Neurointervention.
2017 Sep;12(2):116-121. 10.5469/neuroint.2017.12.2.116.
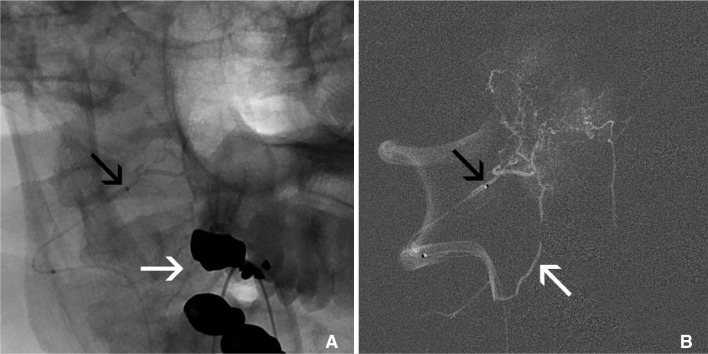
Improving Forward Infusion Pressure during Brain Tumor Embolization with the Double Catheter and Coil Technique
- Affiliations
-
- 1Neurosurgery, Baylor Scott & White Neuroscience Institute, Temple, USA. walter.lesley@bswhealth.org
- 2NeuroInterventional Surgery, Baylor Scott & White Neuroscience Institute, Temple, USA.
- 3College of Medicine, Texas A&M Health Sciences Center, Temple, TX, USA.
- KMID: 2389504
- DOI: http://doi.org/10.5469/neuroint.2017.12.2.116
Abstract
- Endovascular embolization or embosurgery of brain tumors can be used to reduce neoplasm vascularity prior to surgical resection. Two challenges with embosurgery relate to insufficient perfusion pressure into the tumor and inadvertent escape of infused agents into parenchymal branches of the adjacent brain. This report describes a multi-catheter and coil technique to improve tumor perfusion and prevent reflux into normal branches.
Figure
Reference
-
1. Waldron JS, Sughrue ME, Hetts SW, Wilson SP, Mills SA, McDermott MW, et al. Embolization of skull base meningiomas and feeding vessels arising from the internal carotid circulation. Neurosurgery. 2011; 68:162–169.
Article2. Abdel Kerim A, Bonneville F, Jean B, Cornu P, LeJean L, Chiras J. Balloon-assisted embolization of skull base meningioma with liquid embolic agent. J Neurosurg. 2010; 112:70–72. PMID: 19361255.3. Baldi I, Engelhardt J, Bonnet C, Bauchet L, Berteaud E, Grüber A, Loiseau H. Epidemiology of meningiomas. Neurochirurgie. 2014; 9. 20.
Article4. Rockhill J, Mrugala M, Chamberlain MC. Intracranial meningiomas: an overview of diagnosis and treatment. Neurosurg Focus. 2007; 23:E1.
Article5. Klinger DR, Flores BC, Lewis JJ, Barnett SL. The treatment of cavernous sinus meningiomas: evolution of a modern approach. Neurosurg Focus. 2013; 35:E8.
Article6. Singla A, Deshaies EM, Melnyk V, Toshkezi G, Swarnkar A, Choi H, et al. Controversies in the role of preoperative embolization in meningioma management. Neurosurg Focus. 2013; 35:E17. PMID: 24289125.
Article7. Dowd CF, Halbach VV, Higashida RT. Meningiomas: the role of preoperative angiography and embolization. Neurosurg Focus. 2003; 15:E10.
Article8. Mine B, Delpierre I, Hassid S, De Witte O, Lubicz B. The role of interventional neuroradiology in the management of skull base tumours and related surgical complications. B-ENT. 2011; 7(Suppl 17):61–66.9. Bendszus M, Rao G, Burger R, Schaller C, Scheinemann K, Warmuth-Metz M, et al. Is there a benefit of preoperative meningioma embolization? Neurosurgery. 2000; 47:1306–1311. discussion 1311-1302. PMID: 11126901.
Article10. Lazzaro MA, Badruddin A, Zaidat OO, Darkhabani Z, Pandya DJ, Lynch JR. Endovascular embolization of head and neck tumors. Front Neurol. 2011; 2:64. PMID: 22022319.
Article11. Duffis EJ, Gandhi CD, Prestigiacomo CJ, Abruzzo T, Albuquerque F, Bulsara KR, et al. Society for Neurointerventional Surgery. Head, neck, and brain tumor embolization guidelines. J Neurointerv Surg. 2012; 4:251–225. PMID: 22539531.12. Trivelatto F, Nakiri GS, Manisor M, Riva R, Al-Khawaldeh M, Kessler I, et al. Preoperative onyx embolization of meningiomas fed by the ophthalmic artery: a case series. AJNR Am J Neuroradiol. 2011; 32:1762–1766. PMID: 21835949.
Article13. Elhammady MS, Peterson EC, Johnson JN, Aziz-Sultan MA. Preoperative onyx embolization of vascular head and neck tumors by direct puncture. World Neurosurg. 2012; 77:725–730. PMID: 22079824.
Article14. Rangel-Castilla L, Shah AH, Klucznik RP, Diaz OM. Preoperative Onyx embolization of hypervascular head, neck, and spinal tumors: experience with 100 consecutive cases from a single tertiary center. J Neurointerv Surg. 2014; 6:51–56. PMID: 23268473.
Article15. Carli DF, Sluzewski M, Beute GN, van Rooij WJ. Complications of particle embolization of meningiomas: frequency, risk factors, and outcome. AJNR Am J Neuroradiol. 2010; 31:152–154. PMID: 19729535.16. Blakeley J. Drug delivery to brain tumors. Curr Neurol Neurosci Rep. 2008; 8:235–241. PMID: 18541119.
Article17. Peschillo S, Miscusi M, Missori P. Endovascular superselective treatment of brain tumors: a new endovascular era? A quick review. J Neurointerv Surg. 2015; 7:222–224. PMID: 24510377.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ferromagnetic Artifact Due to Metallic Embolic Fragment after Endosaccular Coil Embolization: A Case Report
- Manual Aspiration Technique to Retrieve a Prematurely Detached Coil during Cerebral Aneurysm Embolization
- Delayed cranial nerve palsy after successful coil embolization in cavernous sinus lesion
- Endovascular Treatment of Cerebral Aneurysms: Technical Options in Coil Embolization
- Initial Experience with the New Double-lumen Scepter Balloon Catheter for Treatment of Wide-necked Aneurysms