J Adv Prosthodont.
2017 Jun;9(3):217-223. 10.4047/jap.2017.9.3.217.
Characterization and antimicrobial efficacy of Portland cement impregnated with silver nanoparticles
- Affiliations
-
- 1Department of Dentistry, Dongsan Medical Center, School of Medicine of Keimyung University, Daegu, Republic of Korea. nkyp@dsmc.or.kr
- KMID: 2382609
- DOI: http://doi.org/10.4047/jap.2017.9.3.217
Abstract
- PURPOSE
This study investigated the effects of silver nanoparticle (SN) loading into hydraulic calcium silicate-based Portland cement on its mechanical, antibacterial behavior and biocompatibility as a novel dental bone substitute.
MATERIALS AND METHODS
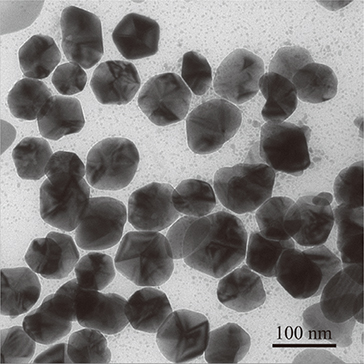
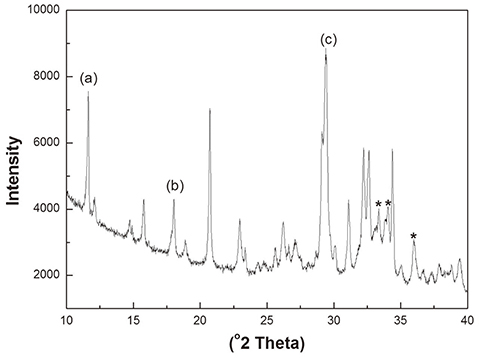
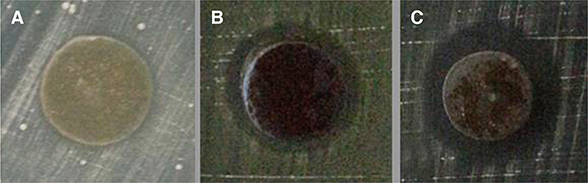
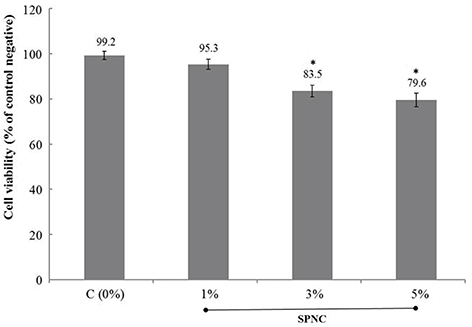
Chemically reduced colloidal SN were combined with Portland cement (PC) by the concentrations of 0 (control), 1.0, 3.0, and 5.0 wt%. The physico-mechanical properties of silver-Portland cement nanocomposites (SPNC) were investigated through X-ray diffraction (XRD), setting time, compressive strength, solubility, and silver ion elution. Antimicrobial properties of SPNC were tested by agar diffusion against Streptococcus mutans and Streptococcus sobrinus. Cytotoxic evaluation for human gingival fibroblast (HGF) was performed by MTS assay.
RESULTS
XRD certified that SN was successfully impregnated in PC. SPNC at above 3.0 wt% significantly reduced both initial and final setting times compared to control PC. No statistical differences of the compressive strength values were detected after SN loadings, and solubility rates of SPNC were below 3.0%, which are acceptable by ADA guidelines. Ag ion elutions from SPNC were confirmed with dose-dependence on the concentrations of SN added. SPNC of 5.0 wt% inhibited the growth of Streptococci, whereas no antimicrobial activity was shown in control PC. SPNC revealed no cytotoxic effects to HGF following ISO 10993 (cell viability > 70%).
CONCLUSION
Addition of SN promoted the antibacterial activity and favored the bio-mechanical properties of PC; thus, SPNC could be a candidate for the futuristic dental biomaterial. For clinical warrant, further studies including the inhibitory mechanism, in vivo and long-term researches are still required.
MeSH Terms
Figure
Reference
-
1. Berberi A, Samarani A, Nader N, Noujeim Z, Dagher M, Kanj W, Mearawi R, Salemeh Z, Badran B. Physicochemical characteristics of bone substitutes used in oral surgery in comparison to autogenous bone. Biomed Res Int. 2014; 2014:320790.2. Kim YK, Yun PY, Um IW, Lee HJ, Yi YJ, Bae JH, Lee J. Alveolar ridge preservation of an extraction socket using autogenous tooth bone graft material for implant site development: prospective case series. J Adv Prosthodont. 2014; 6:521–527.3. Wynn-Jones G, Shelton RM, