Article41. Profita M, Sala A, Bonanno A, Riccobono L, Siena L, Melis MR, Di Giorgi R, Mirabella F, Gjomarkaj M, Bonsignore G, Vignola AM. Increased prostaglandin E2 concentrations and cyclooxygenase-2 expression in asthmatic subjects with sputum eosinophilia. J Allergy Clin Immunol. 2003; 112:709–716.
Article42. Grace M, Birrell MA, Dubuis E, Maher SA, Belvisi MG. Transient receptor potential channels mediate the tussive response to prostaglandin E2 and bradykinin. Thorax. 2012; 67:891–900.43. Hwang SW, Cho H, Kwak J, Lee SY, Kang CJ, Jung J, Cho S, Min KH, Suh YG, Kim D, Oh U. Direct activation of capsaicin receptors by products of lipoxygenases: endogenous capsaicin-like substances. Proc Natl Acad Sci U S A. 2000; 97:6155–6160.
Article44. Caceres AI, Brackmann M, Elia MD, Bessac BF, del Camino D, D'Amours M, Witek JS, Fanger CM, Chong JA, Hayward NJ, Homer RJ, Cohn L, Huang X, Moran MM, Jordt SE. A sensory neuronal ion channel essential for airway inflammation and hyperreactivity in asthma. Proc Natl Acad Sci U S A. 2009; 106:9099–9104.
Article45. Hox V, Vanoirbeek JA, Alpizar YA, Voedisch S, Callebaut I, Bobic S, Sharify A, De Vooght V, Van Gerven L, Devos F, Liston A, Voets T, Vennekens R, Bullens DM, De Vries A, Hoet P, Braun A, Ceuppens JL, Talavera K, Nemery B, Hellings PW. Crucial role of transient receptor potential ankyrin 1 and mast cells in induction of nonallergic airway hyperreactivity in mice. Am J Respir Crit Care Med. 2013; 187:486–493.
Article46. Wu Y, You H, Ma P, Li L, Yuan Y, Li J, Ye X, Liu X, Yao H, Chen R, Lai K, Yang X. Role of transient receptor potential ion channels and evoked levels of neuropeptides in a formaldehyde-induced model of asthma in BALB/c mice. PLoS One. 2013; 8:e62827.
Article47. Nassini R, Pedretti P, Moretto N, Fusi C, Carnini C, Facchinetti F, Viscomi AR, Pisano AR, Stokesberry S, Brunmark C, Svitacheva N, McGarvey L, Patacchini R, Damholt AB, Geppetti P, Materazzi S. Transient receptor potential ankyrin 1 channel localized to non-neuronal airway cells promotes non-neurogenic inflammation. PLoS One. 2012; 7:e42454.
Article48. Sadofsky LR, Ramachandran R, Crow C, Cowen M, Compton SJ, Morice AH. Inflammatory stimuli up-regulate transient receptor potential vanilloid-1 expression in human bronchial fibroblasts. Exp Lung Res. 2012; 38:75–81.
Article49. McGarvey LP, Butler CA, Stokesberry S, Polley L, McQuaid S, Abdullah H, Ashraf S, McGahon MK, Curtis TM, Arron J, Choy D, Warke TJ, Bradding P, Ennis M, Zholos A, Costello RW, Heaney LG. Increased expression of bronchial epithelial transient receptor potential vanilloid 1 channels in patients with severe asthma. J Allergy Clin Immunol. 2013; 11. 07. [Epub]. http://dx.doi.org/10.1016/j.jaci.2013.09.016.
Article50. Plevkova J, Song WJ. Chronic cough in subjects with upper airway diseases: analysis of mechanisms and clinical applications. Asia Pac Allergy. 2013; 3:127–135.51. Tatar M, Plevkova J, Brozmanova M, Pecova R, Kollarik M. Mechanisms of the cough associated with rhinosinusitis. Pulm Pharmacol Ther. 2009; 22:121–126.
Article52. Pecova R, Vrlik M, Tatar M. Cough sensitivity in allergic rhinitis. J Physiol Pharmacol. 2005; 56:Suppl 4. 171–178.53. Plevkova J, Poliacek I, Antosiewicz J, Adamkov M, Jakus J, Svirlochova K, Tatar M. Intranasal TRPV1 agonist capsaicin challenge and its effect on c-fos expression in the guinea pig brainstem. Respir Physiol Neurobiol. 2010; 173:11–15.
Article54. Buday T, Brozmanova M, Biringerova Z, Gavliakova S, Poliacek I, Calkovsky V, Shetthalli MV, Plevkova J. Modulation of cough response by sensory inputs from the nose - role of trigeminal TRPA1 versus TRPM8 channels. Cough. 2012; 8:11.
Article55. Weusten BL, Roelofs JM, Akkermans LM, Van Berge-Henegouwen GP, Smout AJ. The symptom-association probability: an improved method for symptom analysis of 24-hour esophageal pH data. Gastroenterology. 1994; 107:1741–1745.
