J Korean Neurosurg Soc.
2017 Jul;60(4):448-455. 10.3340/jkns.2015.0505.010.
Magnetic Resonance Imaging Patterns of Post-Operative Spinal Infection: Relationship between the Clinical Onset of Infection and the Infection Site
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shlee@amc.seoul.kr
- 2Department of Radiology, Myongji Hospital, Seonam University College of Medicine, Goyang, Korea.
- 3Department of Neurosurgery, School of Medicine, Kangwon National University, Chuncheon, Korea.
- KMID: 2387883
- DOI: http://doi.org/10.3340/jkns.2015.0505.010
Abstract
OBJECTIVE
To investigate the magnetic resonance imaging (MRI) findings and the patterns of postoperative spinal infection according to the passage of time.
METHODS
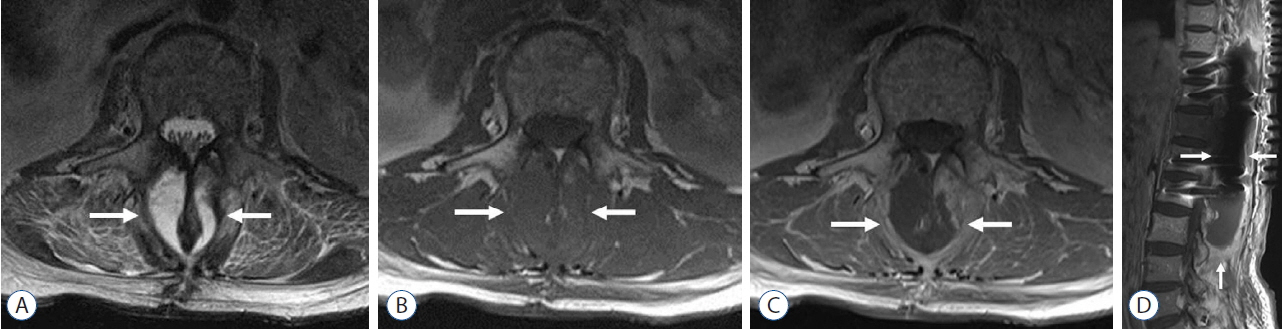
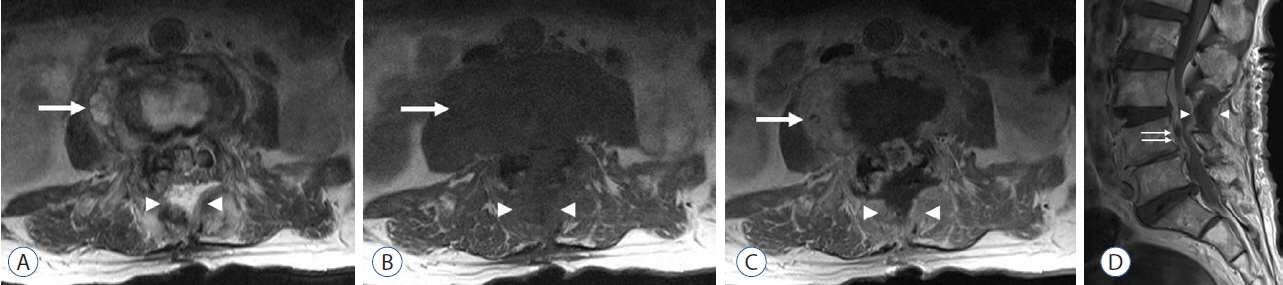
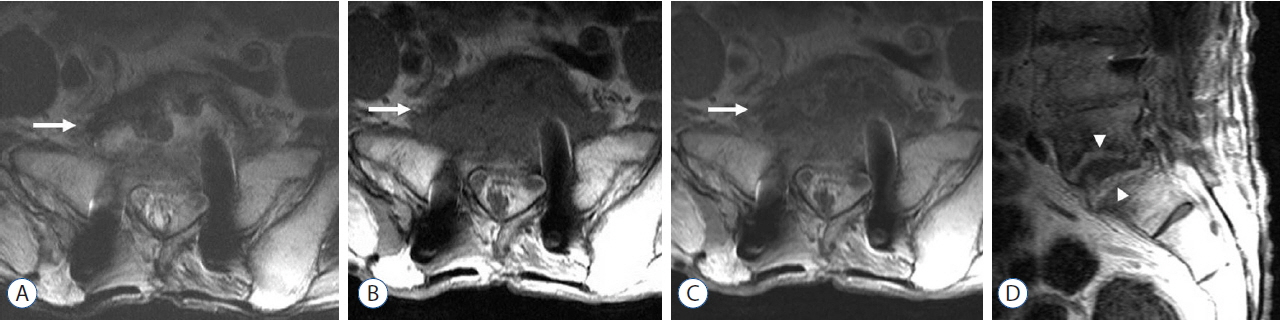
Institutional review board approval was obtained, and informed consent was not obtained for the retrospective review of patients' medical records. A total of 43 patients (27 men and 16 women; mean age, 64) diagnosed with postoperative spinal infection were included in this study. We retrospectively reviewed the MRI findings and the medical records and categorized the infection sites based on MRI, i.e., anterior, posterior, and both parts. The duration of the clinical onset from surgery was divided, i.e., acute (≤2 weeks), subacute (2-4 weeks), and late (>4 weeks).
