Int J Thyroidol.
2017 Nov;10(2):96-101. 10.11106/ijt.2017.10.2.96.
Clinical Characteristics and Prognosis of Differentiated Thyroid Carcinoma with Small Foci of Anaplastic Transformation
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- 2Department of Pathology, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. yjparkmd@snu.ac.kr
- KMID: 2396813
- DOI: http://doi.org/10.11106/ijt.2017.10.2.96
Abstract
- BACKGROUND AND OBJECTIVES
Anaplastic thyroid carcinoma (ATC) is commonly related with concurrent differentiated thyroid carcinoma (DTC). We aimed to examine the clinicopathologic characteristics, prognosis and gene expression of DTC with anaplastic foci.
MATERIALS AND METHODS
Eighteen patients with DTC with anaplastic foci were enrolled in this study. To compare the clinicopathologic characteristics and prognosis of anaplastic foci subjects with conventional ATC or DTC, we additionally included 12 ATC and 1030 DTC patients who diagnosed during same period. Immunohistochemistry was performed to check the gene expression in anaplastic foci and DTC component.
RESULTS
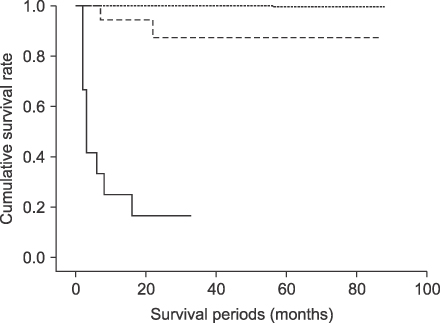
In anaplastic foci group, tumor size was larger (2.5±1.3 vs. 1.2±0.9 cm, p=0.001), distant metastasis was more frequent (11.1 vs. 0%, p=0.000) and 1-year survival rate was low (88.9 vs. 100%, p=0.000) than DTC group. In contrast, compared with ATC group, anaplastic foci group showed younger age at diagnosis (50±16 vs. 63±18 years, p=0.039), smaller tumor size (2.5±1.3 vs. 3.8±1.4 cm, p=0.027), less distant metastasis (11.1 vs. 41.7%, p=0.084) and longer 1-year survival rate (88.9 vs. 25.0%, p=0.001). Expression of p53 protein was observed in 100% of anaplastic foci, ATC and 12.5% of papillary thyroid carcinoma component.
CONCLUSION
DTC with foci of anaplastic transformation has a worse prognosis than DTC, but a better prognosis than ATC. Our results support that DTC with anaplastic foci was intermediate state from DTC to ATC.
MeSH Terms
Figure
Reference
-
1. Pasieka JL. Anaplastic thyroid cancer. Curr Opin Oncol. 2003; 15(1):78–83.
Article2. Haigh PI, Ituarte PH, Wu HS, Treseler PA, Posner MD, Quivey JM, et al. Completely resected anaplastic thyroid carcinoma combined with adjuvant chemotherapy and irradiation is associated with prolonged survival. Cancer. 2001; 91(12):2335–2342.
Article3. Kim TY, Kim KW, Jung TS, Kim JM, Kim SW, Chung KW, et al. Prognostic factors for Korean patients with anaplastic thyroid carcinoma. Head Neck. 2007; 29(8):765–772.
Article4. Sugitani I, Miyauchi A, Sugino K, Okamoto T, Yoshida A, Suzuki S. Prognostic factors and treatment outcomes for anaplastic thyroid carcinoma: ATC Research Consortium of Japan cohort study of 677 patients. World J Surg. 2012; 36(6):1247–1254.
Article5. Spires JR, Schwartz MR, Miller RH. Anaplastic thyroid carcinoma. Association with differentiated thyroid cancer. Arch Otolaryngol Head Neck Surg. 1988; 114(1):40–44.
Article6. Hunt JL, Tometsko M, LiVolsi VA, Swalsky P, Finkelstein SD, Barnes EL. Molecular evidence of anaplastic transformation in coexisting well-differentiated and anaplastic carcinomas of the thyroid. Am J Surg Pathol. 2003; 27(12):1559–1564.
Article7. Tan RK, Finley RK 3rd, Driscoll D, Bakamjian V, Hicks WL Jr, Shedd DP. Anaplastic carcinoma of the thyroid: a 24-year experience. Head Neck. 1995; 17(1):41–47. discussion 47-8.
Article8. McIver B, Hay ID, Giuffrida DF, Dvorak CE, Grant CS, Thompson GB, et al. Anaplastic thyroid carcinoma: a 50-year experience at a single institution. Surgery. 2001; 130(6):1028–1034.