Article56. Patterson N, Mainie I, Rafferty G, McGarvey L, Heaney L, Tutuian R, Castell D, Johnston BT. Nonacid reflux episodes reaching the pharynx are important factors associated with cough. J Clin Gastroenterol. 2009; 43:414–419.
Article57. Faruqi S, Sedman P, Jackson W, Molyneux I, Morice AH. Fundoplication in chronic intractable cough. Cough. 2012; 8:3.
Article58. Zerbib F, Roman S, Bruley Des Varannes S, Gourcerol G, Coffin B, Ropert A, Lepicard P, Mion F. Groupe Francais De Neuro-Gastroenterologie. Normal values of pharyngeal and esophageal 24-hour pH impedance in individuals on and off therapy and interobserver reproducibility. Clin Gastroenterol Hepatol. 2013; 11:366–372.
Article59. Crossfield GL, Jackson W, Burke J, Woodcock AD, Strugala V, Ward C, Pearson JP, Dettmar PW, Morice AH. Pepsin detection despite the use of acid suppressant medication in patients with airway reflux related chronic cough. Thorax. 2013; 68:A19.60. Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI). J Voice. 2002; 16:274–277.
Article61. Morice AH, Faruqi S, Wright CE, Thompson R, Bland JM. Cough hypersensitivity syndrome: a distinct clinical entity. Lung. 2011; 189:73–79.
Article62. Gu Q, Lee LY. Airway irritation and cough evoked by acid: from human to ion channel. Curr Opin Pharmacol. 2011; 11:238–247.
Article63. Kwon NH, Oh MJ, Min TH, Lee BJ, Choi DC. Causes and clinical features of subacute cough. Chest. 2006; 129:1142–1147.
Article64. Dicpinigaitis PV, Bhat R, Rhoton WA, Tibb AS, Negassa A. Effect of viral upper respiratory tract infection on the urge-to-cough sensation. Respir Med. 2011; 105:615–618.
Article65. O'Connell F, Thomas VE, Studham JM, Pride NB, Fuller RW. Capsaicin cough sensitivity increases during upper respiratory infection. Respir Med. 1996; 90:279–286.66. Abdullah H, Heaney LG, Cosby SL, McGarvey LP. Rhinovirus upregulates transient receptor potential channels in a human neuronal cell line: implications for respiratory virus-induced cough reflex sensitivity. Thorax. 2014; 69:46–54.
Article67. Kusel MM, de Klerk NH, Kebadze T, Vohma V, Holt PG, Johnston SL, Sly PD. Early-life respiratory viral infections, atopic sensitization, and risk of subsequent development of persistent asthma. J Allergy Clin Immunol. 2007; 119:1105–1110.
Article68. Morice AH, Jakes AD, Faruqi S, Birring S, McGarvey L, Canning B, Smith JA, Parker S, Chung KF, Lai KF, Mazzone S, Pavord ID, Dicpinigaitis PV. Age and sex distribution of patients presenting to specialist cough clinics [abstract]. In : American Thoracic Society 2013 International Conference; 2013 May 17-22; Philadelphia, USA. New York: American Thoracic Society;2013. p. A1943.69. Visser LE, Stricker BH, van der Velden J, Paes AH, Bakker A. Angiotensin converting enzyme inhibitor associated cough: a population-based case-control study. J Clin Epidemiol. 1995; 48:851–857.
Article70. Morice AH, Lowry R, Brown MJ, Higenbottam T. Angiotensin-converting enzyme and the cough reflex. Lancet. 1987; 2:1116–1118.
Article71. Dicpinigaitis PV. Angiotensin-converting enzyme inhibitor-induced cough: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:1 Suppl. 169S–173S.72. Patberg KW. The female preponderance to cough hypersensitivity syndrome: another clue pointing to the role of TRPV1 in cough. Lung. 2011; 189:257–258.
Article73. Pham TV, Rosen MR. Sex, hormones, and repolarization. Cardiovasc Res. 2002; 53:740–751.
Article74. Yan T, Liu B, Du D, Eisenach JC, Tong C. Estrogen amplifies pain responses to uterine cervical distension in rats by altering transient receptor potential-1 function. Anesth Analg. 2007; 104:1246–1250.
Article75. Chang AB, Phelan PD, Sawyer SM, Del Brocco S, Robertson CF. Cough sensitivity in children with asthma, recurrent cough, and cystic fibrosis. Arch Dis Child. 1997; 77:331–334.
Article76. Varechova S, Plevkova J, Hanacek J, Tatar M. Role of gender and pubertal stage on cough sensitivity in childhood and adolescence. J Physiol Pharmacol. 2008; 59:Suppl 6. 719–726.77. Chung KF, McGarvey L, Mazzone SB. Chronic cough as a neuropathic disorder. Lancet Respir Med. 2013; 1:414–422.
