Ann Hepatobiliary Pancreat Surg.
2017 Aug;21(3):157-162. 10.14701/ahbps.2017.21.3.157.
Liver lesions detected in a hepatitis B core total antibody-positive patient masquerading as hepatocellular carcinoma: a rare case of peliosis hepatis and a review of the literature
- Affiliations
-
- 1Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, University Surgical Cluster, National University Health System, Singapore. alfred_kow@nuhs.edu.sg
- 2Department of Pathology, National University Health System, Singapore.
- KMID: 2389993
- DOI: http://doi.org/10.14701/ahbps.2017.21.3.157
Abstract
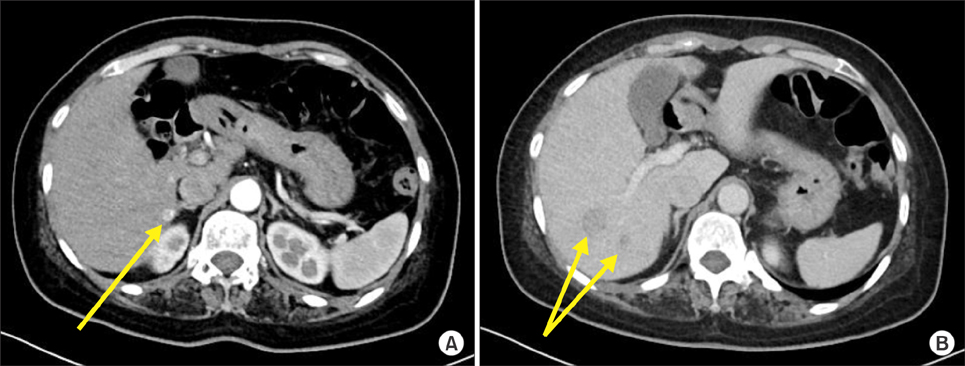
- Peliosis Hepatis (PH) is a rare vascular disorder of the liver, characterized by the presence of cystic blood-filled cavities distributed throughout the hepatic parenchyma. The pathogenesis of PH remains controversial. The preoperative diagnosis of PH is difficult, due to the non-specific imaging characteristics of PH and almost all cases are diagnosed on histology post resection. This study presents a case of PH masquerading as hepatocellular carcinoma (HCC). The patient is a 45-year old Chinese lady, who presented with transaminitis. She was found to be hepatitis B virus core total antibody-positive with an alpha-fetoprotein (AFP) of 29.4 ng/ml. Triphasic liver computed tomography showed several arterial hypervascular lesions and hypoenhancing lesions on the venous phase, particularly in the segments 6/7. Subsequently, a magnetic resonance imaging scan showed multiple lesions in the right hemiliver with an indeterminate enhancement patterns. Subsequently, she decided to undergo a resection procedure. Histopathology revealed findings consistent with PH with some unusual features. This case demonstrates a clinical conundrum, in which PH presented with a raised AFP, in a patient with risk factors for the development of HCC. The clinical suspicion of PH should be high in patients, who present with multiple hepatic lesions with variable enhancement patterns.
Keyword
MeSH Terms
Figure
Reference
-
1. Okada S, Sato T, Okusaka T, Ishii H, Ikeda M, Nakasuka H, et al. Past exposure to hepatitis B virus as a risk factor for hepatocellular carcinoma in patients with chronic liver disease. Br J Cancer. 1998; 77:2028–2031.2. Coppola N, Onorato L, Sagnelli C, Sagnelli E, Angelillo IF. Association between anti-HBc positivity and hepatocellular carcinoma in HBsAg-negative subjects with chronic liver disease: A meta-analysis. Medicine (Baltimore). 2016; 95:e4311.3. Coppola N, Onorato L, Iodice V, Starace M, Minichini C, Farella N, et al. Occult HBV infection in HCC and cirrhotic tissue of HBsAg-negative patients: a virological and clinical study. Oncotarget. 2016; 7:62706–62714.4. Huang CY, Wang ZW. Peliosis hepatis mimicking hepatic malignancy: a case report. J Dig Dis. 2013; 14:272–275.5. Battal B, Akgun V, Sari S. Peliosis hepatis: one pathology, a thousand faces, and a clinical and radiological diagnostic challenge. J Dig Dis. 2014; 15:281–282.6. Grønlykke L, Tarp B, Dutoit SH, Wilkens R. Peliosis hepatis: a complicating finding in a case of biliary colic. BMJ Case Rep. 2013; 2013:bcr2013200539.7. Ferrozzi F, Tognini G, Zuccoli G, Cademartiri F, Pavone P. Peliosis hepatis with pseudotumoral and hemorrhagic evolution: CT and MR findings. Abdom Imaging. 2001; 26:197–199.8. Iannaccone R, Federle MP, Brancatelli G, Matsui O, Fishman EK, Narra VR, et al. Peliosis hepatis: spectrum of imaging findings. AJR Am J Roentgenol. 2006; 187:W43–W52.9. Leslie DF, Johnson CD, MacCarty RL, Ward EM, Ilstrup DM, Harmsen WS. Single-pass CT of hepatic tumors: value of globular enhancement in distinguishing hemangiomas from hypervascular metastases. AJR Am J Roentgenol. 