J Korean Assoc Oral Maxillofac Surg.
2017 Feb;43(1):29-36. 10.5125/jkaoms.2017.43.1.29.
Oral manifestations and their correlation to baseline CD4 count of HIV/AIDS patients in Ghana
- Affiliations
-
- 1Oral and Maxillofacial Microvascular Reconstruction LAB, Brong Ahafo Regional Hospital, Sunyani, Ghana. smin5@snu.ac.kr
- 2Department of Ear, Nose and Throat, Brong Ahafo Regional Hospital, Sunyani, Ghana.
- 3Department of Oral and Maxillofacial Surgery, Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea.
- KMID: 2385067
- DOI: http://doi.org/10.5125/jkaoms.2017.43.1.29
Abstract
OBJECTIVES
Acquired immunodeficiency syndrome (AIDS) is a disease of the human immune system caused by the human immunodeficiency virus (HIV). People with AIDS are much more vulnerable to infections, including opportunistic infections and tumors, than people with a healthy immune system. The objective of this study was to correlate oral lesions associated with HIV/AIDS and immunosuppression levels by measuring clusters of differentiation 4 (CD4) cell counts among patients living in the middle western regions of Ghana.
MATERIALS AND METHODS
A total of 120 patients who visited the HIV clinic at the Komfo Anokye Teaching Hospital and the Regional Hospital Sunyani of Ghana were consecutively enrolled in this prospective and cross-sectional study. Referred patients' baseline CD4 counts were obtained from medical records and each patient received an initial physician assessment. Intraoral diagnoses were based on the classification and diagnostic criteria of the EEC Clearinghouse, 1993. After the initial assessment, extra- and intraoral tissues from each enrolled patient were examined. Data analyses were carried out using simple proportions, frequencies and chi-square tests of significance.
RESULTS
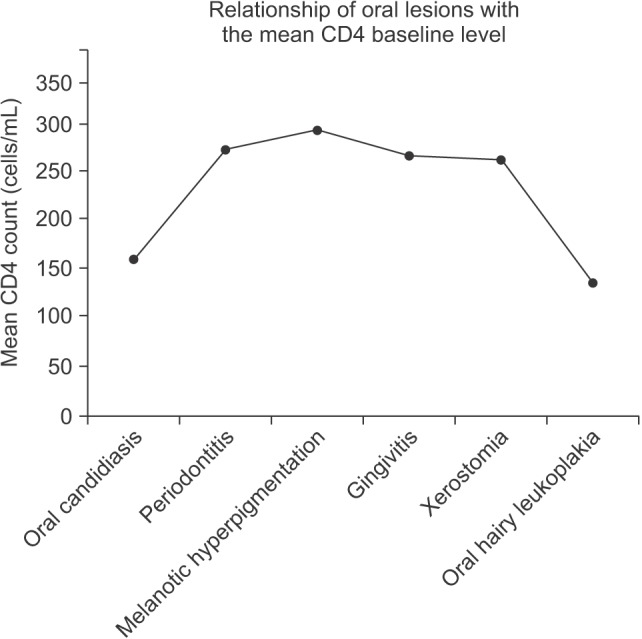
Our study included 120 patients, and was comprised of 42 (35.0%) males and 78 (65.0%) females, ranging in age from 21 to 67 years with sex-specific mean ages of 39.31 years (males) and 39.28 years (females). Patient CD4 count values ranged from 3 to 985 cells/mL with a mean baseline CD4 count of 291.29 cells/mL for males and 325.92 cells/mL for females. The mean baseline CD4 count for the entire sample was 313.80 cells/mL. Of the 120 patients we examined, 99 (82.5%) were observed to have at least one HIV-associated intraoral lesion while 21 (17.5%) had no intraoral lesions. Oral candidiasis, periodontitis, melanotic hyperpigmentation, gingivitis and xerostomia were the most common oral lesions.
CONCLUSION
From a total of nine oral lesions, six lesions that included oral candidiasis, periodontitis, melanotic hyperpigmentation, gingivitis, xerostomia and oral hairy leukoplakia were significantly correlated with declining CD4 counts.
