Brain Tumor Res Treat.
2017 Oct;5(2):116-119. 10.14791/btrt.2017.5.2.116.
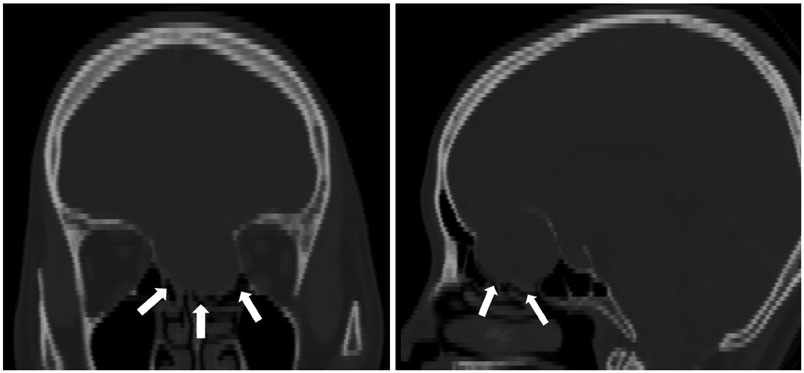
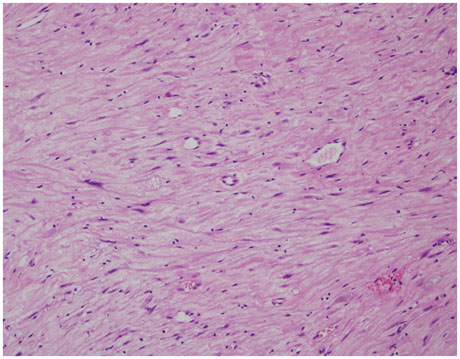
Subfrontal Schwannoma Extended Broadly to Nasal Cavity Treated by Gamma Knife Radiosurgery Following Surgical Excision: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University Hospital, Busan, Korea. chwachoi@pusan.ac.kr
- 2Department of Neurosurgery, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2396457
- DOI: http://doi.org/10.14791/btrt.2017.5.2.116
Abstract
- Subfrontal schwannomas are rarely reported. They are usually found only in the subfrontal area, but some extend to the nasal cavity. In these cases, prevention of postoperative cerebrospinal fluid (CSF) leakage through thinned or eroded anterior skull base is important. A 51-year-old female with anosmia and mild nausea was diagnosed as subfrontal extraaxial mass with nasal cavity extension. This mass was initially thought to be an olfactory groove meningioma. We performed a bifrontal craniotomy for surgical excision. We did not totally remove the tumor, as we wanted to prevent a skull base defect. The histopathological diagnosis was a schwannoma. There was no postoperative complication such as CSF leakage. The residual tumor was treated with gamma knife radiosurgery. The nasal cavity mass has not grown as of five years after radiosurgery.
MeSH Terms
Figure
Reference
-
1. Kim DY, Yoon PH, Kie JH, Yang KH. The olfactory groove schwannoma attached to the cribriform plate: a case report. Brain Tumor Res Treat. 2015; 3:56–59.
Article2. Kanaan HA, Gardner PA, Yeaney G, et al. Expanded endoscopic endonasal resection of an olfactory schwannoma. J Neurosurg Pediatr. 2008; 2:261–265.
Article3. Bezircioğlu H, Sucu HK, Rezanko T, Minoğlu M. Nasal-subfrontal giant schwannoma. Turk Neurosurg. 2008; 18:412–414.4. Amador AR, Santonja C, Del Pozo JM, Ortiz L. Olfactory schwannoma. Eur Radiol. 2002; 12:742–744.
Article5. Choi YS, Sung KS, Song YJ, Kim HD. Olfactory schwannoma-case report. J Korean Neurosurg Soc. 2009; 45:103–106.
Article6. Liu JK, Eloy JA. Expanded endoscopic endonasal transcribriform approach for resection of anterior skull base olfactory schwannoma. Neurosurg Focus. 2012; 32:Suppl 1. E3.
Article7. Elsharkawy M, Xu Z, Schlesinger D, Sheehan JP. Gamma Knife surgery for nonvestibular schwannomas: radiological and clinical outcomes. J Neurosurg. 2012; 116:66–72.
Article8. Puataweepong P, Dhanachai M, Hansasuta A, et al. Clinical outcomes of intracranial nonvestibular schwannomas treated with linac-based stereotactic radiosurgery and radiotherapy. Asian Pac J Cancer Prev. 2016; 17:3271–3276.9. Yamahata H, Hirahara K, Tomosugi T, et al. Subfrontal schwannoma mimicking neuroblastoma: case report. Skull Base Rep. 2011; 1:59–64.
Article10. Adachi K, Yoshida K, Miwa T, Ikeda E, Kawase T. Olfactory schwannoma. Acta Neurochir (Wien). 2007; 149:605–610.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Normal pressure hydrocephalus after gamma knife radiosurgery in a patient with vestibular schwannoma
- A Case of Schwannoma in Subfrontal Area and Nasal Cavity
- Postoperative Residual Juvenile Nasopharyngeal Angiofibroma Treated with Gamma Knife Surgery
- How to use Leksell GammaPlan
- Hearing Preservation, Facial Nerve Dysfunction, and Tumor Control in Small Vestibular Schwannoma: A Systematic Review of Gamma Knife Radiosurgery Versus Microsurgery