Ann Rehabil Med.
2017 Aug;41(4):621-630. 10.5535/arm.2017.41.4.621.
Effect of Patient Education on Reducing Medication in Spinal Cord Injury Patients With Neuropathic Pain
- Affiliations
-
- 1Department of Rehabilitation Medicine and Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine, Seoul, Korea. parkhankyul@gmail.com
- KMID: 2389408
- DOI: http://doi.org/10.5535/arm.2017.41.4.621
Abstract
OBJECTIVE
To determine whether providing education about the disease pathophysiology and drug mechanisms and side effects, would be effective for reducing the use of pain medication while appropriately managing neurogenic pain in spinal cord injury (SCI) patients.
METHODS
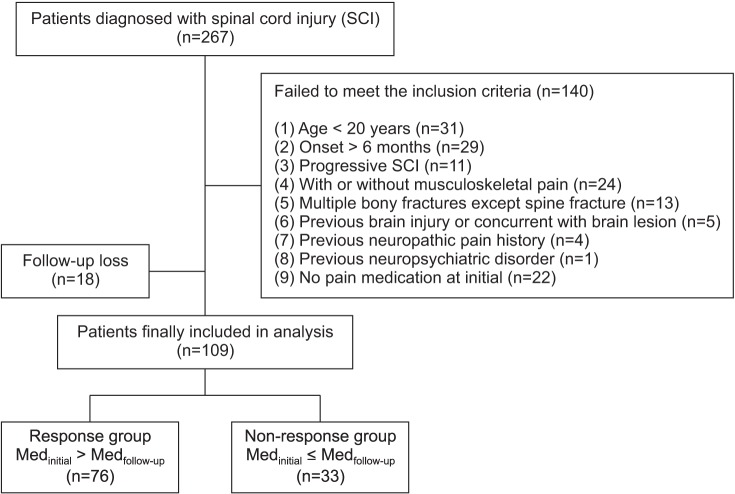
In this prospective study, 109 patients with an SCI and neuropathic pain, participated in an educational pain management program. This comprehensive program was specifically created, for patients with an SCI and neuropathic pain. It consisted of 6 sessions, including educational training, over a 6-week period.
RESULTS
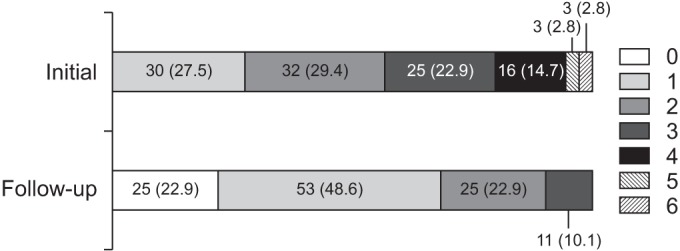
Of 109 patients, 79 (72.5%) initially took more than two types of pain medication, and this decreased to 36 (33.0%) after the educational pain management program was completed. The mean pain scale score and the number of pain medications decreased, compared to the baseline values. Compared to the non-response group, the response group had a shorter duration of pain onset (p=0.004), and a higher initial number of different medications (p<0.001) and certain types of medications.
CONCLUSION
This study results imply that an educational pain management program, can be a valuable complement to the treatment of spinal cord injured patients with neuropathic pain. Early intervention is important, to prevent patients from developing chronic SCI-related pain.
Keyword
MeSH Terms
Figure
Reference
-
1. Werhagen L, Budh CN, Hultling C, Molander C. Neuropathic pain after traumatic spinal cord injury: relations to gender, spinal level, completeness, and age at the time of injury. Spinal Cord. 2004; 42:665–673. PMID: 15289801.2. Werhagen L, Hultling C, Molander C. The prevalence of neuropathic pain after non-traumatic spinal cord lesion. Spinal Cord. 2007; 45:609–615. PMID: 17160075.
Article3. Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003; 103:249–257. PMID: 12791431.