1995; 165:1403–1406.10. Kim EA, Yoon KH, Jeon SJ, Cai QY, Lee YW, Yoon SE, et al. Peliosis hepatis with hemorrhagic necrosis and rupture: a case report with emphasis on the multi-detector CT findings. Korean J Radiol. 2007; 8:64–69.11. Gouya H, Vignaux O, Legmann P, de Pigneux G, Bonnin A. Peliosis hepatis: triphasic helical CT and dynamic MRI findings. Abdom Imaging. 2001; 26:507–509.12. Torabi M, Hosseinzadeh K, Federle MP. CT of nonneoplastic hepatic vascular and perfusion disorders. Radiographics. 2008; 28:1967–1982.13. Xiong WJ, Hu LJ, Jian YC, He Y, Zhou W, Guo XL, et al. Focal peliosis hepatis in a colon cancer patient resembling metastatic liver tumor. World J Gastroenterol. 2012; 18:5999–6002.14. Alessandrino F, Felisaz PF, La Fianza A. Peliosis hepatis associated with hereditary haemorrhagic telangiectasia. Gastroenterol Rep (Oxf). 2013; 1:203–206.15. Crocetti D, Palmieri A, Pedullà G, Pasta V, D'Orazi V, Grazi GL. Peliosis hepatis: Personal experience and literature review. World J Gastroenterol. 2015; 21:13188–13194.16. Steinke K, Terraciano L, Wiesner W. Unusual cross-sectional imaging findings in hepatic peliosis. Eur Radiol. 2003; 13:1916–1919.17. Kim SH, Lee JM, Kim WH, Han JK, Lee JY, Choi BI. Focal peliosis hepatis as a mimicker of hepatic tumors: radiological-pathological correlation. J Comput Assist Tomogr. 2007; 31:79–85.18. Tsokos M, Erbersdobler A. Pathology of peliosis. Forensic Sci Int. 2005; 149:25–33.19. Hayward SR, Lucas CE, Ledgerwood AM. Recurrent spontaneous intrahepatic hemorrhage from peliosis hepatis. Arch Surg. 1991; 126:782–783.20. Yanoff M, Rawson AJ. Peliosis hepatis. An anatomic study with demonstration of two varieties. Arch Pathol. 1964; 77:159–165.21. Zak FG. Peliosis hepatis. Am J Pathol. 1950; 26:1–15. incl 2 pl.22. Khadilkar UN, Prabhu S, Sharma D. Peliosis hepatis presenting as hemoperitoneum. Indian J Med Sci. 2008; 62:236–237.23. Choi SK, Jin JS, Cho SG, Choi SJ, Kim CS, Choe YM, et al. Spontaneous liver rupture in a patient with peliosis hepatis: a case report. World J Gastroenterol. 2009; 15:5493–5497.24. Sommacale D, Palladino E, Tamby EL, Diebold MD, Kianmanesh AR. Spontaneous hepatic rupture in a patient with peliosis hepatis: A report of one case. Int J Surg Case Rep. 2013; 4:508–510.25. Berzigotti A, Magalotti D, Zappoli P, Rossi C, Callea F, Zoli M. Peliosis hepatis as an early histological finding in idiopathic portal hypertension: A case report. World J Gastroenterol. 2006; 12:3612–3615.26. Zafrani ES, Cazier A, Baudelot AM, Feldmann G. Ultrastructural lesions of the liver in human peliosis. A report of 12 cases. Am J Pathol. 1984; 114:349–359.27. Mungan Z, Pinarbasi B, Bakir B, Gulluoglu M, Baran B, Akyuz F, et al. Congenital portal vein aneurysm associated with peliosis hepatis and intestinal lymphangiectasia. Gastroenterol Res Pract. 2009; 2009:479264.28. Kleger A, Bommer M, Kunze M, Klaus J, Leithaeuser F, Wegener M, et al. First reported case of disease: peliosis hepatis as cardinal symptom of Hodgkin's lymphoma. Oncologist. 2009; 14:1088–1094.29. Motoki T, Fukuda M, Nakano T, Matsukage S, Fukui A, Akiyoshi S, et al. Fatal hepatic hemorrhage by peliosis hepatis in X-linked myotubular myopathy: a case report. Neuromuscul Disord. 2013; 23:917–921.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Focal Peliosis Hepatis Mimicking Hepatocellular Carcinoma
- Spiral CT Findings of Peliosis Hepatis: A Case Report
- A Case of Peliosis Hepatis, Diagnosed by Peritoneoscopic Liver Biopsy
- Peliosis Hepatis Shows Isometabolism on 18F-FDG PET/CT: Two Case Reports
- Peliosis Hepatis Cured with Anti-tuberculosis Medication in a Hemodialysis Patient