J Korean Ophthalmol Soc.
2017 Jul;58(7):763-768. 10.3341/jkos.2017.58.7.763.
The Change of the Pathogen in Cultured Jones Tubes according to the Postoperative Periods
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University School of Medicine, Yangsan, Korea. jongsool@pusan.ac.kr
- 2Department of Ophthalmology, Gyeongsang National University School of Medicine, Jinju, Korea.
- 3Department of Ophthalmology, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- 4Division of International Trade, Silla University College of Global Business, Busan, Korea.
- 5Department of Ophthalmology, Pusan National University Hospital, Busan, Korea.
- KMID: 2387148
- DOI: http://doi.org/10.3341/jkos.2017.58.7.763
Abstract
- PURPOSE
To evaluate the change in pathogens in cultured Jones tubes used in lacrimal bypass surgery according to postoperative period and to provide basic data related to preventive antibiotics or functional lacrimal stent development.
METHODS
Fifty patients who underwent Jones tubes removal were enrolled in this study. Removed Jones tubes were cultured to identify bacteria and were tested for antibiotic sensitivity. The results were further analyzed according to the period between lacrimal bypass surgery and tube removal.
RESULTS
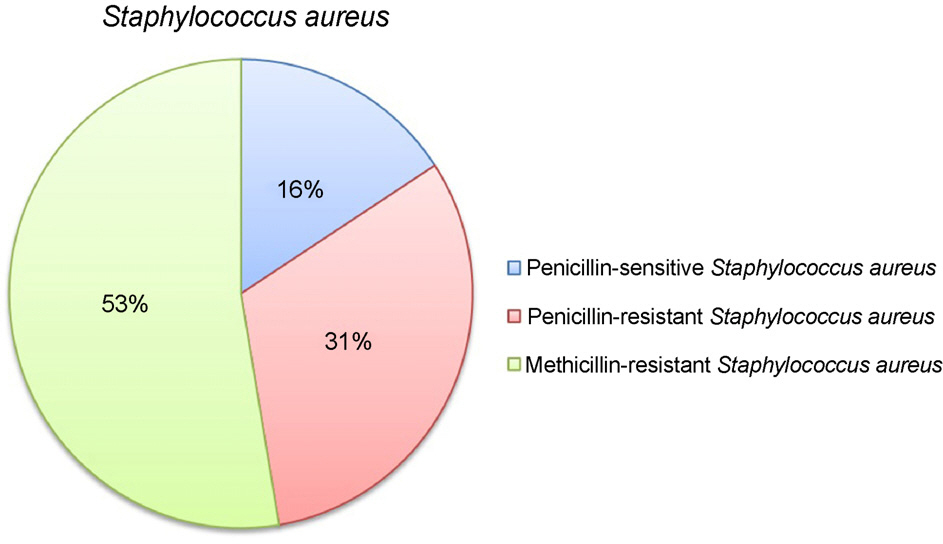
Among 50 cases, 24 (48%) showed cultured bacteria of Staphylococcus aureus, 5 (10%) were Pseudomonas, and another 5 (10%) were Gram-positive bacilli. Although Staphylococcus aureus was the most frequently cultured organism, Proteus mirabilis was the most common cultured organism in patients who underwent tube removal more than 10 years after lacrimal bypass surgery. There was no significant correlation between cultured organism and the period between lacrimal bypass surgery and tube removal. Eighty four percent of cultured Staphylococcus aureus showed resistance to penicillin, and 53% of cultured Staphylococcus aureus showed resistance to methicillin.
CONCLUSIONS
Staphylococcus aureus was the most frequently cultured organism according to Jones tube-related lacrimal bypass surgery. A large proportion of cultured Staphylococcus aureus showed resistance to penicillin and methicillin. Proteus mirabilis should be considered the most common pathogen in patients more than 10 years after lacrimal bypass surgery.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Angrist RC, Dortzbach RK. Silicone intubation for partial and total nasolacrimal duct obstruction in adults. Ophthal Plast Reconstr Surg. 1985; 1:51–4.
Article2. Dortzbach RK, France TD, Kushner BJ, Gonnering RS. Silicone intubation for obstruction of the nasolacrimal duct in children. Am J Ophthalmol. 1982; 94:585–90.
Article3. Tarbet KJ, Custer PL. External dacryocystorhinostomy. Surgical success, patient satisfaction, and economic cost. Ophthalmology. 1995; 102:1065–70.
