J Periodontal Implant Sci.
2016 Jun;46(3):166-175. 10.5051/jpis.2016.46.3.166.
Preferences and flexibility in decision-making among dental clinicians regarding the treatment of multirooted teeth: an interactive communication device-based survey at two academic conferences
- Affiliations
-
- 1Department of Periodontology, Institute for Periodontal Regeneration, Yonsei University College of Dentistry, Seoul, Korea. drjew@yuhs.ac
- 2Department of Periodontology, Kyung Hee University School of Dentistry, Seoul, Korea.
- KMID: 2382981
- DOI: http://doi.org/10.5051/jpis.2016.46.3.166
Abstract
- PURPOSE
Decision-making by dental and medical experts can be influenced by their biases, interests, and experiences, and academic arguments about controversial issues may additionally be considered indirect experiences capable of affecting decision-making. This study reports on the use of interactive communication devices to evaluate preferences and flexibility in decision-making among dental care providers who attended two distinct academic conferences.
METHODS
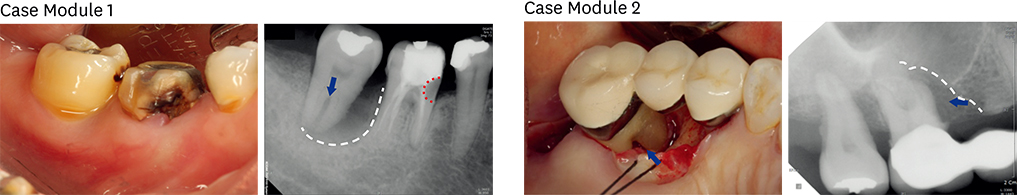
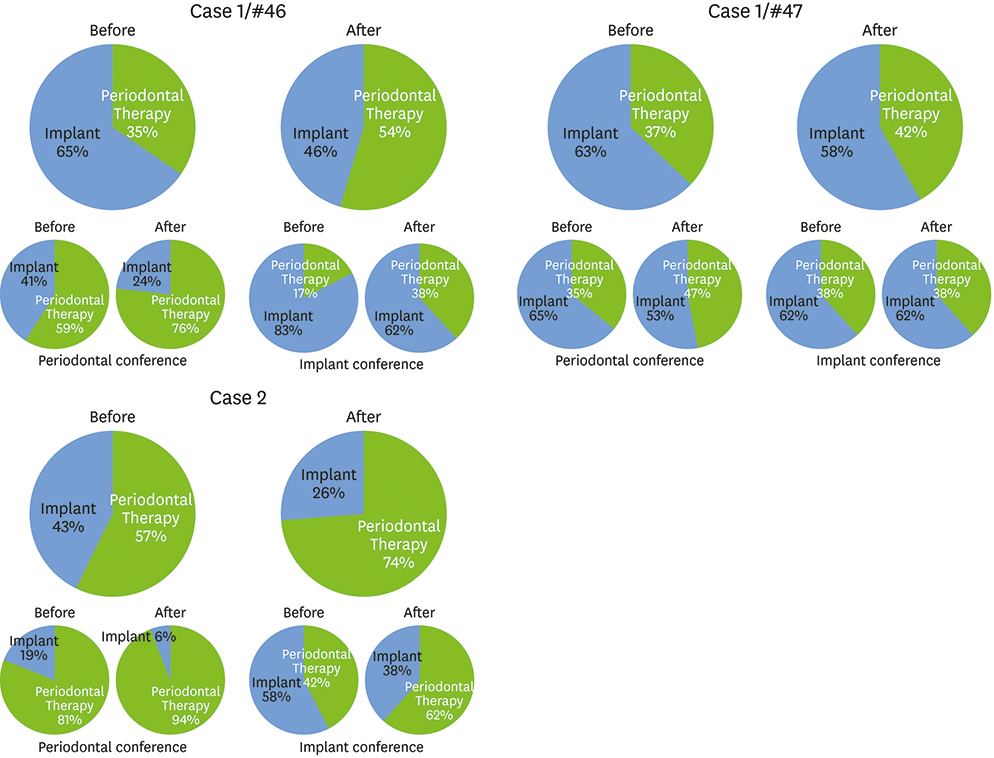
Two debates were presented by a team of two lecturers at two academic conferences (focusing on periodontology and implant dentistry, respectively) and the audience members of each session were surveyed. Before each lecture, two case modules about the diagnosis and treatment of multirooted molar lesions were provided, and interactive communication devices were used to collect responses about decision-making preferences in treatment planning immediately before and after a debate about treatment strategies.
