Korean Circ J.
2016 Sep;46(5):632-638. 10.4070/kcj.2016.46.5.632.
Impact of Cigarette Smoking: a 3-Year Clinical Outcome of Vasospastic Angina Patients
- Affiliations
-
- 1Department of Medicine, Korea University Graduate School, Seoul, Korea.
- 2Cardiovascular Center, Korea University Guro Hospital, Seoul, Korea. swrha617@yahoo.co.kr
- 3Department of General Internal Medicine, Weiss Memorial Hospital, Chicago, IL, USA.
- 4Department of Cardiology, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- 5Cardiovascular Center, Eulji University, Eulji General Hospital, Seoul, Korea.
- 6Cardiovascular Center, Chungju Kunkuk University, Chungju, Korea.
- 7Cardiovascular Center, Seonam University, Myongji Hospital, Goyang, Korea.
- KMID: 2389619
- DOI: http://doi.org/10.4070/kcj.2016.46.5.632
Abstract
- BACKGROUND AND OBJECTIVES
Cigarette smoking is a risk significant factor in coronary artery disease (CAD) and vasospastic angina (VSA). However, it is largely unknown whether smoking adds to any long-term clinical risk in VSA patients.
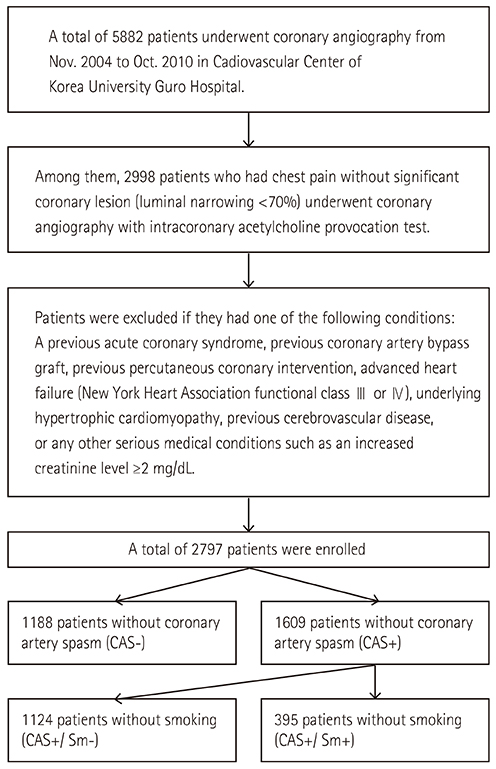
SUBJECTS AND METHODS
A total of 2797 patients without significant CAD underwent acetylcholine (Ach) provocation test between November 2004 and October 2010. Patients were divided into three groups, based on the presence of coronary artery spasm (CAS) and smoking habits (non-CAS group: n=1188, non-smoking CAS group: n=1214, smoking CAS group: n=395). All CAS patients were prescribed with anti-anginal medications for at least 6 months. The incidence of major clinical outcomes and recurrent angina of these groups were compared up to 3 years.
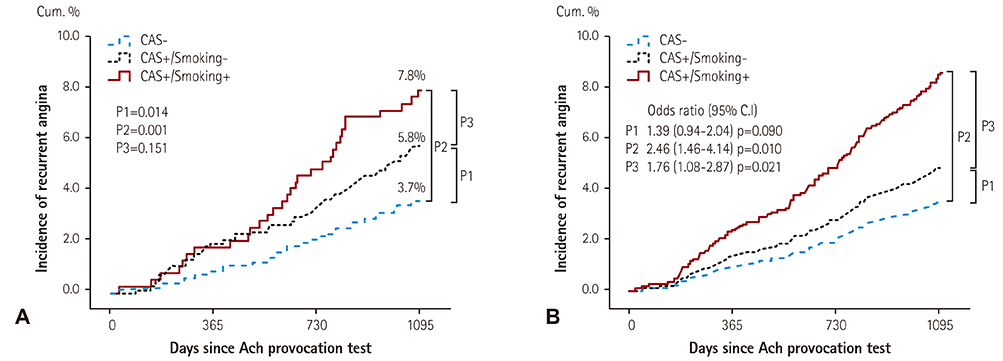
RESULTS
There were considerable differences in the baseline clinical and angiographic characteristics among the three groups, but there was no difference in the endpoints among the three groups (including individual and composite hard endpoints) such as death, myocardial infarction, de novo percutaneous coronary intervention, cerebrovascular accident, and major adverse cardiac events. However, there was a higher incidence of recurrent angina in both the non-smoking CAS group and smoking CAS group, as compared to the non-CAS group. In multivariable adjusted Cox-proportional hazards regression analysis, smoking CAS group exhibited a higher incidence of recurrent angina compared with the non-CAS group (hazard ratio [HR]; 2.46, 95% confidence interval [CI]; 1.46-4.14, p=0.001) and non-smoking CAS group (HR; 1.76, 95% CI; 1.08-2.87, p=0.021).
