J Cardiovasc Ultrasound.
2013 Jun;21(2):64-71.
Feasibility of Real-Time Three-Dimensional Echocardiography for the Assessment of Distorted Biventricular Systolic Function in Patients with Cor Pulmonale
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea. younhj@catholic.ac.kr
Abstract
- BACKGROUND
This study was to investigate the feasibility of real-time 3-dimensional echocardiography (RT3DE) for the analysis of biventricular ejection fractions and volume measurements in patients with cor pulmonale and the correlations of RT3DE results with 64-slice multi-detector cardiac computed tomography (64-MDCT) results.
METHODS
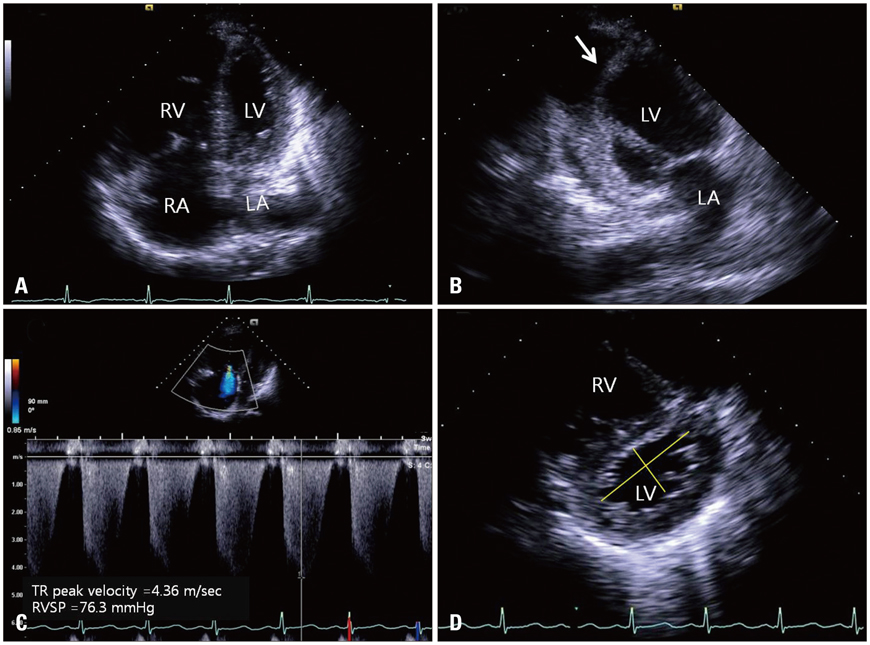
This study included a total of 22 patients (59.3 +/- 16.6 years of age; 10 males and 12 females) who showed flattening or reverse curvature of the interventricular septum and severe pulmonary hypertension [mean right ventricular (RV) systolic pressure = 66.8 +/- 19.7 mmHg] on 2-dimensional transthoracic echocardiography due to cor pulmonale. Biventricular end-diastolic and end-systolic volumes were measured by RT3DE and 64-MDCT. The severity of D-shaped deformation was evaluated by using left ventricular (LV) eccentricity index (ratio of diameters parallel/perpendicular to the interventricular septum on parasternal short axis images of the papillary muscle level).
RESULTS
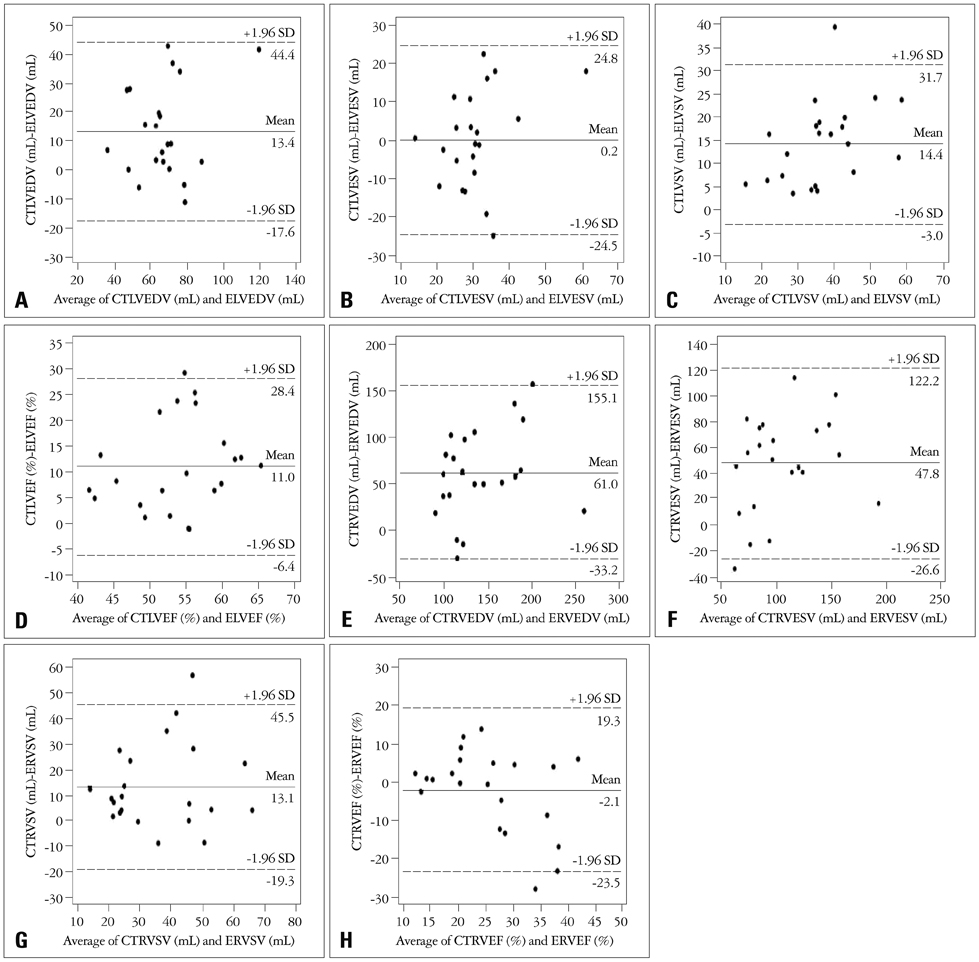
There were moderate correlations between biventricular volumes measured by RT3DE and 64-MDCT except for LV end-systolic volume (59.8 +/- 17.1 vs. 73.2 +/- 20.2 mL, r = 0.652, p = 0.001 for LV end-diastolic volume; 30.6 +/- 9.1 vs. 30.8 +/- 12.5 mL, r = 0.361, p = 0.099 for LV end-systolic volume; 110.1 +/- 42.9 vs. 171.1 +/- 55.3 mL, r = 0.545, p = 0.009 for RV end-diastolic volume; and 80.9 +/- 35.0 vs. 128.7 +/- 45.1 mL, r = 0.549, p = 0.005 for RV end-systolic volume respectively).
CONCLUSION
This study suggests that RT3DE may be a modest method for measuring distorted biventricular end-systolic and end-diastolic volumes in patients with cor pulmonale.
Keyword
MeSH Terms
Figure
Reference
-
1. Grapsa J, O'Regan DP, Pavlopoulos H, Durighel G, Dawson D, Nihoyannopoulos P. Right ventricular remodelling in pulmonary arterial hypertension with three-dimensional echocardiography: comparison with cardiac magnetic resonance imaging. Eur J Echocardiogr. 2010; 11:64–73.