RESULTS
In total, 81 and 84 completed answers from both conferences were obtained for the first and second case modules, respectively. The preferred treatment plan differed significantly according to the focus of the conference, and a tendency emerged for the clinicians participating in each conference to express uniform preferences. However, attending the debates resulted in significant changes in decision-making preferences regardless of the conference focus or the characteristics of the participants.
CONCLUSIONS
Our findings suggest that providing continuing education via debates on controversial issues may be effective in widening conceptual knowledge and reducing biases among experts in the dental and medical fields.
Keyword
MeSH Terms
Figure
Reference
-
1. Nunn ME, Fan J, Su X, Levine RA, Lee HJ, McGuire MK. Development of prognostic indicators using classification and regression trees for survival. Periodontol 2000. 2012; 58:134–142.
Article2. Halperin-Sternfeld M, Levin L. Do we really know how to evaluate tooth prognosis? A systematic review and suggested approach. Quintessence Int. 2013; 44:447–456.3. Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009; 80:476–491.
Article4. Wang HL, Burgett FG, Shyr Y, Ramfjord S. The influence of molar furcation involvement and mobility on future clinical periodontal attachment loss. J Periodontol. 1994; 65:25–29.
Article5. Thomas MV, Beagle JR. Evidence-based decision-making: implants versus natural teeth. [viii.]. Dent Clin North Am. 2006; 50:451–461.
Article6. Kinsel RP, Lamb RE, Ho D. The treatment dilemma of the furcated molar: root resection versus single-tooth implant restoration. A literature review. Int J Oral Maxillofac Implants. 1998; 13:322–332.7. Brägger U, Krenander P, Lang NP. Economic aspects of single-tooth replacement. Clin Oral Implants Res. 2005; 16:335–341.
Article8. Holm-Pedersen P, Lang NP, Müller F. What are the longevities of teeth and oral implants? Clin Oral Implants Res. 2007; 18:Suppl 3. 15–19.
Article9. Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res. 2007; 18:Suppl 3. 97–113.
Article10. Hutton RJ, Klein G. Expert decision making. Syst Eng. 1999; 2:32–45.
Article11. Milkman KL, Chugh D, Bazerman MH. How can decision making be improved? Perspect Psychol Sci. 2009; 4:379–383.
Article12. Pommer B, Becker K, Arnhart C, Fabian F, Rathe F, Stigler RG. How meta-analytic evidence impacts clinical decision making in oral implantology: a Delphi opinion poll. Clin Oral Implants Res. 2016; 27:282–287.
Article13. Brånemark PI, Adell R, Albrektsson T, Lekholm U, Lundkvist S, Rockler B. Osseointegrated titanium fixtures in the treatment of edentulousness. Biomaterials. 1983; 4:25–28.
Article14. Laney WR, Tolman DE, Keller EE, Desjardins RP, Van Roekel NB, Brånemark PI. Dental implants: tissue-integrated prosthesis utilizing the osseointegration concept. Mayo Clin Proc. 1986; 61:91–97.
Article15. Wang G, Gao X, Lo EC. Public perceptions of dental implants: a qualitative study. J Dent. 2015; 43:798–805.
Article16. Aminoshariae A, Teich S, Heima M, Kulild JC. The role of insurance and training in dental decision making. J Endod. 2014; 40:1082–1086.
Article17. Lang-Hua BH, McGrath CP, Lo EC, Lang NP. Factors influencing treatment decision-making for maintaining or extracting compromised teeth. Clin Oral Implants Res. 2014; 25:59–66.
Article18. Matzel LD, Light KR, Wass C, Colas-Zelin D, Denman-Brice A, Waddel AC, et al. Longitudinal attentional engagement rescues mice from age-related cognitive declines and cognitive inflexibility. Learn Mem. 2011; 18:345–356.
Article19. Moshaverinia A, Kar K, Chee WW. Treatment planning decisions: implant placement versus preserving natural teeth. J Calif Dent Assoc. 2014; 42:859–868.20. Esposito M, Ardebili Y, Worthington HV. Interventions for replacing missing teeth: different types of dental implants. Cochrane Database Syst Rev. 2014; 7:CD003815.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Shared-Decision Making on Patient Satisfaction
- Patient and clinician priorities for information on treatment outcomes for advanced ovarian cancer: a Delphi exercise
- Factors affecting patients decision-making for dental prosthetic treatment
- Key Elements for Effective Shared Decision-making in Digital Environments
- Shared decision making: relevant concepts and facilitating strategies