J Rheum Dis.
2017 Aug;24(4):236-240. 10.4078/jrd.2017.24.4.236.
Cytoplasmic Anti-Neutrophil Cytoplasmic Antibody Positive Diffuse Alveolar Hemorrhage Associated with Methimazole
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Ajou University School of Medicine, Suwon, Korea. jhpamc@hanmail.net
- 2Department of Rheumatology, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2389065
- DOI: http://doi.org/10.4078/jrd.2017.24.4.236
Abstract
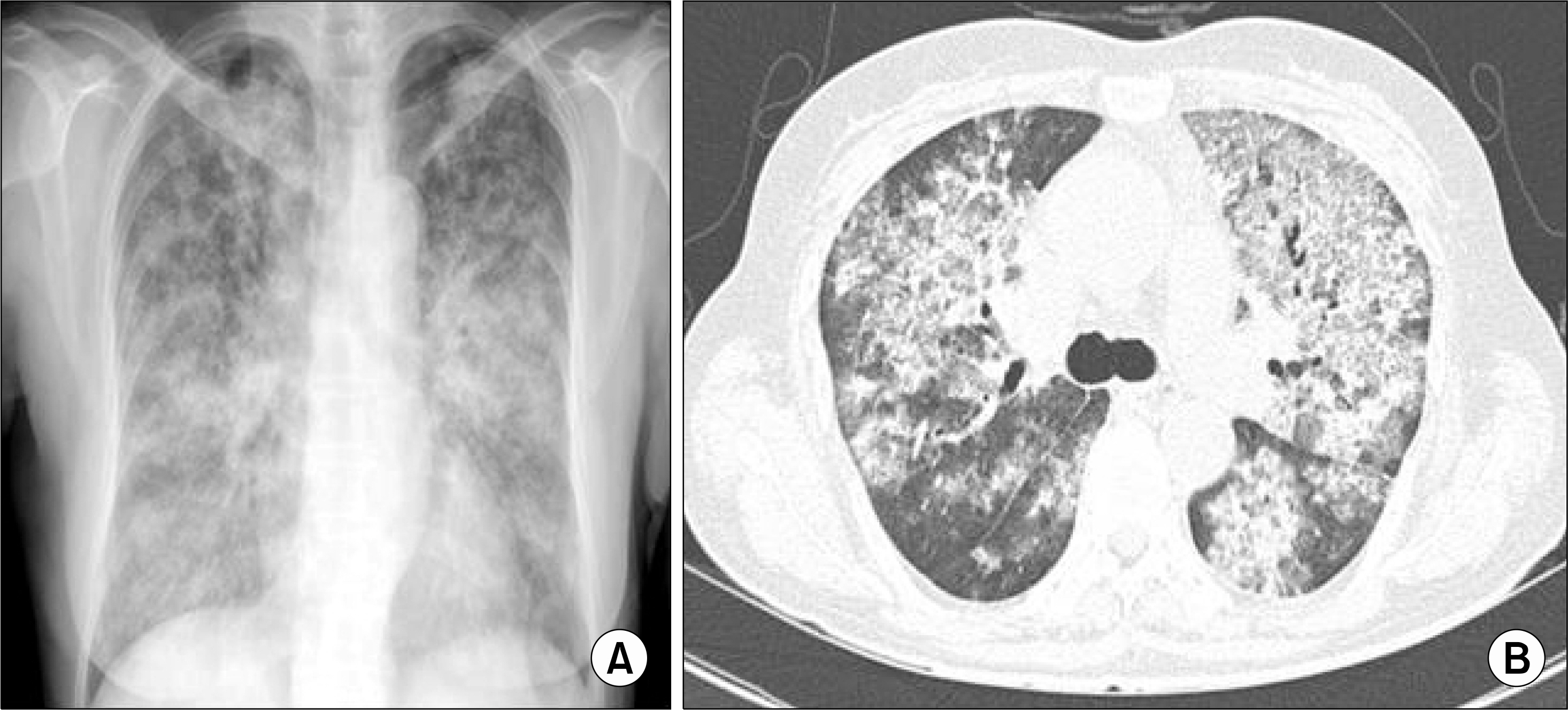
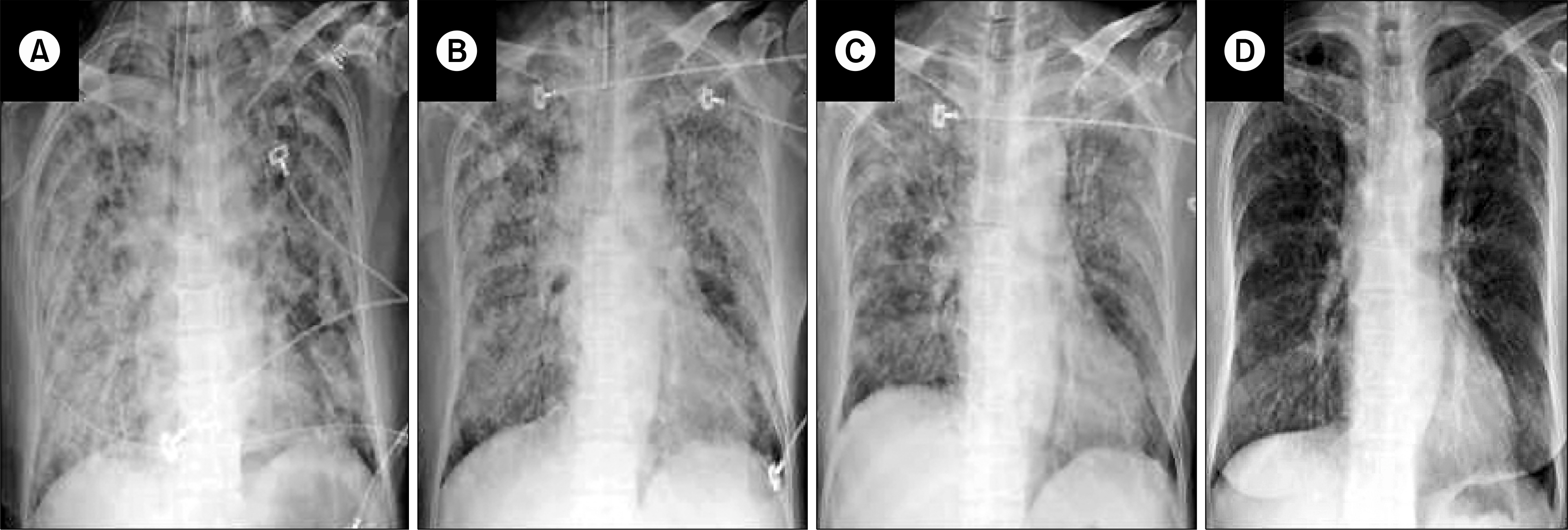
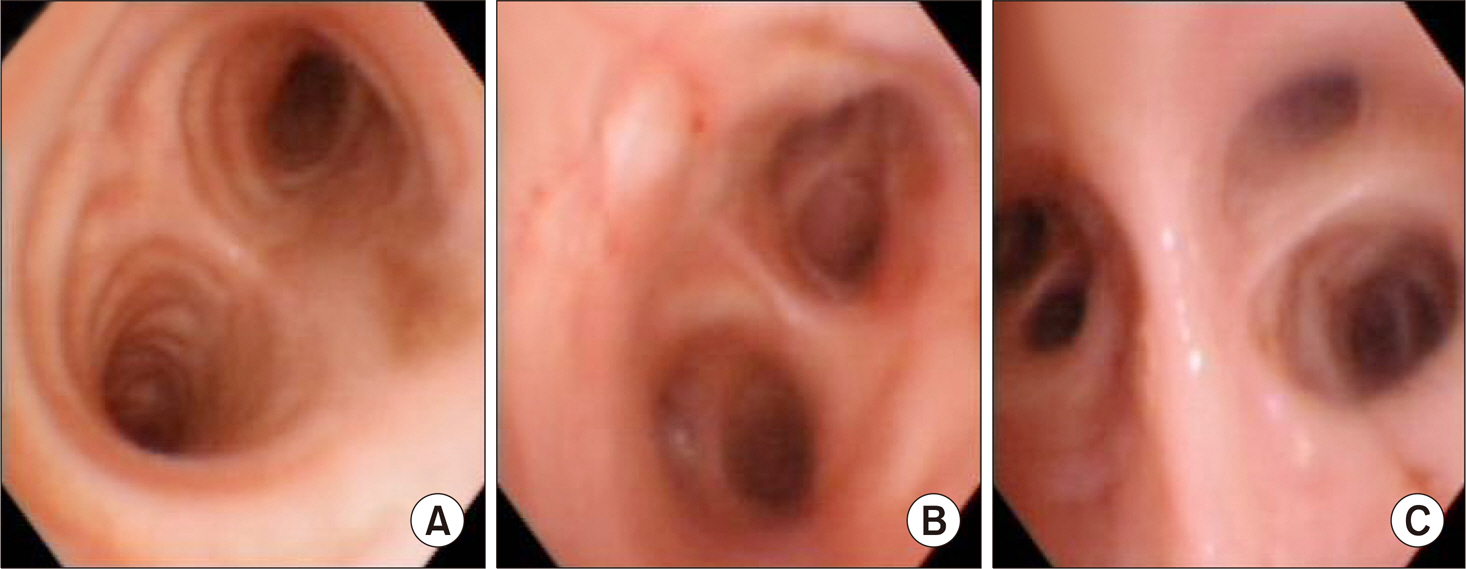
- Diffuse alveolar hemorrhage (DAH) is a life-threatening condition associated with many disorders. Here, we report a case of 59-year-old female who had diffuse alveolar hemorrhage associated with methimazole. She had been treated with methimazole for two weeks due to the recurrence of Grave's disease, before visiting the emergency room. She had to be intubated on the 3rd day of hospitalization because of unabated massive hemoptysis and rapid progression of diffuse alveolar infiltration on chest radiographs. Since her clinical condition improved substantially after cessation of methimazole and steroid pulse therapy, she was extubated on the 9th day of hospitalization and then discharged. After discharge, DAH did not recur with cessation of steroid and she had radioactive iodine therapy for her Grave's disease. This was a rare and interesting case of life-threatening DAH associated with cytoplasmic-antineutrophil cytoplasmic antibody and methimazole.
