Investig Clin Urol.
2017 May;58(3):192-199. 10.4111/icu.2017.58.3.192.
Thulium laser vaporesection of the prostate: Can we operate without interrupting oral antiplatelet/anticoagulant therapy?
- Affiliations
-
- 1Department of Urology, Marmara University School of Medicine, Istanbul, Turkey. dr.emresener@gmail.com
- 2Department of Human Pathology, Section of Urology, University of Messina, Messina, Italy.
- 3Department of Urology, Asklepios Hospital Barmbek, Hamburg, Germany.
- 4Department of Urology, Emergency County Hospital, Pius Branzeu, Timisoara, Romania.
- KMID: 2388064
- DOI: http://doi.org/10.4111/icu.2017.58.3.192
Abstract
- PURPOSE
Thulium vaporesection of the prostate (ThuVARP) is a new and safe approach for patients receiving anticoagulant therapy in whom transurethral resection of the prostate (TURP) may possess a high bleeding risk. We aimed to demonstrate the efficacy and safety of ThuVARP in patients receiving oral antiplatelet/anticoagulant (OAP/OAC) therapy.
MATERIALS AND METHODS
A total of 103 patients who underwent ThuVARP between 2011 and 2013 were enrolled in the study. Patients were divided into 2 groups. Group A consisted of 47 patients who underwent low molecular weight heparin (LMWH) bridging and group B consisted of 56 patients who were operated on while receiving OAP/OAC therapy.
RESULTS
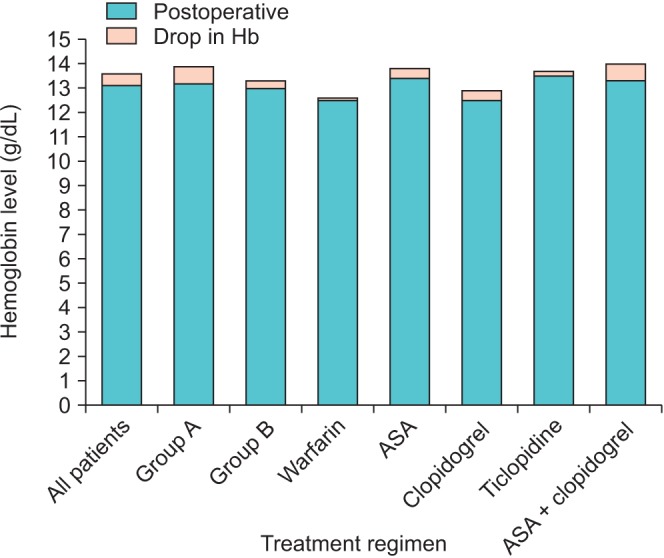
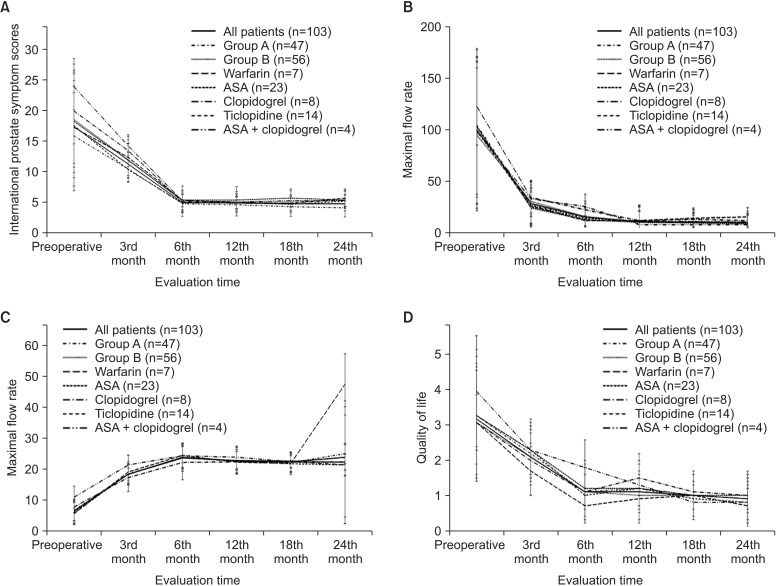
The drop in hemoglobin levels in the pre- and postoperative periods was significantly higher in group A than in group B. When subgroups were analyzed, the mean drop in hemoglobin was significantly lower in the warfarin and ticlopidine subgroups of group B than in group A. International Prostate Symptom Scores were significantly lower 3, 12, 18, and 24 months after surgery in group A than in group B. Quality of life scores, maximal flow rate values, and postmicturition residual urine volumes (mL) were similar between the 2 groups. A total of 38 and 41 patients in groups A and B, respectively, had no complications.
