Korean J Pain.
2017 Oct;30(4):287-295. 10.3344/kjp.2017.30.4.287.
State of education regarding ultrasound-guided interventions during pain fellowships in Korea: a survey of recent fellows
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Presbyterian Hospital, Jeonju, Korea.
- 2Department of Anesthesiology and Pain Medicine, Kyungpook National University Medical Center, School of Medicine, Kyungpook National University, Daegu, Korea.
- 3Department of Anesthesiology and Pain Medicine, Pusan National University Yangsan Hospital, School of Medicine, Pusan National University, Yangsan, Korea.
- 4Mac Pain Clinic, Seoul, Korea.
- 5Department of Anesthesiology and Pain Medicine, Samsung Medical Center, School of Medicine, Sungkyunkwan University, Seoul, Korea.
- 6Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 7Department of Anesthesiology and Pain Medicine, Ajou University Hospital, Suwon, Korea.
- 8Department of Anesthesiology and Pain Medicine, Keimyung University Dongsan Medical Center, School of Medicine, Keimyung University, Daegu, Korea.
- 9Department of Anesthesiology and Pain Medicine, Wonkwang University Hospital, School of Medicine, Wonkwang University, Wonkwang Institute of Scinece, Iksan, Korea. kydpain@hanmail.net
- 10Committee on Ultrasound in Pain Medicine, Korean Pain Society, Seoul, Korea.
- KMID: 2392906
- DOI: http://doi.org/10.3344/kjp.2017.30.4.287
Abstract
- BACKGROUND
Recently, the use of ultrasound (US) techniques in regional anesthesia and pain medicine has increased significantly. However, the current extent of training in the use of US-guided pain management procedures in Korea remains unknown. The purpose of the present study was to assess the current state of US training provided during Korean Pain Society (KPS) pain fellowship programs through the comparative analysis between training hospitals.
METHODS
We conducted an anonymous survey of 51 pain physicians who had completed KPS fellowships in 2017. Items pertained to current US practices and education, as well as the types of techniques and amount of experience with US-guided pain management procedures. Responses were compared based on the tier of the training hospital.
RESULTS
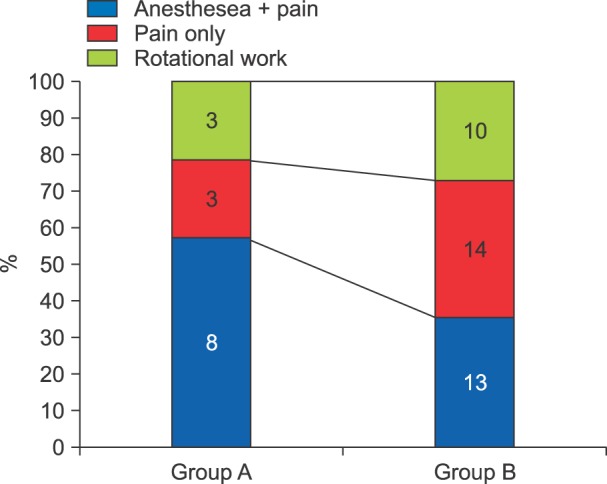
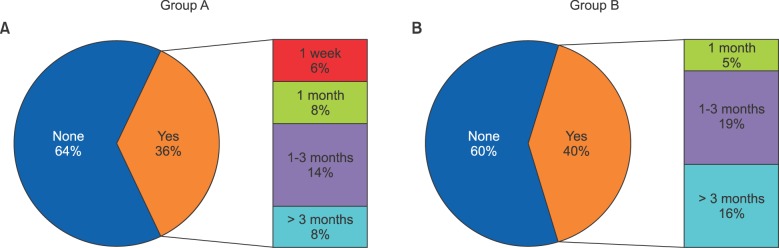
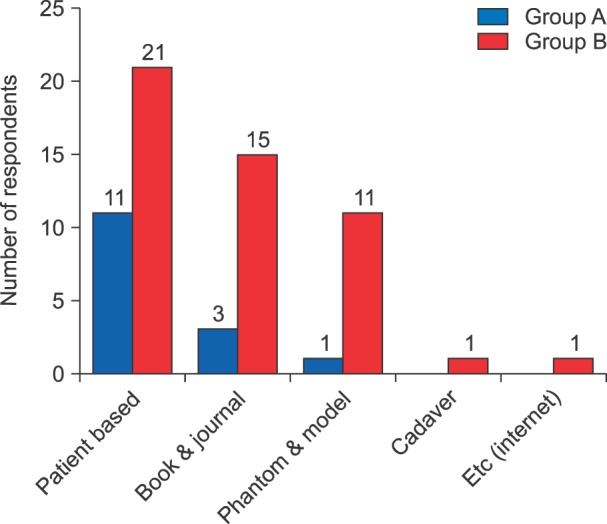
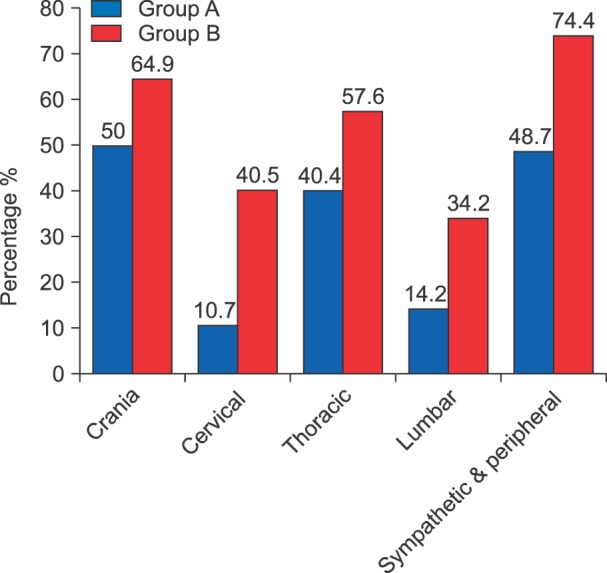
Among the 51 respondents, 14 received training at first- and second-tier hospitals (Group A), while 37 received training at third-tier hospitals (Group B). The mean total duration of pain training during the 1-year fellowship was 7.4 months in Group A and 8.4 months in Group B. Our analysis revealed that 36% and 40% of respondents in Groups A and B received dedicated US training, respectively. Most respondents underwent US training in patient-care settings under the supervision of attending physicians. Cervical root, stellate ganglion, piriformis, and lumbar plexus blocks were more commonly performed by Group B than by Group A (P < 0.05).