CONCLUSION
Cigarette smoking CAS group exhibited higher incidence of recurrent angina during the 3-year clinical follow-up compared with both the non-CAS group and non-smoking CAS group. Quitting of smoking, paired with intensive medical therapy and close clinical follow-up, can help to prevent recurrent angina.
MeSH Terms
Figure
Cited by 2 articles
-
Ergonovine Provocation Echocardiography for Detection and Prognostication in Patients with Vasospastic Angina
Jae-Hyeong Park
Korean Circ J. 2018;48(10):917-919. doi: 10.4070/kcj.2018.0139.Impact of Insulin Resistance on Acetylcholine-Induced Coronary Artery Spasm in Non-Diabetic Patients
Kwan Woo Kang, Byoung Geol Choi, Seung-Woon Rha
Yonsei Med J. 2018;59(9):1057-1063. doi: 10.3349/ymj.2018.59.9.1057.
Reference
-
1. Kugiyama K, Yasue H, Okumura K, et al. Nitric oxide activity is deficient in spasm arteries of patients with coronary spastic angina. Circulation. 1996; 94:266–271.2. Kugiyama K, Ohgushi M, Motoyama T, et al. Nitric oxide-mediated flow-dependent dilation is impaired in coronary arteries in patients with coronary spastic angina. J Am Coll Cardiol. 1997; 30:920–926.3. Kugiyama K, Murohara T, Yasue H, et al. Increased constrictor response to acetylcholine of the isolated coronary arteries from patients with variant angina. Int J Cardiol. 1995; 52:223–233.4. Beltrame JF, Sasayama S, Maseri A. Racial heterogeneity in coronary artery vasomotor reactivity: differences between Japanese and Caucasian patients. J Am Coll Cardiol. 1999; 33:1442–1452.5. Erhardt L. Cigarette smoking: an undertreated risk factor for cardiovascular disease. Atherosclerosis. 2009; 205:23–32.6. Sugiishi M, Takatsu F. Cigarette smoking is a major risk factor for coronary spasm. Circulation. 1993; 87:76–79.7. Wolf PA, D'Agostino RB, Kannel WB, Bonita R, Belanger AJ. Cigarette smoking as a risk factor for stroke. The Framingham Study. JAMA. 1988; 259:1025–1029.8. Bornemisza P, Major G, Suciu I, Major I. Cigarette smoking as a risk factor for atherosclerosis. Study of the biologic changes consecutive to smoking in normals, in patients with coronary heart disease and in diabetics. Med Interne. 1981; 19:251–258.9. Cheon BW, Rha SW, Wani SP, et al. Impact of smoking and smoking-related parameters on acetylcholine-induced coronary artery spasm. Korean Circ J. 2006; 36:661–665.10. Brunner H, Cockcroft JR, Deanfield J, et al. Endothelial function and dysfunction. Part II: Association with cardiovascular risk factors and diseases. A statement by the Working Group on Endothelins and Endothelial Factors of the European Society of Hypertension. J Hypertens. 2005; 23:233–246.11. de Maat MP, Pietersma A, Kofflard M, Sluiter W, Kluft C. Association of plasma fibrinogen levels with coronary artery disease, smoking and inflammatory markers. Atherosclerosis. 1996; 121:185–191.12. Park JY, Rha SW, Li YJ, et al. The impact of high sensitivity C-reactive protein level on coronary artery spasm as assessed by intracoronary acetylcholine provocation test. Yonsei Med J. 2013; 54:1299–1304.13. Takaoka K, Yoshimura M, Ogawa H, et al. Comparison of the risk factors for coronary artery spasm with those for organic stenosis in a Japanese population: role of cigarette smoking. Int J Cardiol. 2000; 72:121–126.14. Figueras J, Domingo E, Ferreira I, Lidón RM, Garcia-Dorado D. Persistent angina pectoris, cardiac mortality and myocardial infarction during a 12 year follow-up in 273 variant angina patients without significant fixed coronary stenosis. Am J Cardiol. 2012; 110:1249–1255.15. Choi BG, Park SH, Rha SW, et al. Five-year clinical outcomes in patients with significant coronary artery spasm: A propensity score-matched analysis. Int J Cardiol. 2015; 184:533–539.16. Bakhru A, Erlinger TP. Smoking cessation and cardiovascular disease risk factors: results from the Third National Health and Nutrition Examination Survey. PLoS Med. 2005; 2:e160.17. Haustein KO, Krause J, Haustein H, Rasmussen T, Cort N. Changes in hemorheological and biochemical parameters following short-term and long-term smoking cessation induced by nicotine replacement therapy (NRT). Int J Clin Pharmacol Ther. 2004; 42:83–92.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Exercise-Induced Vasospastic Angina With Prominent Regional Wall Motion Abnormality
- Diagnostic Significance of ECG Ergonovine Provocation Test in Patients with Vasospastic Angina
- The Vasomotor Tone In Vasospastic Angina
- Cigarette Smoking in South Korea: A Narrative Review
- Recent Insights Into the Mechanisms of Vasospastic Angina