Keyword
MeSH Terms
-
Acquired Immunodeficiency Syndrome
Candidiasis, Oral
CD4 Lymphocyte Count*
Cell Count
Classification
Cross-Sectional Studies
Diagnosis
European Union
Female
Ghana*
Gingivitis
HIV
Hospitals, Teaching
Humans
Hyperpigmentation
Immune System
Immunosuppression
Leukoplakia, Hairy
Male
Medical Records
Opportunistic Infections
Oral Manifestations*
Periodontitis
Prospective Studies
Statistics as Topic
Xerostomia
Figure
Cited by 2 articles
-
Oral lesions associated with human immunodeficiency virus in 75 adult patients: a clinical study
Antoine Berberi, Georges Aoun
J Korean Assoc Oral Maxillofac Surg. 2017;43(6):388-394. doi: 10.5125/jkaoms.2017.43.6.388.Importance of various oral manifestations regardless of CD4 cell count in HIV/AIDS patients
Soung Min Kim, Jong Ho Lee
J Korean Assoc Oral Maxillofac Surg. 2018;44(6):298-301. doi: 10.5125/jkaoms.2018.44.6.298.
Reference
-
1. Summary of the 2013 HIV Sentinel survey report [Internet]. Accra, Ghana: Ghana AIDS Commission;cited 2016 Mar 12. Available from: http://www.ghanaids.gov.gh/gac1/aids_info.php.2. Parathyras J, Gebhardt S, Hillermann-Rebello R, Grobbelaar N, Venter M, Warnich L. A pharmacogenetic study of CD4 recovery in response to HIV antiretroviral therapy in two South African population groups. J Hum Genet. 2009; 54:261–265. PMID: 19282874.
Article3. Begg MD, Lamster IB, Panageas KS, Mitchell-Lewis D, Phelan JA, Grbic JT. A prospective study of oral lesions and their predictive value for progression of HIV disease. Oral Dis. 1997; 3:176–183. PMID: 9467362.
Article4. Cheng R, Patel S, Mandel L. Oral manifestations in untreated HIV patient. N Y State Dent J. 2011; 77:58–60. PMID: 22029118.5. Saini R. Oral lesions: a true clinical indicator in human immunodeficiency virus. J Nat Sci Biol Med. 2011; 2:145–150. PMID: 22346226.
Article6. Mellors JW, Muñoz A, Giorgi JV, Margolick JB, Tassoni CJ, Gupta P, et al. Plasma viral load and CD4+ lymphocytes as prognostic markers of HIV-1 infection. Ann Intern Med. 1997; 126:946–954. PMID: 9182471.
Article7. Mellors JW, Rinaldo CR Jr, Gupta P, White RM, Todd JA, Kingsley LA. Prognosis in HIV-1 infection predicted by the quantity of virus in plasma. Science. 1996; 272:1167–1170. PMID: 8638160.
Article8. Vlahov D, Graham N, Hoover D, Flynn C, Bartlett JG, Margolick JB, et al. Prognostic indicators for AIDS and infectious disease death in HIV-infected injection drug users: plasma viral load and CD4+ cell count. JAMA. 1998; 279:35–40. PMID: 9424041.9. Chan RK. Early clinical manifestations of HIV infection. Singapore Med J. 1990; 31:477–479. PMID: 2259948.10. Beverly P, Helbert M. Immunology of aids; ABC of AIDS. 4th ed. New York: BMJ Publication Group;1997. p. 11–12.11. Berkley S, Naamara W, Okware S, Downing R, Konde-Lule J, Wawer M, et al. AIDS and HIV infection in Uganda--are more women infected than men? AIDS. 1990; 4:1237–1242. PMID: 2088401.
Article12. Guteta S, Feleke Y, Fekade D, Neway M, Diro E. Prevalence of oral and perioral manifestations in HIV positive adults at Tikur Anbessa Teaching Hospital Addis Ababa, Ethiopia. Ethiop Med J. 2008; 46:349–357. PMID: 19271399.13. Gasparin AB, Ferreira FV, Danesi CC, Mendoza-Sassi RA, Silveira J, Martinez AM, et al. Prevalence of oral lesions in persons with HIV and associated factors in a southern Brazilian city. Cad Saude Publica. 2009; 25:1307–1315. PMID: 19503961.14. 2014 progress report on the global plan [Internet]. Geneva, Switzerland: UNAIDS;2014. 11. 11. cited 2017 Feb 9. Available from: http://www.unaids.org/en/resources/documents/2014/JC2681_2014-Global-Plan-progress.15. Butt FM, Chindia ML, Vaghela VP, Mandalia K. Oral manifestations of HIV/AIDS in a Kenyan provincial hospital. East Afr Med J. 2001; 78:398–401. PMID: 11921559.16. Greenwood I, Zakrzewska JM, Robinson PG. Changes in the prevalence of HIV-associated mucosal disease at a dedicated clinic over 7 years. Oral Dis. 2002; 8:90–94. PMID: 11991309.17. EC Clearinghouse on Oral Problems Related to HIV Infection and WHO Collaborating Centre on Oral Manifestations of the Human Immunodeficiency Virus. Classification and diagnostic criteria for oral lesions in HIV infection. J Oral Pathol Med. 1991; 20:97–100. PMID: 1645406.18. Classification and diagnostic criteria for oral lesions in HIV infection. EC-Clearinghouse on Oral Problems Related to HIV Infection and WHO Collaborating Centre on Oral Manifestations of the Immunodeficiency Virus. J Oral Pathol Med. 1993; 22:289–291. PMID: 8229864.19. Ending the AIDS epidemic [Internet]. Geneva, Switzerland: UNAIDS;2014. 12. 01. cited 2017 Feb 9. Available from: http://www.unaids.org/en/resources/documents/2014/20141201_Paris_declaration.20. Ranganathan K, Reddy BV, Kumarasamy N, Solomon S, Viswanathan R, Johnson NW. Oral lesions and conditions associated with human immunodeficiency virus infection in 300 south Indian patients. Oral Dis. 2000; 6:152–157. PMID: 10822358.