Article4. Jones LT. The cure of epiphora due to canalicular disorders, trauma and surgical failures on the lacrimal passages. Trans Am Acad Ophthalmol Otolaryngol. 1962; 66:506–24.5. Yoo JR, Choi WC. A survey of post-operative satisfaction in patients with canalicular obstruction after jones tube intubation. J Korean Ophthalmol Soc. 2002; 43:2081–8.6. Ide H, Mollahaliloglu S. How firms set prices for medical materi-als: a multi-country study. Health Policy. 2009; 92:73–8.
Article7. Park SW, Park JM, Lee JE, Lee JS. Results of the cultured jones tubes used in lacrimal bypass surgery. J Korean Ophthalmol Soc. 2006; 47:696–702.8. Lee JS, Oum BS, Lee JE. . Treatment of obstructed lacrimal ap-paratus by Bowman’s probe guided lacrimal bypass surgery. J Korean Ophthalmol Soc. 1999; 40:1746–54.9. Lamping K, Levine MR. Jones’ tubes. How good are they? Arch Ophthalmol. 1983; 101:260–1.
Article10. Welham RA, Guthoff R. The Lester-Jones tube: a 15-year fol-low-up. Graefes Arch Clin Exp Ophthalmol. 1985; 223:106–8.
Article11. Sekhar GC, Dortzbach RK, Gonnering RS, Lemke BN. Problems associated with conjunctivodacryocystorhinostomy. Am J Ophthalmol. 1991; 112:502–6.
Article12. Kim YS, Lee TS. Clinical study conjunctivodacryocystorhinostomy with Jones tube. J Korean Ophthalmol Soc. 1991; 32:129–33.13. Neuhaus RW. Postcataract surgery endophthalmitis in a patient with a functioning Jones tube. Ophthal Plast Reconstr Surg. 1992; 8:208–9.
Article14. Bartley GB. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 3. Ophthal Plast Reconstr Surg. 1993; 9:11–26.15. Steinsapir KD, Glatt HJ, Putterman AM. A 16-year study of con-junctival dacryocystorhinostomy. Am J Ophthalmol. 1990; 109:387–93.
Article16. Lim C, Martin P, Benger R. . Lacrimal canalicular bypass sur-gery with the Lester Jones tube. Am J Ophthalmol. 2004; 137:101–8.
Article17. Hartikainen J, Lehtonen OP, Saari KM. Bacteriology of lacrimal duct obstruction in adults. Br J Ophthalmol. 1997; 81:37–40.
Article18. Nakai H, Hagihara M, Kato H. . Prevalence and risk factors of infections caused by extended-spectrum β-lactamase (ESBL)- pro-ducing Enterobacteriaceae. J Infect Chemother. 2016; 22:319–26.19. Shibasaki M, Komatsu M, Sueyoshi N. . Community spread of extended-spectrum β-lactamase-producing bacteria detected in so-cial insurance hospitals throughout Japan. J Infect Chemother. 2016; 22:395–9.
Article20. Burall LS, Harro JM, Li X. . Proteus mirabilis genes that con-tribute to pathogenesis of urinary tract infection: identification of 25 signature-tagged mutants attenuated at least 100-fold. Infect Immun. 2004; 72:2922–38.21. Coker C, Poore CA, Li X, Mobley HL. Pathogenesis of Proteus mirabilis urinary tract infection. Microbes Infect. 2000; 2:1497–505.22. Shin H, Price K, Albert L. . Changes in the eye microbiota as-sociated with contact lens wearing. MBio. 2016; 7:e00198.
Article23. Park JH, Song HY, Shin JH. . Polydioxanone biodegradable stent placement in a canine urethral model: analysis of in-flammatory reaction and biodegradation. J Vasc Interv Radiol. 2014; 25:1257–64.e1.
Article24. Li G, Li Y, Lan P. . Biodegradable weft-knitted intestinal stents: fabrication and physical changes investigation in vitro degradation. J Biomed Mater Res A. 2014; 102:982–90.
Article25. Zamiri P, Kuang Y, Sharma U. . The biocompatibility of rap-idly degrading polymeric stents in porcine carotid arteries. Biomaterials. 2010; 31:7847–55.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Results of the Cultured Jones Tubes Used in Lacrimal Bypass Surgery
- Clinical Study Conjunctivodacryocystorhinostomy with Jones Tube
- Conjunctivodacryocystorhinostomy with Rubber-Tipped Jones Tube
- Management of Complications after Conjunctivodacryocystorhinostomy with Jones Tube
- Secretion and Excretion of Tears in Normal Eyes of Korean