Seasonal Patterns of Asthma in Children and Adolescents Presenting at Emergency Departments in Korea
- Affiliations
-
- 1Department of Pediatrics, National Medical Center, Seoul, Korea. ehchung@nmc.or.kr
- 2Department of Pediatrics, Sun General Hospital, Daejeon, Korea.
- KMID: 2391042
- DOI: http://doi.org/10.4168/aair.2016.8.3.223
Abstract
- PURPOSE
Seasonal variations in asthma-related hospitalizations and emergency department visits have long been recognized. This study aimed to investigate the seasonal patterns of asthma in children and adolescents who presented at emergency departments in Korea.
METHODS
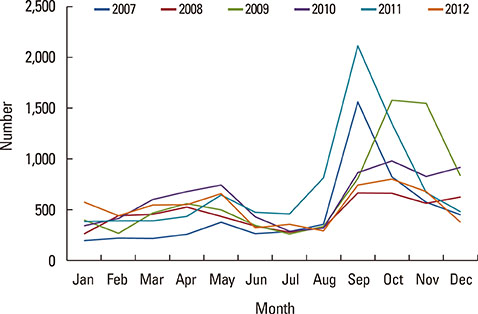
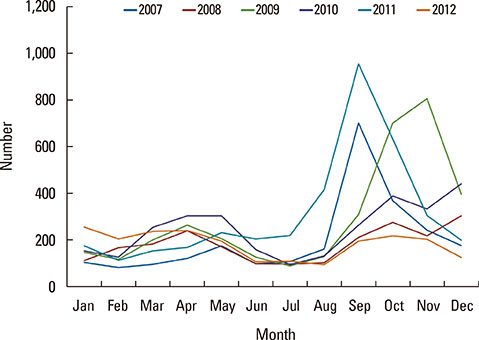
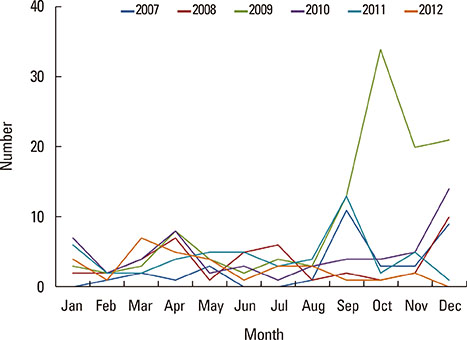
We analyzed the National Emergency Department Information System records from 117 emergency departments in Korea that comprised all of the patients with asthma who were aged 3-18 years and who presented at the emergency departments from 2007 to 2012. The children and adolescents were divided into 3 groups based on their ages, namely, 3-6 years, 7-12 years, and 13-18 years. The data were tabulated, and graphs were created to show the seasonal trends in the monthly numbers of emergency department visits as a consequence of asthma.
RESULTS
A total of 41,128 subjects were identified, and the male-to-female ratio was 1:0.5. General ward admissions comprised 42.6% (n=17,524 patients) of the emergency department visits, and intensive care unit admissions comprised 0.8% (n=335 patients) of the emergency department visits. The monthly numbers of emergency department visits for asthma varied according to the season, with high peaks during fall, which was from September to November, and low levels in summer, which was from June to August.
CONCLUSIONS
Important differences in the seasonal patterns of emergency department visits for asthma were evident in children and adolescents. Identifying seasonal trends in asthma-related emergency department visits may help determine the causes and reduce the likelihood of asthma exacerbation.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Dyspnea Perception During Induced Bronchoconstriction Is Complicated by the Inhaled Methacholine in Children With Clinical Asthma
Yun Jung Choi, Dong In Suh, Myung Hyun Sohn, Young Yull Koh
Allergy Asthma Immunol Res. 2018;10(2):131-136. doi: 10.4168/aair.2018.10.2.131.Therapeutic Effect of Omalizumab in Severe Asthma: A Real-World Study in Korea
Ji-Ho Lee, Hyun Young Lee, Chang-Gyu Jung, Ga-Young Ban, Yoo Seob Shin, Young-Min Ye, Dong-Ho Nahm, Hae-Sim Park
Allergy Asthma Immunol Res. 2018;10(2):121-130. doi: 10.4168/aair.2018.10.2.121.Seasonal Cycle and Relationship of Seasonal Rhino- and Influenza Virus Epidemics With Episodes of Asthma Exacerbation in Different Age Groups
Seung Won Lee, Shinhae Lee, Youn Ho Sheen, Eun Kyo Ha, Sun Hee Choi, Min-Suk Yang, Sohyun Hwang, Sung Soon Kim, Jang-Hoon Choi, Man Yong Han
Allergy Asthma Immunol Res. 2017;9(6):517-525. doi: 10.4168/aair.2017.9.6.517.