Article4. Norrbrink Budh C, Hultling C, Lundeberg T. Quality of sleep in individuals with spinal cord injury: a comparison between patients with and without pain. Spinal Cord. 2005; 43:85–95. PMID: 15570322.
Article5. van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J. Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur J Pain. 2015; 19:5–14. PMID: 24824334.
Article6. Cuff L, Fann JR, Bombardier CH, Graves DE, Kalpakjian CZ. Depression, pain intensity, and interference in acute spinal cord injury. Top Spinal Cord Inj Rehabil. 2014; 20:32–39. PMID: 24574820.
Article7. Siddall PJ. Management of neuropathic pain following spinal cord injury: now and in the future. Spinal Cord. 2009; 47:352–359. PMID: 19002150.
Article8. Wollaars MM, Post MW, van Asbeck FW, Brand N. Spinal cord injury pain: the influence of psychologic factors and impact on quality of life. Clin J Pain. 2007; 23:383–391. PMID: 17515736.
Article9. van Leeuwen CM, Post MW, van Asbeck FW, Bongers-Janssen HM, van der Woude LH, de Groot S, et al. Life satisfaction in people with spinal cord injury during the first five years after discharge from inpatient rehabilitation. Disabil Rehabil. 2012; 34:76–83. PMID: 21870935.
Article10. Dworkin RH, O'Connor AB, Audette J, Baron R, Gourlay GK, Haanpaa ML, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010; 85(3 Suppl):S3–14.
Article11. Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 2010; 9:807–819. PMID: 20650402.
Article12. Baastrup C, Finnerup NB. Pharmacological management of neuropathic pain following spinal cord injury. CNS Drugs. 2008; 22:455–475. PMID: 18484790.
Article13. Backonja MM, Irving G, Argoff C. Rational multidrug therapy in the treatment of neuropathic pain. Curr Pain Headache Rep. 2006; 10:34–38. PMID: 16499828.
Article14. Siddall PJ, Middleton JW. A proposed algorithm for the management of pain following spinal cord injury. Spinal Cord. 2006; 44:67–77. PMID: 16116488.
Article15. Attal N, Cruccu G, Baron R, Haanpaa M, Hansson P, Jensen TS, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010; 17:1113–1e88. PMID: 20402746.
Article16. Kitzman P, Cecil D, Kolpek JH. The risks of polypharmacy following spinal cord injury. J Spinal Cord Med. 2017; 40:147–153. PMID: 24970339.
Article17. Mehta S, Orenczuk K, McIntyre A, Willems G, Wolfe DL, Hsieh JT, et al. Neuropathic pain post spinal cord injury part 1: systematic review of physical and behavioral treatment. Top Spinal Cord Inj Rehabil. 2013; 19:61–77. PMID: 23678287.
Article18. Meyer TJ, Van Kooten D, Marsh S, Prochazka AV. Reduction of polypharmacy by feedback to clinicians. J Gen Intern Med. 1991; 6:133–136. PMID: 2023020.
Article19. Widerstrom-Noga E, Biering-Sorensen F, Bryce TN, Cardenas DD, Finnerup NB, Jensen MP, et al. The International Spinal Cord Injury Pain Basic Data Set (version 2.0). Spinal Cord. 2014; 52:282–286. PMID: 24469147.
Article20. Bryce TN, Biering-Sorensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T, et al. International spinal cord injury pain classification. Part I. Background and description. March 6-7, 2009. Spinal Cord. 2012; 50:413–417. PMID: 22182852.21. Hwang M, Zebracki K, Vogel LC. Medication profile and polypharmacy in adults with pediatric-onset spinal cord injury. Spinal Cord. 2015; 53:673–678. PMID: 25896344.
Article22. Finnerup NB, Baastrup C. Spinal cord injury pain: mechanisms and management. Curr Pain Headache Rep. 2012; 16:207–216. PMID: 22392531.
Article23. Kalpakjian CZ, Bombardier CH, Schomer K, Brown PA, Johnson KL. Measuring depression in persons with spinal cord injury: a systematic review. J Spinal Cord Med. 2009; 32:6–24. PMID: 19264045.
