Investig Clin Urol.
2020 Jan;61(1):67-74. 10.4111/icu.2020.61.1.67.
Effect of 5α-reductase inhibitors on the efficiency of thulium:yttrium-aluminium-garnet (RevoLix®) vaporesection for treating benign prostatic hyperplasia
- Affiliations
-
- 1Department of Urology, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 2Department of Urology, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. prosdoc@hanmail.net
- 3Department of Urology, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2466794
- DOI: http://doi.org/10.4111/icu.2020.61.1.67
Abstract
- PURPOSE
Preoperative use of 5α-reductase inhibitors (5ARIs) may cause fibrosis of the prostate tissue and reduce the efficiency of thulium laser surgery for treating benign prostate hyperplasia (BPH). Thus, we investigated the effects of preoperative 5ARI use in this setting.
MATERIALS AND METHODS
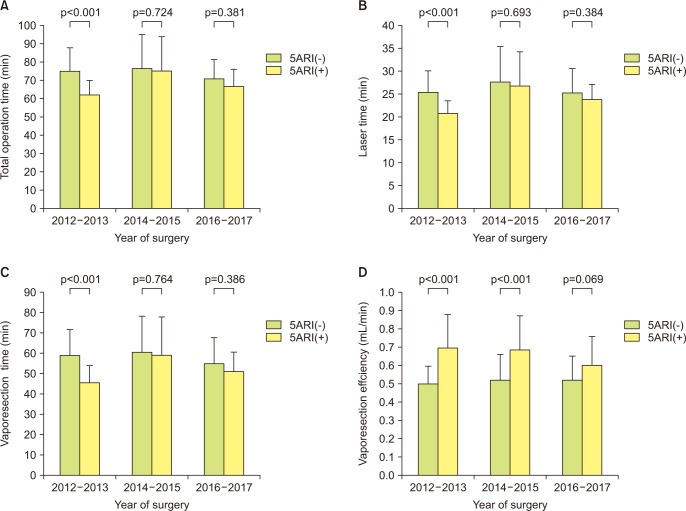
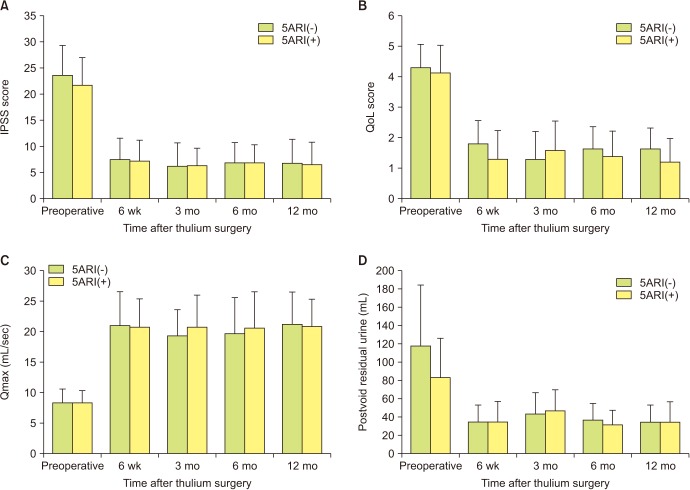
This retrospective study examined 184 patients who underwent thulium laser surgery for BPH during 2012-2017. Patients were grouped according to their 5ARI use in order to compare their preoperative and intraoperative characteristics and subsequent outcomes. Surgical efficiency was assessed using vaporesection efficiency. The total operation time, vaporesection time and prostate volume change were measured.
RESULTS
The 5ARI+ group included 83 patients (45.1%) and the 5ARI− group included 101 patients (54.9%). There were no significant differences in the two groups' preoperative characteristics, postoperative prostate size, thulium laser energy use, or prostate volume reduction rate. However, relative to the 5ARI− group, the 5ARI+ group had a significant shorter total operative time (65.0 min vs. 70.0 min, p=0.013) and a significantly shorter vaporesection time (48.0 min vs. 54.0 min, p=0.014), which resulted in significantly higher vaporesection efficiency in the 5ARI+ group (0.66 mL/min vs. 0.51 mL/min, p < 0.001). Both groups exhibit significant improvements in their quality of life score and International Prostate Symptom Score during the 12-month follow-up.