Reference
-
1. Busse WW, Lemanske RF Jr. Asthma. N Engl J Med. 2001; 344:350–362.2. Kimes D, Ullah A, Levine E, Nelson R, Timmins S, Weiss S, et al. Relationships between pediatric asthma and socioeconomic/urban variables in Baltimore, Maryland. Health Place. 2004; 10:141–152.3. Kimbell-Dunn M, Pearce N, Beasley R. Seasonal variation in asthma hospitalizations and death rates in New Zealand. Respirology. 2000; 5:241–246.4. Fleming DM, Cross KW, Sunderland R, Ross AM. Comparison of the seasonal patterns of asthma identified in general practitioner episodes, hospital admissions, and deaths. Thorax. 2000; 55:662–665.5. Kimes D, Levine E, Timmins S, Weiss SR, Bollinger ME, Blaisdell C. Temporal dynamics of emergency department and hospital admissions of pediatric asthmatics. Environ Res. 2004; 94:7–17.6. Harju T, Keistinen T, Tuuponen T, Kivelä SL. Seasonal variation in childhood asthma hospitalisations in Finland, 1972-1992. Eur J Pediatr. 1997; 156:436–439.7. Masoli M, Fabian D, Holt S, Beasley R. Global Initiative for Asthma (GINA) Program. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004; 59:469–478.8. Ivey MA, Simeon DT, Monteil MA. Climatic variables are associated with seasonal acute asthma admissions to accident and emergency room facilities in Trinidad, West Indies. Clin Exp Allergy. 2003; 33:1526–1530.9. Hashimoto M, Fukuda T, Shimizu T, Watanabe S, Watanuki S, Eto Y, et al. Influence of climate factors on emergency visits for childhood asthma attack. Pediatr Int. 2004; 46:48–52.10. Sears MR. Epidemiology of asthma exacerbations. J Allergy Clin Immunol. 2008; 122:662–668.11. Johnston NW, Sears MR. Asthma exacerbations. 1: epidemiology. Thorax. 2006; 61:722–728.12. Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980-2007. Pediatrics. 2009; 123:Suppl 3. S131–S145.13. Fagan JK, Scheff PA, Hryhorczuk D, Ramakrishnan V, Ross M, Persky V. Prevalence of asthma and other allergic diseases in an adolescent population: association with gender and race. Ann Allergy Asthma Immunol. 2001; 86:177–184.14. Brooks LJ, Byard PJ, Helms RC, Fouke JM, Strohl KP. Relationship between lung volume and tracheal area as assessed by acoustic reflection. J Appl Physiol (1985). 1988; 64:1050–1054.15. Chen Y, Stewart P, Johansen H, McRae L, Taylor G. Sex difference in hospitalization due to asthma in relation to age. J Clin Epidemiol. 2003; 56:180–187.16. Troisi RJ, Speizer FE, Willett WC, Trichopoulos D, Rosner B. Menopause, postmenopausal estrogen preparations, and the risk of adult-onset asthma. A prospective cohort study. Am J Respir Crit Care Med. 1995; 152:1183–1188.17. Ahn K, Kim J, Kwon HJ, Chae Y, Hahm MI, Lee KJ, et al. The prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in Korean children: nationwide cross-sectional survey using complex sampling design. J Korean Med Assoc. 2011; 54:769–778.18. Statistics Korea. Sex ratio of age groups [Internet]. Daejeon: Statistics Korea;2015. cited 2015 Aug 1. Available from: http://www.index.go.kr/potal/stts/idxMain/selectPoSttsIdxSearch.do?idx_cd=2917&clas_div=&idx_sys_cd=544&idx_clas_cd=1.19. Taussig LM, Wright AL, Holberg CJ, Halonen M, Morgan WJ, Martinez FD. Tucson children's respiratory study: 1980 to present. J Allergy Clin Immunol. 2003; 111:661–675.20. Tan WC. Viruses in asthma exacerbations. Curr Opin Pulm Med. 2005; 11:21–26.21. Khetsuriani N, Kazerouni NN, Erdman DD, Lu X, Redd SC, Anderson LJ, et al. Prevalence of viral respiratory tract infections in children with asthma. J Allergy Clin Immunol. 