RESULTS
Postoperative spinal infection was involved in the posterior part in 31 (72%), anterior part in two (4.7%), and both parts in 10 patients (23.3%). Abscess or phlegmon in the back muscles and laminectomy site were the most common MRI findings. The number of patients with acute, subacute, and late clinical onset were 35, two, and six, respectively (mean, 33.4 days; range, 1-730 days). The mean duration of the clinical onset was 12 days in the posterior part, 15.2 days in both parts, and 456.5 days in the anterior part.
CONCLUSION
Postoperative spinal infection usually occurred within four weeks in the posterior part and over time the infection was considered to spread into the anterior part. For the evaluation of postoperative spinal infection, the posterior surgical field was more important than the vertebral body or the disc space on MRI.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Boden SD, Davis DO, Dina TS, Sunner JL, Wiesel SW. Postoperative diskitis: distinguishing early MR imaging findings from normal postoperative disk space changes. Radiology. 184:765–771. 1992.
Article2. Bose B. Delayed infection after instrumented spine surgery: case reports and review of the literature. Spine J. 3:394–399. 2003.
Article3. Chaudhary SB, Vives MJ, Basra SK, Reiter MF. Postoperative spinal wound infections and postprocedural diskitis. J Spinal Cord Med. 30:441–451. 2007.
Article4. Clark CE, Shufflebarger HL. Late-developing infection in instrumented idiopathic scoliosis. Spine (Phila Pa 1976). 24:1909–1912. 1999.
Article5. Collins I, Wilson-MacDonald J, Chami G, Burgoyne W, Vineyakam P, Berendt T, et al. The diagnosis and management of infection following instrumented spinal fusion. Eur Spine J. 17:445–450. 2008.
Article6. Djukic S, Genant HK, Helms CA, Holt RG. Magnetic resonance imaging of the postoperative lumbar spine. Radiol Clin North Am. 28:341–360. 1990.7. Djukic S, Vahlensieck M, Resendes M, Genant HK. The lumbar spine: postoperative magnetic resonance imaging. Bildgebung. 59:136–146. 1992.8. Dufour V, Feydy A, Rillardon L, Redondo A, Le Page L, Bert F, et al. Comparative study of postoperative and spontaneous pyogenic spondylodiscitis. Semin Arthritis Rheum. 34:766–771. 2005.
Article9. Fang A, Hu SS, Endres N, Bradford DS. Risk factors for infection after spinal surgery. Spine (Phila Pa 1976). 30:1460–1465. 2005.
Article10. Hall KK, Lyman JA. Updated review of blood culture contamination. Clin Microbiol Rev. 19:788–802. 2006.
Article11. Hamdan TA. Postoperative disc space infection after discectomy: a report on thirty-five patients. Int Orthop. 36:445–450. 2012.
Article12. Hedin G. Staphylococcus epidermidis--hospital epidemiology and the detection of methicillin resistance. Scand J Infect Dis Suppl. 90:1–59. 1993.13. Kowalski TJ, Layton KF, Berbari EF, Steckelberg JM, Huddleston PM, Wald JT, et al. Follow-up MR imaging in patients with pyogenic spine infections: lack of correlation with clinical features. AJNR Am J Neuroradiol. 28:693–699. 2007.14. Levi AD, Dickman CA, Sonntag VK. Management of postoperative infections after spinal instrumentation. J Neurosurg. 86:975–980. 1997.
Article15. Massie JB, Heller JG, Abitbol JJ, McPherson D, Garfin SR. Postoperative posterior spinal wound infections. Clin Orthop Relat Res. (284):99–108. 1992.
Article16. Pull ter Gunne AF, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976). 34:1422–1428. 2009.
Article17. Pull ter Gunne AF, Mohamed AS, Skolasky RL, van Laarhoven CJ, Cohen DB. The presentation, incidence, etiology, and treatment of surgical site infections after spinal surgery. Spine (Phila Pa 1976). 35:1323–1328. 2010.
Article18. Van Goethem JW, Parizel PM, van den Hauwe L, Van de Kelft E, Verlooy J, De Schepper AM. The value of MRI in the diagnosis of postoperative spondylodiscitis. Neuroradiology. 42:580–585. 2000.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Paraplegia Caused by Infection Extending to Spine Due to Aspergillosis: A Case Report
- High Prevalence of Multifocal Spine Infections Involving the Cervical and Thoracic Regions: A Case for Imaging the Entire Spine
- Effect of the Exchange of Saline Used in Surgical Procedures on Surgical Site Infection
- A Rare Case of Syphilitic Myelitis of the Spinal Cord
- Serratia marcescens Spinal Epidural Abscess Following Caudal Epidural Injection