CONCLUSIONS
In contrast with our expectations, the preoperative use of 5ARI increased the efficiency of thulium laser surgery for BPH. Thus, it may not be necessary to stop 5ARI treatment before performing thulium laser surgery in this setting.
MeSH Terms
Figure
Reference
-
1. Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol. 2015; 67:1066–1096. PMID: 24972732.
Article2. Gravas S, Bachmann A, Reich O, Roehrborn CG, Gilling PJ, De La Rosette J. Critical review of lasers in benign prostatic hyperplasia (BPH). BJU Int. 2011; 107:1030–1043. PMID: 21438974.
Article3. Xia SJ, Zhuo J, Sun XW, Han BM, Shao Y, Zhang YN. Thulium laser versus standard transurethral resection of the prostate: a randomized prospective trial. Eur Urol. 2008; 53:382–389. PMID: 17566639.
Article4. Gross AJ, Netsch C, Knipper S, Hölzel J, Bach T. Complications and early postoperative outcome in 1080 patients after thulium vapoenucleation of the prostate: results at a single institution. Eur Urol. 2013; 63:859–867. PMID: 23245687.
Article5. Kim HK, Zhao C, Choi BR, Chae HJ, Kim DS, Park JK. Is transforming growth factor-β signaling activated in human hypertrophied prostate treated by 5-alpha reductase inhibitor? Dis Markers. 2013; 35:679–685. PMID: 24311892.6. Hochberg DA, Basillote JB, Armenakas NA, Vasovic L, Shevchuk M, Pareek G, et al. Decreased suburethral prostatic microvessel density in finasteride treated prostates: a possible mechanism for reduced bleeding in benign prostatic hyperplasia. J Urol. 2002; 167:1731–1733. PMID: 11912398.
Article7. Sato R, Sadaoka Y, Nishio K, Kobori Y, Yagi H, Arai G, et al. Effects of preoperative dutasteride treatment in holmium laser enucleation of the prostate. Int J Urol. 2015; 22:385–388. PMID: 25631165.
Article8. Donohue JF, Sharma H, Abraham R, Natalwala S, Thomas DR, Foster MC. Transurethral prostate resection and bleeding: a randomized, placebo controlled trial of role of finasteride for decreasing operative blood loss. J Urol. 2002; 168:2024–2026. PMID: 12394700.
Article9. Hahn RG, Fagerström T, Tammela TL, Van Vierssen Trip O, Beisland HO, Duggan A, et al. Blood loss and postoperative complications associated with transurethral resection of the prostate after pretreatment with dutasteride. BJU Int. 2007; 99:587–594. PMID: 17407516.
Article10. Kravchick S, Cytron S, Mamonov A, Peled R, Linov L. Effect of short-term dutasteride therapy on prostate vascularity in patients with benign prostatic hyperplasia: a pilot study. Urology. 2009; 73:1274–1278. PMID: 19375786.
Article11. Pastore AL, Mariani S, Barrese F, Palleschi G, Valentini AM, Pacini L, et al. Transurethral resection of prostate and the role of pharmacological treatment with dutasteride in decreasing surgical blood loss. J Endourol. 2013; 27:68–70. PMID: 23030716.
Article12. Araki M, Lam PN, Culkin DJ, Wong C. Decreased efficiency of potassium-titanyl-phosphate laser photoselective vaporization prostatectomy with long-term 5 alpha-reductase inhibition therapy: is it true? Urology. 2007; 70:927–930. PMID: 18068449.