2007; 119:314–321.22. Johnston SL, Pattemore PK, Sanderson G, Smith S, Campbell MJ, Josephs LK, et al. The relationship between upper respiratory infections and hospital admissions for asthma: a time-trend analysis. Am J Respir Crit Care Med. 1996; 154:654–660.23. Miller EK, Williams JV. Rhinoviruses. In : Kliegman RM, Stanton BF, St Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia (PA): Elsevier/Saunders;2011. p. 1133–1134.24. Korean Centers for Disease Control and Prevention. The prevalence of the respiratory viruses in the patients with acute respiratory infections, 2012 [Internet]. Cheongwon: Korean Centers for Disease Control and Prevention;2013. cited 2015 Aug 1. Available from: http://www.cdc.go.kr/CDC/info/CdcKrInfo0301.jsp?menuIds=HOME001-MNU1132-MNU1138-MNU0037-MNU1380&fid=31&q_type=title&q_value=%EB%B0%94%EC%9D%B4%EB%9F%AC%EC%8A%A4&cid=21323&pageNum=1.25. Korean Centers for Disease Control and Prevention. Weakly occurrence of acute respiratory tract infection with 8 respiratory viruses in Korea patients [Internet]. Cheongwon: Korean Centers for Disease Control and Prevention;2013. cited 2015 Aug 1. Available from: http://www.cdc.go.kr/CDC/info/CdcKrInfo0502.jsp?menuIds=HOME001-MNU1175-MNU0048-MNU0050&fid=477&q_type=&q_value=&cid=19952&pageNum=1.26. Roh EJ, Jin YM, Chung EH, Rheem I, Kim JK. The prevalence of respiratory viral infection in exacerbation of asthma in hospitalized children. Korean J Asthma Allergy Clin Immunol. 2007; 27:241–247.27. Kang SH, Choi HM, Lee EH. Positive rates of 2009 novel influenza A (H1N1) was high in school-aged individuals: significance in pandemic control. J Korean Med Sci. 2012; 27:332–334.28. Kim EK, Youn YS, Rhim JW, Shin MS, Kang JH, Lee KY. Epidemiological comparison of three Mycoplasma pneumoniae pneumonia epidemics in a single hospital over 10 years. Korean J Pediatr. 2015; 58:172–177.29. Neuzil KM, Wright PF, Mitchel EF Jr, Griffin MR. The burden of influenza illness in children with asthma and other chronic medical conditions. J Pediatr. 2000; 137:856–864.30. Kloepfer KM, Olenec JP, Lee WM, Liu G, Vrtis RF, Roberg KA, et al. Increased H1N1 infection rate in children with asthma. Am J Respir Crit Care Med. 2012; 185:1275–1279.31. Shin SY, Kim JH, Kim HS, Kang YA, Lee HG, Kim JS, et al. Clinical characteristics of Korean pediatric patients critically ill with influenza A (H1N1) virus. Pediatr Pulmonol. 2010; 45:1014–1020.32. Celenza A, Fothergill J, Kupek E, Shaw RJ. Thunderstorm associated asthma: a detailed analysis of environmental factors. BMJ. 1996; 312:604–607.33. Larsson K, Ohlsén P, Larsson L, Malmberg P, Rydström PO, Ulriksen H. High prevalence of asthma in cross country skiers. BMJ. 1993; 307:1326–1329.34. Rossi OV, Kinnula VL, Tienari J, Huhti E. Association of severe asthma attacks with weather, pollen, and air pollutants. Thorax. 1993; 48:244–248.35. Oh JW, Lee HB, Kang IJ, Kim SW, Park KS, Kook MH, et al. The revised edition of Korean calendar for allergenic pollens. Allergy Asthma Immunol Res. 2012; 4:5–11.36. Green RM, Custovic A, Sanderson G, Hunter J, Johnston SL, Woodcock A. Synergism between allergens and viruses and risk of hospital admission with asthma: case-control study. BMJ. 2002; 324:763.37. Sun HL, Chou MC, Lue KH. The relationship of air pollution to ED visits for asthma differ between children and adults. Am J Emerg Med. 2006; 24:709–713.38. Kim SH, Son JY, Lee JT, Kim TB, Park HW, Lee JH, et al. Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea: a case-crossover study. Korean J Med. 2010; 78:450–456.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study on the Seasonal Occurrence of Asthma in Children
- National Patterns and Characteristics in Pediatric Dental Emergency Visits for Dental Conditions
- Seasonality of asthma exacerbation in children caused by respiratory virus infection and allergen sensitization
- An epidemic of thunderstorm asthma in Melbourne 2016: asthma, rhinitis, and other previous allergies
- The Effects of COVID-19 on the Self-Harm in Children and Adolescents Observed in a University Hospital