Article21. Ranganathan K, Umadevi M, Saraswathi TR, Kumarasamy N, Solomon S, Johnson N. Oral lesions and conditions associated with human immunodeficiency virus infection in 1000 South Indian patients. Ann Acad Med Singapore. 2004; 33(4 Suppl):37–42. PMID: 15389305.22. Bravo IM, Correnti M, Escalona L, Perrone M, Brito A, Tovar V, et al. Prevalence of oral lesions in HIV patients related to CD4 cell count and viral load in a Venezuelan population. Med Oral Patol Oral Cir Bucal. 2006; 11:E33–E39. PMID: 16388291.23. Adurogbangba MI, Aderinokun GA, Odaibo GN, Olaleye OD, Lawoyin TO. Oro-facial lesions and CD4 counts associated with HIV/AIDS in an adult population in Oyo State, Nigeria. Oral Dis. 2004; 10:319–326. PMID: 15533205.
Article24. Jonsson N, Zimmerman M, Chidzonga MM, Jonsson K. Oral manifestations in 100 Zimbabwean HIV/AIDS patients referred to a specialist centre. Cent Afr J Med. 1998; 44:31–34. PMID: 9675968.25. Adedigba MA, Ogunbodede EO, Jeboda SO, Naidoo S. Patterns of oral manifestation of HIV/AIDS among 225 Nigerian patients. Oral Dis. 2008; 14:341–346. PMID: 18410577.
Article26. Arendorf T, Holmes H. Oral manifestations associated with human immunodeficiency virus (HIV) infection in developing countries--are there differences from developed countries? Oral Dis. 2000; 6:133–135. PMID: 10822355.
Article27. Naidoo S, Chikte U. Oro-facial manifestations in paediatric HIV: a comparative study of institutionalized and hospital outpatients. Oral Dis. 2004; 10:13–18. PMID: 14996288.
Article28. Bodhade AS, Ganvir SM, Hazarey VK. Oral manifestations of HIV infection and their correlation with CD4 count. J Oral Sci. 2011; 53:203–211. PMID: 21712625.
Article29. Greenspan JS. Sentinels and signposts: the epidemiology and significance of the oral manifestations of HIV disease. Oral Dis. 1997; 3(Suppl 1):S13–S17. PMID: 9456650.
Article30. Sabin CA, Phillips AN. Should HIV therapy be started at a CD4 cell count above 350 cells/microl in asymptomatic HIV-1-infected patients? Curr Opin Infect Dis. 2009; 22:191–197. PMID: 19283914.31. Gaurav S, Keerthilatha PM, Archna N. Prevalence of Oral Manifestations and Their Association with CD4/CD8 Ratio and HIV Viral Load in South India. Int J Dent. 2011; 2011:964278. PMID: 22046186.
Article32. Nam JH, Noh KL, Pang EO, Kim DY, Kim JH, Chung JA, et al. AIDS-associated Kaposi's sarcoma on left lower retromolar triangle and parapharyngeal area: a case report. J Korean Assoc Oral Maxillofac Surg. 2009; 35:182–186.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Importance of various oral manifestations regardless of CD4 cell count in HIV/AIDS patients
- Frequency of Skin Disorders in HIV-infected Patients and Their Relationship to CD4+ T Lymphocyte Counts
- Oral lesions associated with human immunodeficiency virus in 75 adult patients: a clinical study
- Oral Manifestations of Human Immunodeficiency Virus Infection: Early Diagnostic Indicators
- Ocular Manifestations of Acquired Immunodeficiency Syndrome in Korea