Article2. Torbicki A, Skwarski K, Hawrylkiewicz I, Pasierski T, Miskiewicz Z, Zielinski J. Attempts at measuring pulmonary arterial pressure by means of Doppler echocardiography in patients with chronic lung disease. Eur Respir J. 1989; 2:856–860.3. Barberà JA, Peinado VI, Santos S. Pulmonary hypertension in chronic obstructive pulmonary disease. Eur Respir J. 2003; 21:892–905.
Article4. Laaban JP, Diebold B, Zelinski R, Lafay M, Raffoul H, Rochemaure J. Noninvasive estimation of systolic pulmonary artery pressure using Doppler echocardiography in patients with chronic obstructive pulmonary disease. Chest. 1989; 96:1258–1262.
Article5. Naeije R, Torbicki A. More on the noninvasive diagnosis of pulmonary hypertension: Doppler echocardiography revisited. Eur Respir J. 1995; 8:1445–1449.6. Chin KM, Kingman M, de Lemos JA, Warner JJ, Reimold S, Peshock R, Torres F. Changes in right ventricular structure and function assessed using cardiac magnetic resonance imaging in bosentan-treated patients with pulmonary arterial hypertension. Am J Cardiol. 2008; 101:1669–1672.
Article7. Sandstede J, Lipke C, Beer M, Hofmann S, Pabst T, Kenn W, Neubauer S, Hahn D. Age- and gender-specific differences in left and right ventricular cardiac function and mass determined by cine magnetic resonance imaging. Eur Radiol. 2000; 10:438–442.
Article8. Alfakih K, Plein S, Bloomer T, Jones T, Ridgway J, Sivananthan M. Comparison of right ventricular volume measurements between axial and short axis orientation using steady-state free precession magnetic resonance imaging. J Magn Reson Imaging. 2003; 18:25–32.
Article9. Nicol ED, Kafka H, Stirrup J, Padley SP, Rubens MB, Kilner PJ, Gatzoulis MA. A single, comprehensive non-invasive cardiovascular assessment in pulmonary arterial hypertension: combined computed tomography pulmonary and coronary angiography. Int J Cardiol. 2009; 136:278–288.
Article10. Guo YK, Gao HL, Zhang XC, Wang QL, Yang ZG, Ma ES. Accuracy and reproducibility of assessing right ventricular function with 64-section multi-detector row CT: comparison with magnetic resonance imaging. Int J Cardiol. 2010; 139:254–262.
Article11. Angelini ED, Homma S, Pearson G, Holmes JW, Laine AF. Segmentation of real-time three-dimensional ultrasound for quantification of ventricular function: a clinical study on right and left ventricles. Ultrasound Med Biol. 2005; 31:1143–1158.
