Korean Circ J.
2015 May;45(3):194-201. 10.4070/kcj.2015.45.3.194.
Usefulness of Hyperemic Microvascular Resistance Index as a Predictor of Clinical Outcomes in Patients with ST-Segment Elevation Myocardial Infarction
- Affiliations
-
- 1Department of Cardiology, Ajou University School of Medicine, Suwon, Korea. yoonmh65@hanmail.net
- KMID: 2389126
- DOI: http://doi.org/10.4070/kcj.2015.45.3.194
Abstract
- BACKGROUND AND OBJECTIVES
Microvascular function is a useful predictor of left ventricular functional changes in patients with ST-segment elevation myocardial infarction (STEMI). We evaluated the usefulness of the hyperemic microvascular resistance index (hMVRI) for predicting long-term major adverse cardiovascular events (MACEs) in patients with STEMI assessed immediately after primary percutaneous coronary intervention (PCI).
SUBJECTS AND METHODS
hMVRI were evaluated in 145 patients with first acute STEMI treated with primary PCI using an intracoronary Doppler wire. hMVRI was defined as the ratio of mean aortic pressure over hyperemic averaged peak velocity of infarct-related artery. Major adverse cardiovascular events (MACEs) included cardiac death and re-hospitalization for congestive heart failure.
RESULTS
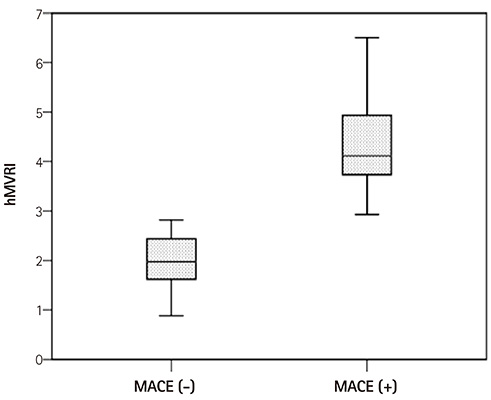
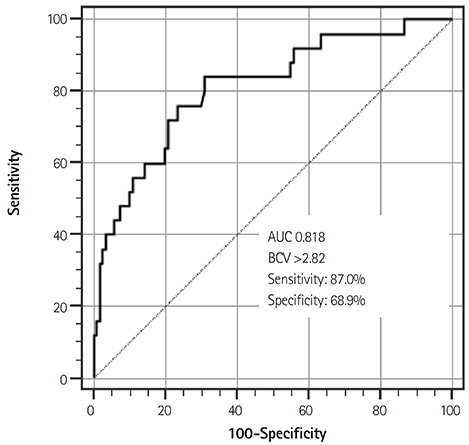
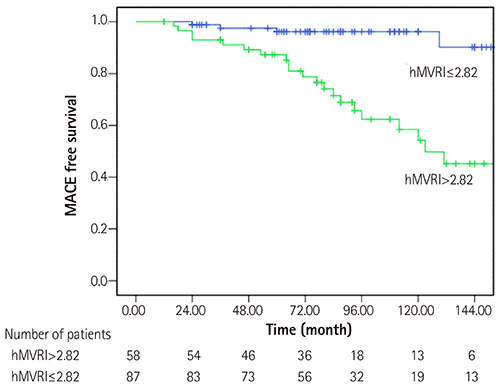
During the mean follow-up of 85+/-43 months, MACEs occurred in 17.2% of patients. Using a receiver-operating characteristics analysis, hMVRI >2.82 mm Hg.cm-1.sec (sensitivity: 87%; specificity: 69%; and area under curve: 0.818) was the best cut-off values for predicting future cardiac events. The Cox proportional hazard analysis showed that hMVRI was an independent predictor for long-term MACEs (hazard ratio 1.741, 95% confidence interval 1.348-2.264, p<0.001). The Kaplan-Meier survival analysis showed a higher incidence of MACEs in patients with hMVRI >2.82 mm Hg.cm-1.sec (p<0.001).
CONCLUSION
hMVRI was a strong predictor of long-term MACEs in patients with STEMI treated with primary PCI.
MeSH Terms
Figure
Cited by 1 articles
-
Therapeutic Hypothermia for Cardioprotection in Acute Myocardial Infarction
In Sook Kang, Ikeno Fumiaki, Wook Bum Pyun
Yonsei Med J. 2016;57(2):291-297. doi: 10.3349/ymj.2016.57.2.291.