Article78. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL 3rd. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009; 10:447–485.
Article79. Derbyshire SW, Nichols TE, Firestone L, Townsend DW, Jones AK. Gender differences in patterns of cerebral activation during equal experience of painful laser stimulation. J Pain. 2002; 3:401–411.
Article80. Paulson PE, Minoshima S, Morrow TJ, Casey KL. Gender differences in pain perception and patterns of cerebral activation during noxious heat stimulation in humans. Pain. 1998; 76:223–229.
Article81. Moulton EA, Keaser ML, Gullapalli RP, Maitra R, Greenspan JD. Sex differences in the cerebral BOLD signal response to painful heat stimuli. Am J Physiol Regul Integr Comp Physiol. 2006; 291:R257–R267.
Article82. Yarnitsky D. Conditioned pain modulation (the diffuse noxious inhibitory control-like effect): its relevance for acute and chronic pain states. Curr Opin Anaesthesiol. 2010; 23:611–615.
Article83. Philpott H, Gibson P, Thien F. Irritable bowel syndrome - an inflammatory disease involving mast cells. Asia Pac Allergy. 2011; 1:36–42.
Article84. Lovell RM, Ford AC. Effect of gender on prevalence of irritable bowel syndrome in the community: systematic review and meta-analysis. Am J Gastroenterol. 2012; 107:991–1000.
Article85. Ford AC, Forman D, Moayyedi P, Morice AH. Cough in the community: a cross sectional survey and the relationship to gastrointestinal symptoms. Thorax. 2006; 61:975–979.
Article86. Hamdan AL, Jabbour J, Barazi R, Korban Z, Azar ST. Prevalence of laryngopharyngeal reflux disease in patients with diabetes mellitus. J Voice. 2013; 27:495–499.
Article87. Wang X, Pitchumoni CS, Chandrarana K, Shah N. Increased prevalence of symptoms of gastroesophageal reflux diseases in type 2 diabetics with neuropathy. World J Gastroenterol. 2008; 14:709–712.
Article88. Lee JH, McCarty R. Pain threshold in diabetic rats: effects of good versus poor diabetic control. Pain. 1992; 50:231–236.
Article89. Bair MJ, Brizendine EJ, Ackermann RT, Shen C, Kroenke K, Marrero DG. Prevalence of pain and association with quality of life, depression and glycaemic control in patients with diabetes. Diabet Med. 2010; 27:578–584.
Article90. Herbert MS, Varley AL, Andreae SJ, Goodin BR, Bradley LA, Safford MM. Association of pain with HbA1c in a predominantly black population of community-dwelling adults with diabetes: a cross-sectional analysis. Diabet Med. 2013; 30:1466–1471.91. Smit LA, Kogevinas M, Anto JM, Bouzigon E, Gonzalez JR, Le Moual N, Kromhout H, Carsin AE, Pin I, Jarvis D, Vermeulen R, Janson C, Heinrich J, Gut I, Lathrop M, Valverde MA, Demenais F, Kauffmann F. Transient receptor potential genes, smoking, occupational exposures and cough in adults. Respir Res. 2012; 13:26.
Article92. Park HK, Oh SY, Kim TB, Bahn JW, Shin ES, Lee JE, Oh HB, Kim YK, Park T, Cho SH, Min KU, Kim YY. Association of genetic variations in neurokinin-2 receptor with enhanced cough sensitivity to capsaicin in chronic cough. Thorax. 2006; 61:1070–1075.
Article93. Morjaria JB, Dickinson RS, Morice AH. Novel antitussive strategies. Drug Discov Today. 2013; 18:380–388.
Article94. Morice AH, Menon MS, Mulrennan SA, Everett CF, Wright C, Jackson J, Thompson R. Opiate therapy in chronic cough. Am J Respir Crit Care Med. 2007; 175:312–315.
Article95. Ryan NM, Birring SS, Gibson PG. Gabapentin for refractory chronic cough: a randomised, double-blind, placebo-controlled trial. Lancet. 2012; 380:1583–1589.
Article96. Smith JA, Murdoch RD, Newlands A, Smart K, Khalid S, Kelsall A, Holt K, Dockry R, Woodcock A. The impact of a selective oral TRPV1 antagonist in patients with chronic cough. Thorax. 2012; 67:A128.97. Abdulqawi R, Dockry R, Holt K, Woodcock A, Layton G, McCarthy B, Ford A, Smith J. Inhibition of ATP-gated P2X3 channels by AF-219: An effective anti-tussive mechanism in chronic cough [oral presentation]. In : Annual Cogress Barcelona 2013; 2013 Sep 7-11; Barcelona, Spain. Lausanne (CH): European Respiratory Society;2013.98. Ford AP. In pursuit of P2X3 antagonists: novel therapeutics for chronic pain and afferent sensitization. Purinergic Signal. 2012; 8:Suppl 1. 3–26.
Article