Article13. Bepple JL, Barone BB, Eure G. The effect of dutasteride on the efficacy of photoselective vaporization of the prostate: results of a randomized, placebo-controlled, double-blind study (DOP trial). Urology. 2009; 74:1101–1104. PMID: 19800668.
Article14. Strom KH, Gu X, Spaliviero M, Wong C. The effects of 5α-reductase inhibition on benign prostatic hyperplasia treated by photoselective vaporization prostatectomy with the 120 Watt GreenLight HPS laser system. J Am Coll Surg. 2011; 212:244–250. PMID: 21183365.
Article15. Warner JN, Nunez RN, Tyson MD, Viprakasit DP, Miller NL, Humphreys MR. A multiinstitutional study of the effects of medical therapy for lower urinary symptoms on the perioperative outcomes of holmium laser enucleation of the prostate. Urology. 2011; 78:1385–1390. PMID: 21871654.
Article16. Monn MF, El Tayeb M, Bhojani N, Mellon MJ, Sloan JC, Boris RS, et al. Predictors of enucleation and morcellation time during holmium laser enucleation of the prostate. Urology. 2015; 86:338–342. PMID: 26189134.
Article17. Dimopoulos P, Christopoulos P, Kampantais S. A focused review on the effects of preoperative 5α-reductase inhibitors treatment in patients undergoing holmium laser enucleation of the prostate: what do we know so far? J Endourol. 2018; 32:79–83. PMID: 29161905.
Article18. Herrmann TR, Bach T, Imkamp F, Georgiou A, Burchardt M, Oelke M, et al. Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support. Introduction of a novel technique for the treatment of benign prostatic obstruction. World J Urol. 2010; 28:45–51. PMID: 20063164.
Article19. Bach T, Xia SJ, Yang Y, Mattioli S, Watson GM, Gross AJ, et al. Thulium: YAG 2 mum cw laser prostatectomy: where do we stand? World J Urol. 2010; 28:163–168. PMID: 20204378.20. Sandfeldt L, Bailey DM, Hahn RG. Blood loss during transurethral resection of the prostate after 3 months of treatment with finasteride. Urology. 2001; 58:972–976. PMID: 11744471.
Article21. McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Dixon CM, Kusek JW, et al. Medical Therapy of Prostatic Symptoms (MTOPS). The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003; 349:2387–2398. PMID: 14681504.
Article22. Kearney MC, Bingham J, Bergland R, Meade-D'Alisera P, Puchner PJ. Clinical predictors in the use of finasteride for control of gross hematuria due to benign prostatic hyperplasia. J Urol. 2002; 167:2489–2491. PMID: 11992064.
Article23. Pareek G, Shevchuk M, Armenakas NA, Vasovic L, Hochberg DA, Basillote JB, et al. The effect of finasteride on the expression of vascular endothelial growth factor and microvessel density: a possible mechanism for decreased prostatic bleeding in treated patients. J Urol. 2003; 169:20–23. PMID: 12478093.
Article24. Sutton MT, Yingling M, Vyas A, Atiemo H, Borkowski A, Jacobs SC, et al. Finasteride targets prostate vascularity by inducing apoptosis and inhibiting cell adhesion of benign and malignant prostate cells. Prostate. 2006; 66:1194–1202. PMID: 16652387.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Analytical Comparison of Short-term Effectiveness and Safety Between Thulium:YAG Laser Vaporesection of the Prostate and Bipolar Transurethral Resection of the Prostate in Patients With Benign Prostatic Hyperplasia
- The Effect of 5-alpha Reductase Inhibitors on the Efficacy of Photoselective Vaporization of the Prostate with 120 W GreenLight HPS Laser
- Finasteride and Erectile Dysfunction in Patients with Benign Prostatic Hyperplasia or Male Androgenetic Alopecia
- Treatment of Diffuse Planar Xanthoma of the Face after One Session of 1,444-nm Neodymium-Doped Yttrium Aluminium Garnet Laser
- Recent advances in laser treatment for benign prostatic hyperplasia