CONCLUSIONS
Instruction regarding US-guided pain management interventions varied among fellowship training hospitals, highlighting the need for the development of educational standards that mandate a minimum number of US-guided nerve blocks or injections during fellowships in interventional pain management.
Keyword
MeSH Terms
Figure
Reference
-
1. Jeon YH. Easier and safer regional anesthesia and peripheral nerve block under ultrasound guidance. Korean J Pain. 2016; 29:1–2. PMID: 26839663.
Article2. Conway JA, Adhikary SD, Giampetro D, Stolzenberg D. A survey of ultrasound training in US and Canadian chronic pain fellowship programs. Pain Med. 2015; 16:1923–1929. PMID: 26095214.
Article3. Asaad BO, Reinsel RA, DeVeaux E, Moten H, Durkin B. A survey on teaching ultrasound-guided chronic pain procedures in pain medicine fellowship programs. Pain Physician. 2014; 17:E681–E689. PMID: 25415783.4. Shin SM. Prevalence and trends of pain associated with chronic diseases and personal out-of-pocket medical expenditures in Korea. Korean J Pain. 2017; 30:142–150. PMID: 28416998.
Article5. Hopkins PM. Ultrasound guidance as a gold standard in regional anaesthesia. Br J Anaesth. 2007; 98:299–301. PMID: 17307777.
Article6. Bhatia A, Brull R. Review article: is ultrasound guidance advantageous for interventional pain management? A systematic review of chronic pain outcomes. Anesth Analg. 2013; 117:236–251. PMID: 23592606.
Article7. Choi S, Brull R. Is ultrasound guidance advantageous for interventional pain management? A review of acute pain outcomes. Anesth Analg. 2011; 113:596–604. PMID: 21642604.
Article8. Gelfand HJ, Ouanes JP, Lesley MR, Ko PS, Murphy JD, Sumida SM, et al. Analgesic efficacy of ultrasound-guided regional anesthesia: a meta-analysis. J Clin Anesth. 2011; 23:90–96. PMID: 21377070.
Article9. Chin KJ, Chan V. Ultrasound-guided peripheral nerve blockade. Curr Opin Anaesthesiol. 2008; 21:624–631. PMID: 18784490.
Article10. Abrahams MS, Aziz MF, Fu RF, Horn JL. Ultrasound guidance compared with electrical neurostimulation for peripheral nerve block: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2009; 102:408–417. PMID: 19174373.
Article11. Sites BD, Beach ML, Chinn CD, Redborg KE, Gallagher JD. A comparison of sensory and motor loss after a femoral nerve block conducted with ultrasound versus ultrasound and nerve stimulation. Reg Anesth Pain Med. 2009; 34:508–513. PMID: 19920428.
Article12. Assmann N, McCartney CJ, Tumber PS, Chan VW. Ultrasound guidance for brachial plexus localization and catheter insertion after complete forearm amputation. Reg Anesth Pain Med. 2007; 32:93.
Article13. Ferraro LH, Tardelli MA, Yamashita AM, Cardone JD, Kishi JM. Ultrasound-guided femoral and sciatic nerve blocks in an anticoagulated patient. Case reports. Rev Bras Anestesiol. 2010; 60:422–428. PMID: 20659615.
Article14. Narouze SN. Ultrasound-guided interventional procedures in pain management: evidence-based medicine. Reg Anesth Pain Med. 2010; 35:S55–S58. PMID: 20216026.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-guided interventions for spinal pain
- Ultrasound Guided Therapeutic Medial Branch Block for the Facet Joint Pain
- Endoscopic ultrasound-guided vascular interventions: An overview of current and emerging techniques
- Ultrasound-Guided Intervention in Thoracic Spine
- Ultrasound-guided interventions for controlling the thoracic spine and chest wall pain: a narrative review