J Korean Orthop Assoc.
2017 Aug;52(4):359-363. 10.4055/jkoa.2017.52.4.359.
Serratia marcescens Spinal Epidural Abscess Following Caudal Epidural Injection
- Affiliations
-
- 1Department of Orthopedic Surgery, Presbyterian Medical Center, Jeonju, Korea. docby@hanmail.net
- KMID: 2387796
- DOI: http://doi.org/10.4055/jkoa.2017.52.4.359
Abstract
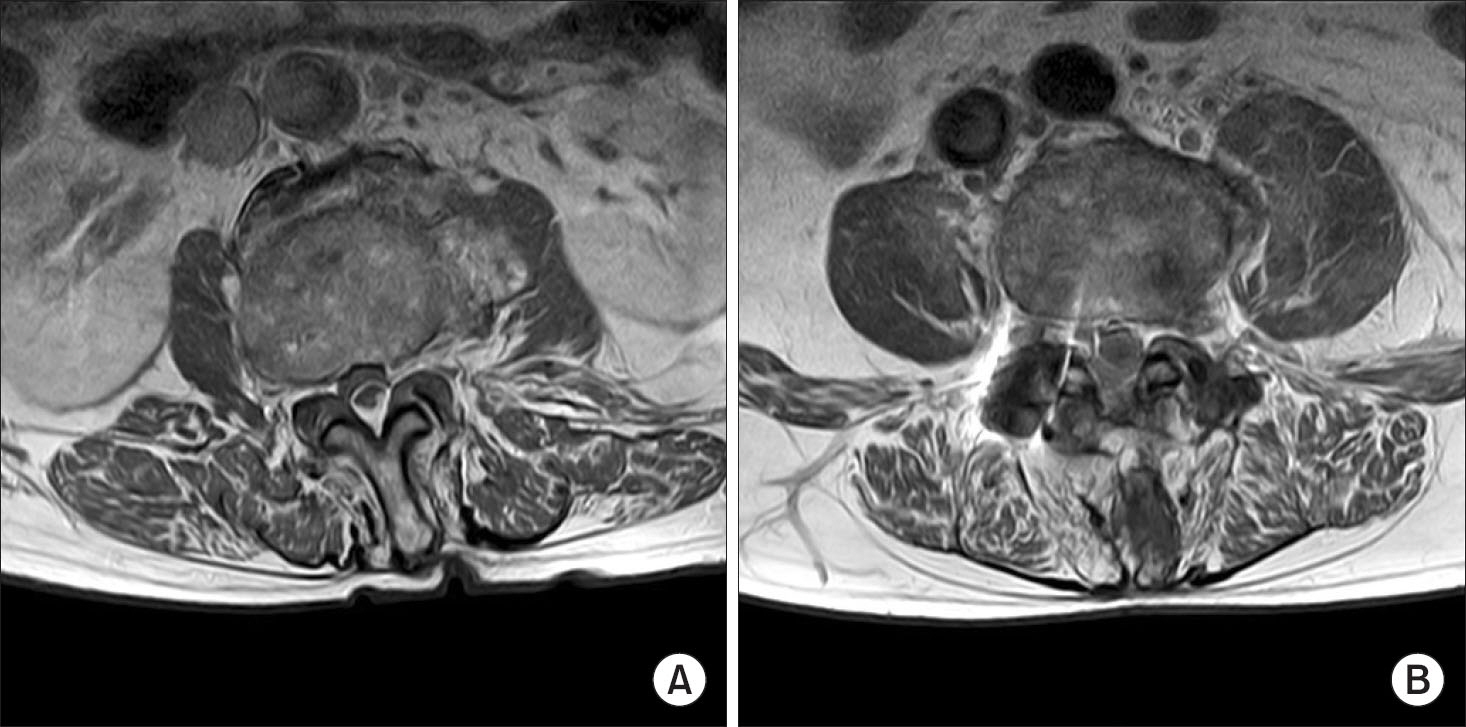
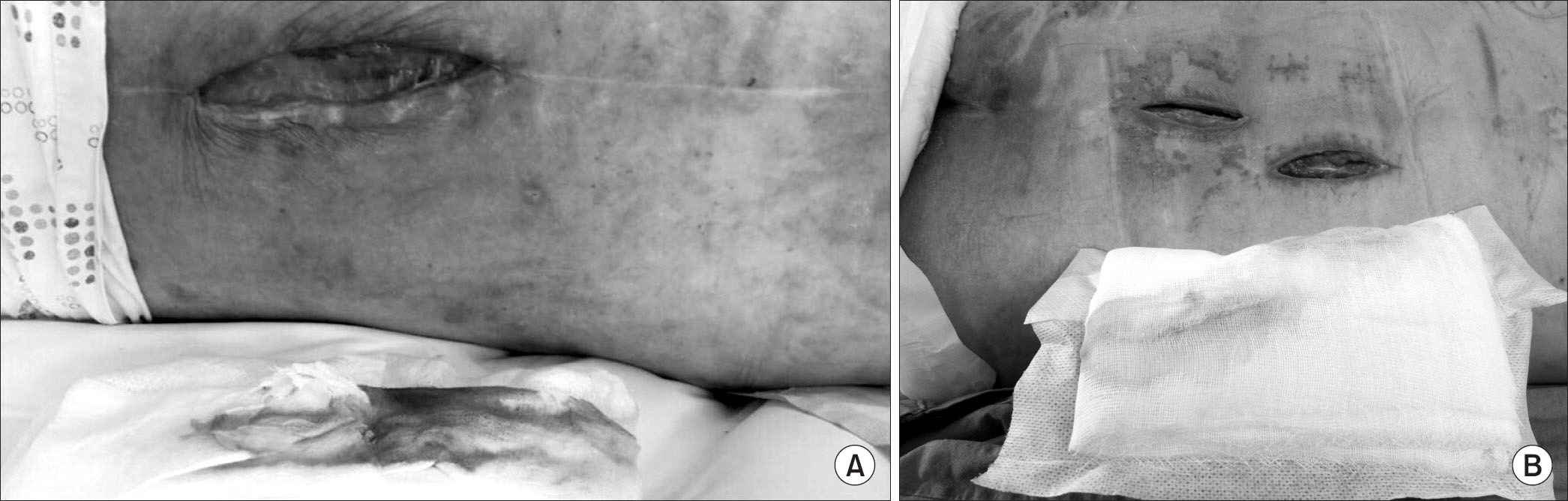
- Spinal infection due to Serratia marcescens is very rare. A 78-year-old male patient withoutany risk factor was admitted to our hospital with chief complaints of severe back pain, fever, weakness in both legs, and bowel dysfunction, following caudal epidural injection. Magnetic resonance imaging revealed spondylodiscitis with epidural abscess. Surgical decompression was performed and the epidural abscess was removed. The cultures isolated S. marcescens, which can cause nosocomial infection in immunocompromised patient. However, to the best of our knowledge, we report the first case of S. marcescens spinal epidural abscess following epidural injection, with literature review.
MeSH Terms
Figure
Reference
-
1. Kim SK, Chung JY. Epidural steroid injection. J Korean Med Assoc. 2014; 57:318–25.
Article2. Rigamonti D, Liem L, Sampath P. . Spinal epidural abscess: contemporary trends in etiology, evaluation, and management. Surg Neurol. 1999; 52:189–96.
Article3. Darouiche RO. Spinal epidural abscess. N Engl J Med. 2006; 355:2012–20.
Article4. Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2000; 23:175–204. discussion 205.
Article5. Soehle M, Wallenfang T. Spinal epidural abscesses: clinical manifestations, prognostic factors, and outcomes. Neurosurgery. 2002; 51:79–85. discussion 86, 7.