Article12. Jenkins C, Leano R, Chan J, Marwick TH. Reconstructed versus real-time 3-dimensional echocardiography: comparison with magnetic resonance imaging. J Am Soc Echocardiogr. 2007; 20:862–868.
Article13. Jenkins C, Bricknell K, Hanekom L, Marwick TH. Reproducibility and accuracy of echocardiographic measurements of left ventricular parameters using real-time three-dimensional echocardiography. J Am Coll Cardiol. 2004; 44:878–886.
Article14. Jenkins C, Bricknell K, Chan J, Hanekom L, Marwick TH. Comparison of two- and three-dimensional echocardiography with sequential magnetic resonance imaging for evaluating left ventricular volume and ejection fraction over time in patients with healed myocardial infarction. Am J Cardiol. 2007; 99:300–306.
Article15. Grewal J, Majdalany D, Syed I, Pellikka P, Warnes CA. Three-dimensional echocardiographic assessment of right ventricular volume and function in adult patients with congenital heart disease: comparison with magnetic resonance imaging. J Am Soc Echocardiogr. 2010; 23:127–133.
Article16. Khoo NS, Young A, Occleshaw C, Cowan B, Zeng IS, Gentles TL. Assessments of right ventricular volume and function using three-dimensional echocardiography in older children and adults with congenital heart disease: comparison with cardiac magnetic resonance imaging. J Am Soc Echocardiogr. 2009; 22:1279–1288.
Article17. Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713. quiz 786-8.
Article18. Burgess MI, Bright-Thomas RJ, Ray SG. Echocardiographic evaluation of right ventricular function. Eur J Echocardiogr. 2002; 3:252–262.
Article19. Chuang ML, Hibberd MG, Salton CJ, Beaudin RA, Riley MF, Parker RA, Douglas PS, Manning WJ. Importance of imaging method over imaging modality in noninvasive determination of left ventricular volumes and ejection fraction: assessment by two- and three-dimensional echocardiography and magnetic resonance imaging. J Am Coll Cardiol. 2000; 35:477–484.
Article20. Jacobs LD, Salgo IS, Goonewardena S, Weinert L, Coon P, Bardo D, Gerard O, Allain P, Zamorano JL, de Isla LP, Mor-Avi V, Lang RM. Rapid online quantification of left ventricular volume from real-time three-dimensional echocardiographic data. Eur Heart J. 2006; 27:460–468.
Article21. Okuyama T, Ehara S, Shirai N, Sugioka K, Ogawa K, Oe H, Kitamura H, Itoh T, Otani K, Matsuoka T, Inoue Y, Ueda M, Hozumi T, Yoshiyama M. Usefulness of three-dimensional automated quantification of left ventricular mass, volume, and function by 64-slice computed tomography. J Cardiol. 2008; 52:276–284.
Article22. Sugeng L, Mor-Avi V, Weinert L, Niel J, Ebner C, Steringer-Mascherbauer R, Schmidt F, Galuschky C, Schummers G, Lang RM, Nesser HJ. Quantitative assessment of left ventricular size and function: side-by-side comparison of real-time three-dimensional echocardiography and computed tomography with magnetic resonance reference. Circulation. 2006; 114:654–661.
Article23. Brent BN, Berger HJ, Matthay RA, Mahler D, Pytlik L, Zaret BL. Physiologic correlates of right ventricular ejection fraction in chronic obstructive pulmonary disease: a combined radionuclide and hemodynamic study. Am J Cardiol. 1982; 50:255–262.
Article24. MacNee W, Wathen CG, Hannan WJ, Flenley DC, Muir AL. Effects of pirbuterol and sodium nitroprusside on pulmonary haemodynamics in hypoxic cor pulmonale. Br Med J (Clin Res Ed). 1983; 287:1169–1172.
Article25. MacNee W. Pathophysiology of cor pulmonale in chronic obstructive pulmonary disease. Part One. Am J Respir Crit Care Med. 1994; 150:833–852.
Article26. Takakura M, Harada T, Fukuno H, Okushi H, Taniguchi T, Sawada S, Fujinaga H, Wakatsuki T, Oki T. Echocardiographic Detection of Occult Cor Pulmonale During Exercise in Patients with Chronic Obstructive Pulmonary Disease. Echocardiography. 1999; 16:127–134.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Echocardiographic Evaluation of Right Ventricular Diastolic Function in Patients with Chronic Obstructive Pulmonary Disease
- Radiological discrimination of cor pulmonale with pulmonary function and electrocardiography finding in coal workers pneumoconiosis
- Efficacy of Inhaled Iloprost in Cor Pulmonale and Severe Pulmonary Hypertension Associated with Tuberculous Destroyed Lung
- Comparison of Noninvasive Criteria for Diagnosing Cor Pulmonale - With Particular Reference to Comparison of Electrocardiogrhphic Diagnostic Criteria and Echocardiographic Diagnostic Criteria
- Circulating Blood Volume in Various Respiratory Diseases