Article24. Ataoglu E, Tiftik T, Kara M, Tunc H, Ersoz M, Akkus S. Effects of chronic pain on quality of life and depression in patients with spinal cord injury. Spinal Cord. 2013; 51:23–26. PMID: 22547044.
Article25. American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012; 60:616–631. PMID: 22376048.26. Teasell RW, Mehta S, Aubut JA, Foulon B, Wolfe DL, Hsieh JT, et al. A systematic review of pharmacologic treatments of pain after spinal cord injury. Arch Phys Med Rehabil. 2010; 91:816–831. PMID: 20434623.
Article27. Pitkala KH, Strandberg TE, Tilvis RS. Is it possible to reduce polypharmacy in the elderly? A randomised, controlled trial. Drugs Aging. 2001; 18:143–149. PMID: 11346128.28. Widerstrom-Noga EG, Felipe-Cuervo E, Yezierski RP. Chronic pain after spinal injury: interference with sleep and daily activities. Arch Phys Med Rehabil. 2001; 82:1571–1577. PMID: 11689978.29. Hanlon JT, Weinberger M, Samsa GP, Schmader KE, Uttech KM, Lewis IK, et al. A randomized, controlled trial of a clinical pharmacist intervention to improve inappropriate prescribing in elderly outpatients with polypharmacy. Am J Med. 1996; 100:428–437. PMID: 8610730.
Article30. Wand BM, Bird C, McAuley JH, Dore CJ, MacDowell M, De Souza LH. Early intervention for the management of acute low back pain: a single-blind randomized controlled trial of biopsychosocial education, manual therapy, and exercise. Spine (Phila Pa 1976). 2004; 29:2350–2356. PMID: 15507794.31. Cardenas DD, Jensen MP. Treatments for chronic pain in persons with spinal cord injury: a survey study. J Spinal Cord Med. 2006; 29:109–117. PMID: 16739554.
Article32. Finnerup NB, Haroutounian S, Kamerman P, Baron R, Bennett DL, Bouhassira D, et al. Neuropathic pain: an updated grading system for research and clinical practice. Pain. 2016; 157:1599–1606. PMID: 27115670.
Article33. Rollason V, Vogt N. Reduction of polypharmacy in the elderly: a systematic review of the role of the pharmacist. Drugs Aging. 2003; 20:817–832. PMID: 12964888.34. Mahnig S, Landmann G, Stockinger L, Opsommer E. Pain assessment according to the International Spinal Cord Injury Pain classification in patients with spinal cord injury referred to a multidisciplinary pain center. Spinal Cord. 2016; 54:809–815. PMID: 26754471.
Article35. Tarride JE, Gordon A, Vera-Llonch M, Dukes E, Rousseau C. Cost-effectiveness of pregabalin for the management of neuropathic pain associated with diabetic peripheral neuropathy and postherpetic neuralgia: a Canadian perspective. Clin Ther. 2006; 28:1922–1934. PMID: 17213013.
Article36. Tzellos TG, Papazisis G, Amaniti E, Kouvelas D. Efficacy of pregabalin and gabapentin for neuropathic pain in spinal-cord injury: an evidence-based evaluation of the literature. Eur J Clin Pharmacol. 2008; 64:851–858. PMID: 18607580.
Article37. Reddy PS, Waseemuddin M. Assessment of drug related problems in geriatrics with polypharmacy and risk measurement. Asian J Pharm Technol Innov. 2014; 2:39–58.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spinal cord stimulation for neuropathic pain following idiopathic transverse myelitis: A case report
- Spinal Gap Junction Channels in Neuropathic Pain
- Management of Spinal Cord Injury Pain with Small Divided Doses of Intravenous Ketamine
- Posterior Cord Syndrome After Spinal Cord Stimulation Electrode Lead Insertion: A Case Report
- Intractable Abdominal Pain in a Patient With Spinal Cord Injury: A Case Report