Reference
-
1. Gibson CM, Cannon CP, Murphy SA, et al. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation. 2000; 101:125–130.2. Gibson CM, Cannon CP, Murphy SA, et al. Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction. Circulation. 2002; 105:1909–1913.3. Fearon WF, Balsam LB, Farouque HM, et al. Novel index for invasively assessing the coronary microcirculation. Circulation. 2003; 107:3129–3132.4. Fearon WF, Shah M, Ng M, et al. Predictive value of the index of microcirculatory resistance in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2008; 51:560–565.5. Lim HS, Yoon MH, Tahk SJ, et al. Usefulness of the index of microcirculatory resistance for invasively assessing myocardial viability immediately after primary angioplasty for anterior myocardial infarction. Eur Heart J. 2009; 30:2854–2860.6. Lepper W, Hoffmann R, Kamp O, et al. Assessment of myocardial reperfusion by intravenous myocardial contrast echocardiography and coronary flow reserve after primary percutaneous transluminal coronary angioplasty [correction of angiography] in patients with acute myocardial infarction. Circulation. 2000; 101:2368–2374.7. Takahashi T, Hiasa Y, Ohara Y, et al. Usefulness of coronary flow reserve immediately after primary coronary stenting in predicting wall motion recovery in patients with anterior wall acute myocardial infarction. Am J Cardiol. 2004; 94:1033–1037.8. Yoon MH, Tahk SJ, Yang HM, et al. Comparison of accuracy in the prediction of left ventricular wall motion changes between invasively assessed microvascular integrity indexes and fluorine-18 fluorodeoxyglucose positron emission tomography in patients with ST-elevation myocardial infarction. Am J Cardiol. 2008; 102:129–134.9. Yamamoto K, Ito H, Iwakura K, et al. Pressure-derived collateral flow index as a parameter of microvascular dysfunction in acute myocardial infarction. J Am Coll Cardiol. 2001; 38:1383–1389.10. Kawamoto T, Yoshida K, Akasaka T, et al. Can coronary blood flow velocity pattern after primary percutaneous transluminal coronary angioplasty [correction of angiography] predict recovery of regional left ventricular function in patients with acute myocardial infarction? Circulation. 1999; 100:339–345.11. Ng MK, Yeung AC, Fearon WF. Invasive assessment of the coronary microcirculation: superior reproducibility and less hemodynamic dependence of index of microcirculatory resistance compared with coronary flow reserve. Circulation. 2006; 113:2054–2061.12. Klauss V, Ackermann K, Henneke KH, et al. Epicardial intimal thickening in transplant coronary artery disease and resistance vessel response to adenosine: a combined intravascular ultrasound and Doppler study. Circulation. 1997; 96:Suppl 9. II-159–II-164.13. Schiller NB, Shah PM, Crawford M, et al. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. J Am Soc Echocardiogr. 1989; 2:358–367.14. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971; 285:1441–1446.15. Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007; 356:830–840.16. Furber AP, Prunier F, Nguyen HC, Boulet S, Delépine S, Geslin P. Coronary blood flow assessment after successful angioplasty for acute myocardial infarction predicts the risk of long-term cardiac events. Circulation. 2004; 110:3527–3533.17. Leung DY, Leung M. Non-invasive/invasive imaging: significance and assessment of coronary microvascular dysfunction. Heart. 2011; 97:587–595.18. van Liebergen RA, Piek JJ, Koch KT, de Winter RJ, Lie KI. Immediate and long-term effect of balloon angioplasty or stent implantation on the absolute and relative coronary blood flow velocity reserve. Circulation. 1998; 98:2133–2140.19. Kitabata H, Imanishi T, Kubo T, et al. Coronary microvascular resistance index immediately after primary percutaneous coronary intervention as a predictor of the transmural extent of infarction in patients with ST-segment elevation anterior acute myocardial infarction. JACC Cardiovasc Imaging. 2009; 2:263–272.20. Anjeja BG, Gibson CM. Preserved coronary flow reserve in viable myocardium: further evidence for the microvascular hypothesis. Am Heart J. 2001; 141:329–330.21. Aarnoudse W, Fearon WF, Manoharan G, et al. Epicardial stenosis severity does not affect minimal microcirculatory resistance. Circulation. 2004; 110:2137–2142.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differences in Clinical Outcomes Between Patients With ST-Elevation Versus Non-ST-Elevation Acute Myocardial Infarction in Korea
- A Case of ST-Segment Elevation in a Patient with Subarachnoid Hemorrhage
- ST segment
- Clinical and Angiographic Predictors of Microvascular Dysfunction in ST-Segment Elevation Myocardial Infarction
- Acute Myocardial Infarction by Right Coronary Artery Occlusion Presenting as Precordial ST Elevation on Electrocardiography