CONCLUSIONS
Our study showed the safety profile of continuing different OAP/OAC therapies in terms of bleeding problems in patients undergoing ThuVARP. We strongly recommend abandoning LMWH bridging and maintaining the OAP/OAC regimen patients are already receiving.
Keyword
MeSH Terms
Figure
Reference
-
1. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol. 2006; 50:969–979. PMID: 16469429.
Article2. Macchione L, Mucciardi G, Gali' A, Di Benedetto A, Butticè S, Magno C. Efficacy and safety of prostate vaporesection using a 120-W 2-μm continuous-wave Tm:YAG laser (RevoLix 2) in patients on continuous oral anticoagulant or antiplatelet therapy. Int Urol Nephrol. 2013; 45:1545–1551. PMID: 23892531.
Article3. Rieken M, Ebinger Mundorff N, Bonkat G, Wyler S, Bachmann A. Complications of laser prostatectomy: a review of recent data. World J Urol. 2010; 28:53–62. PMID: 20052586.
Article4. Herrmann TR, Bach T, Imkamp F, Georgiou A, Burchardt M, Oelke M, et al. Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support. Introduction of a novel technique for the treatment of benign prostatic obstruction. World J Urol. 2010; 28:45–51. PMID: 20063164.
Article5. Fu WJ, Zhang X, Yang Y, Hong BF, Gao JP, Cai W, et al. Comparison of 2-microm continuous wave laser vaporesection of the prostate and transurethral resection of the prostate: a prospective nonrandomized trial with 1-year follow-up. Urology. 2010; 75:194–199. PMID: 19819535.6. Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol. 2015; 67:1066–1096. PMID: 24972732.
Article7. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014; 12:1495–1499. PMID: 25046131.
Article8. Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU Guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015; 67:1099–1109. PMID: 25613154.
Article9. Reich O, Bachmann A, Siebels M, Hofstetter A, Stief CG, Sulser T. High power (80 W) potassium-titanyl-phosphate laser vaporization of the prostate in 66 high risk patients. J Urol. 2005; 173:158–160. PMID: 15592063.
Article10. Capodanno D, Musumeci G, Lettieri C, Limbruno U, Senni M, Guagliumi G, et al. Impact of bridging with perioperative low-molecular-weight heparin on cardiac and bleeding outcomes of stented patients undergoing non-cardiac surgery. Thromb Haemost. 2015; 114:423–431. PMID: 26017898.
Article11. Rose AJ, Allen AL, Minichello T. A call to reduce the use of bridging anticoagulation. Circ Cardiovasc Qual Outcomes. 2016; 9:64–67. PMID: 26715651.
Article12. Taylor K, Filgate R, Guo DY, Macneil F. A retrospective study to assess the morbidity associated with transurethral prostatectomy in patients on antiplatelet or anticoagulant drugs. BJU Int. 2011; 108(Suppl 2):45–50. PMID: 22085127.
Article13. Dotan ZA, Mor Y, Leibovitch I, Varon D, Golomb J, Duvdevani M, et al. The efficacy and safety of perioperative low molecular weight heparin substitution in patients on chronic oral anticoagulant therapy undergoing transurethral prostatectomy for bladder outlet obstruction. J Urol. 2002; 168:610–613. PMID: 12131319.
Article14. Parr NJ, Loh CS, Desmond AD. Transurethral resection of the prostate and bladder tumour without withdrawal of warfarin therapy. Br J Urol. 1989; 64:623–625. PMID: 2627636.