Article6. Hadjipavlou AG, Gaitanis IN, Papadopoulos CA, Katonis PG, Kontakis GM. Serratia spondylodiscitis after elective lumbar spine surgery: a report of two cases. Spine (Phila Pa 1976). 2002; 27:E507–12.7. Alfonso Olmos M, Silva González A, Duart Clemente J, Villas Tomé C. Infected vertebroplasty due to uncommon bacteria solved surgically: a rare and threatening life complication of a common procedure: report of a case and a review of the literature. Spine (Phila Pa 1976). 2006; 31:E770–3.8. Weinstein MA, McCabe JP, Cammisa FP Jr. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord. 2000; 13:422–6.
Article9. Perez-Toro MR, Burton AW, Hamid B, Koyyalagunta D. Two-tuohy needle and catheter technique for fluoroscopically guided percutaneous drainage of spinal epidural abscess: a case report. Pain Med. 2009; 10:501–5.
Article10. Huang CR, Lu CH, Chien CC, Chang WN. Protean infectious types and frequent association with neurosurgical procedures in adult Serratia marcescens CNS infections: report of two cases and review of the literature. Clin Neurol Neurosurg. 2001; 103:171–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chronic Spinal Epidural Abscess after Epidural Analgesia: Case Report
- Epidural Abscess and Vertebral Osteomyelitis Induced by Epidural Injection: A case report
- The Effect of Caudal Epidural Injection for the Pseudoclaudication of Spinal Stenosis
- Development of Spinal Epidural Abscess during Treatment of Pneumococcal Meningitis
- Comparison of Transforaminal Epidural Steroid Injection and Lumbar/Caudal Epidural Steroid Injection for the Treatment of Lumbosacral Radiculopathy