MeSH Terms
Figure
Reference
-
1. Green RJ, Ruoss SJ, Kraft SA, Duncan SR, Berry GJ, Raffin TA. Pulmonary capillaritis and alveolar hemorrhage. Update on diagnosis and management. Chest. 1996; 110:1305–16.2. Cordier JF, Cottin V. Alveolar hemorrhage in vasculitis: primary and secondary. Semin Respir Crit Care Med. 2011; 32:310–21.
Article3. Primack SL, Miller RR, Müller NL. Diffuse pulmonary hemorrhage: clinical, pathologic, and imaging features. AJR Am J Roentgenol. 1995; 164:295–300.
Article4. Lara AR, Schwarz MI. Diffuse alveolar hemorrhage. Chest. 2010; 137:1164–71.
Article5. Specks U. Diffuse alveolar hemorrhage syndromes. Curr Opin Rheumatol. 2001; 13:12–7.
Article6. Lau EY, So SY, Chan E, Kwok J, Ma J, Kung AW. Methimazole-induced antineutrophil cytoplasmic anti-body-associated diffuse alveolar haemorrhage in a Chinese woman with Graves' disease. Hong Kong Med J. 2009; 15:209–12.7. Gunton JE, Stiel J, Clifton-Bligh P, Wilmshurst E, McElduff A. Prevalence of positive anti-neutrophil cytoplasmic anti-body (ANCA) in patients receiving anti-thyroid medication. Eur J Endocrinol. 2000; 142:587.
Article8. Colby TV, Fukuoka J, Ewaskow SP, Helmers R, Leslie KO. Pathologic approach to pulmonary hemorrhage. Ann Diagn Pathol. 2001; 5:309–19.
Article9. De Lassence A, Fleury-Feith J, Escudier E, Beaune J, Bernaudin JF, Cordonnier C. Alveolar hemorrhage. Diagnostic criteria and results in 194 immunocompromised hosts. Am J Respir Crit Care Med. 1995; 151:157–63.
Article10. Tsai MH, Chang YL, Wu VC, Chang CC, Huang TS. Methimazole-induced pulmonary hemorrhage associated with antimyeloperoxidase-antineutrophil cytoplasmic anti-body: a case report. J Formos Med Assoc. 2001; 100:772–5.11. Katayama K, Hata C, Kagawa K, Noda M, Nakamura K, Shimizu H, et al. Diffuse alveolar hemorrhage associated with myeloperoxidase-antineutrophil cytoplasmic antibody induced by propylthiouracil therapy. Respiration. 2002; 69:473.
Article12. Bonaci-Nikolic B, Nikolic MM, Andrejevic S, Zoric S, Bukilica M. Antineutrophil cytoplasmic antibody (ANCA)-associated autoimmune diseases induced by antithyroid drugs: comparison with idiopathic ANCA vasculitides. Arthritis Res Ther. 2005; 7:R1072–81.13. Keller SF, Miloslavsky EM. Corticosteroids in antineutrophil cytoplasmic antibody-associated vasculitis. Rheum Dis Clin North Am. 2016; 42:91–101.
Article14. Holguin F, Ramadan B, Gal AA, Roman J. Prognostic factors for hospital mortality and ICU admission in patients with ANCA-related pulmonary vasculitis. Am J Med Sci. 2008; 336:321–6.
Article15. de Prost N, Parrot A, Picard C, Ancel PY, Mayaud C, Fartoukh M, et al. Diffuse alveolar haemorrhage: factors associated with in-hospital and long-term mortality. Eur Respir J. 2010; 35:1303–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Antineutrophil Cytoplasmic Antibody (ANCA) Positive, Propylthiouracil-Induced Diffuse Alveolar Hemorrhage in Graves' Disease
- Methimazole-Induced Anti-Neutrophil Cytoplasmic Antibody-Associated Vasculitis in the Peripheral Nerves
- Diffuse Alveolar Hemorrhage
- Orbital Apex Syndrome with Perinuclear Anti-neutrophil Cytoplasmic Antibody-associated Pachymeningitis
- Diffuse Alveolar Hemorrhage Associated with Antineutrophil Cytoplasmic Antibody levels in a Pregnant Woman Taking Propylthiouracil