Article15. Ong WL, Koh TL, Fletcher J, Gruen R, Royce P. Perioperative management of antiplatelets and anticoagulants among patients undergoing elective transurethral resection of the prostate: a single institution experience. J Endourol. 2015; 29:1321–1327. PMID: 26154769.16. Pariser JJ, Famakinwa OJ, Pearce SM, Chung DE. High-power thulium laser vaporization of the prostate: short-term outcomes of safety and effectiveness. J Endourol. 2014; 28:1357–1362. PMID: 24936718.
Article17. Vincent MW, Gilling PJ. HoLEP has come of age. World J Urol. 2015; 33:487–493. PMID: 25416347.
Article18. Berger J, Robert G, Descazeaud A. Laser treatment of benign prostatic hyperplasia in patients on oral anticoagulant therapy. Curr Urol Rep. 2010; 11:236–241. PMID: 20461480.
Article19. Hirayama T, Shitara T, Fujita T, Iwamura M, Kubo S, Baba S. Holmium laser enucleation of the prostate (HoLEP) in patients with continuous oral anticoagulation: first reported cases in Japan. Nihon Hinyokika Gakkai Zasshi. 2010; 101:754–757. PMID: 21174742.
Article20. Chung DE, Wysock JS, Lee RK, Melamed SR, Kaplan SA, Te AE. Outcomes and complications after 532 nm laser prostatectomy in anticoagulated patients with benign prostatic hyperplasia. J Urol. 2011; 186:977–981. PMID: 21791350.
Article21. Ruszat R, Wyler S, Forster T, Reich O, Stief CG, Gasser TC, et al. Safety and effectiveness of photoselective vaporization of the prostate (PVP) in patients on ongoing oral anticoagulation. Eur Urol. 2007; 51:1031–1038. PMID: 16945475.
Article22. Bach T, Huck N, Wezel F, Häcker A, Gross AJ, Michel MS. 70 vs 120 W thulium:yttrium-aluminium-garnet 2 microm continuous-wave laser for the treatment of benign prostatic hyperplasia: a systematic ex-vivo evaluation. BJU Int. 2010; 106:368–372. PMID: 19912204.23. Bach T, Herrmann TR, Ganzer R, Burchardt M, Gross AJ. RevoLix vaporesection of the prostate: initial results of 54 patients with a 1-year follow-up. World J Urol. 2007; 25:257–262. PMID: 17530258.
Article24. Netsch C, Magno C, Buttice S, Macchione L, Mucciardi G, Herrmann TR, et al. Thulium vaporesection of the prostate and thulium vapoenucleation of the prostate in patients on oral anticoagulants: a retrospective three-centre matched-paired comparison. Urol Int. 2016; 96:421–426. PMID: 27197739.
Article25. Roehrborn CG, McConnell J, Bonilla J, Rosenblatt S, Hudson PB, Malek GH, et al. Serum prostate specific antigen is a strong predictor of future prostate growth in men with benign prostatic hyperplasia. PROSCAR long-term efficacy and safety study. J Urol. 2000; 163:13–20. PMID: 10604304.26. Roehrborn CG, Boyle P, Bergner D, Gray T, Gittelman M, Shown T, et al. Serum prostate-specific antigen and prostate volume predict long-term changes in symptoms and flow rate: results of a four-year, randomized trial comparing finasteride versus placebo. PLESS Study Group. Urology. 1999; 54:662–669. PMID: 10510925.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of 5α-reductase inhibitors on the efficiency of thulium:yttrium-aluminium-garnet (RevoLix®) vaporesection for treating benign prostatic hyperplasia
- An Analytical Comparison of Short-term Effectiveness and Safety Between Thulium:YAG Laser Vaporesection of the Prostate and Bipolar Transurethral Resection of the Prostate in Patients With Benign Prostatic Hyperplasia
- Recent advances in laser treatment for benign prostatic hyperplasia
- A novel one lobe technique of thulium laser enucleation of the prostate: 'All-in-One' technique
- The Role of Novel Oral Anticoagulants and Antiplatelet Therapy after Percutaneous Coronary Intervention: Individualizing Therapy to Optimize Outcomes