Article9. Wiseman SM, Griffith OL, Deen S, Rajput A, Masoudi H, Gilks B, et al. Identification of molecular markers altered during transformation of differentiated into anaplastic thyroid carcinoma. Arch Surg. 2007; 142(8):717–727. discussion 727-9.
Article10. Albores-Saavedra J, Henson DE, Glazer E, Schwartz AM. Changing patterns in the incidence and survival of thyroid cancer with follicular phenotype--papillary, follicular, and anaplastic: a morphological and epidemiological study. Endocr Pathol. 2007; 18(1):1–7.
Article11. Han JM, Bae Kim W, Kim TY, Ryu JS, Gong G, Hong SJ, et al. Time trend in tumour size and characteristics of anaplastic thyroid carcinoma. Clin Endocrinol (Oxf). 2012; 77(3):459–464.
Article12. Wiseman SM, Loree TR, Hicks WL Jr, Rigual NR, Winston JS, Tan D, et al. Anaplastic thyroid cancer evolved from papillary carcinoma: demonstration of anaplastic transformation by means of the inter-simple sequence repeat polymerase chain reaction. Arch Otolaryngol Head Neck Surg. 2003; 129(1):96–100.
Article13. Sugitani I, Kasai N, Fujimoto Y, Yanagisawa A. Prognostic factors and therapeutic strategy for anaplastic carcinoma of the thyroid. World J Surg. 2001; 25(5):617–622.
Article14. Ibanez ML, Russell WO, Albores-Saavedra J, Lampertico P, White EC, Clark RL. Thyroid carcinoma--biologic behavior and mortality. Postmortem findings in 42 cases, including 27 in which the disease was fatal. Cancer. 1966; 19(8):1039–1052.
Article15. Xing M. BRAF mutation in thyroid cancer. Endocr Relat Cancer. 2005; 12(2):245–262.
Article16. Quiros RM, Ding HG, Gattuso P, Prinz RA, Xu X. Evidence that one subset of anaplastic thyroid carcinomas are derived from papillary carcinomas due to BRAF and p53 mutations. Cancer. 2005; 103(11):2261–2268.
Article17. Nikiforova MN, Kimura ET, Gandhi M, Biddinger PW, Knauf JA, Basolo F, et al. BRAF mutations in thyroid tumors are restricted to papillary carcinomas and anaplastic or poorly differentiated carcinomas arising from papillary carcinomas. J Clin Endocrinol Metab. 2003; 88(11):5399–5404.
Article18. Nilsson O, Lindeberg J, Zedenius J, Ekman E, Tennvall J, Blomgren H, et al. Anaplastic giant cell carcinoma of the thyroid gland: treatment and survival over a 25-year period. World J Surg. 1998; 22(7):725–730.
Article19. Sugino K, Ito K, Mimura T, Nagahama M, Fukunari N, Kubo A, et al. The important role of operations in the management of anaplastic thyroid carcinoma. Surgery. 2002; 131(3):245–248.
Article20. Neff RL, Farrar WB, Kloos RT, Burman KD. Anaplastic thyroid cancer. Endocrinol Metab Clin North Am. 2008; 37(2):525–538, xi.
Article21. O'Neill JP, Power D, Condron C, Bouchier-Hayes D, Walsh M. Anaplastic thyroid cancer, tumorigenesis and therapy. Ir J Med Sci. 2010; 179(1):9–15.22. Smallridge RC, Ain KB, Asa SL, Bible KC, Brierley JD, Burman KD, et al. American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid. 2012; 22(11):1104–1139.
Article23. Lee DY, Won JK, Lee SH, Park DJ, Jung KC, Sung MW, et al. Changes of clinicopathologic characteristics and survival outcomes of anaplastic and poorly differentiated thyroid carcinoma. Thyroid. 2016; 26(3):404–413.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anaplastic Transformation of Papillary Thyroid Carcinoma in a Young Man: A Case Study with Immunohistochemical and BRAF Analysis
- Anaplastic Transformation of Follicular Thyroid Cancer in the Lung, Liver, Bone, and Adrenal Gland
- Anaplastic Transformation of Metastatic Papillary Thyroid Carcinomas in the Cervical Lymph Nodes: Report of 3 Cases
- Coexistent Papillary Thyroid Carcinoma and Its Anaplastic Transformation in Cervical Lymph Node Metastasis
- Importance of Regular Follow-Up Examination during Active Surveillance: a Case of Anaplastic Transformation of Papillary Thyroid Microcarcinoma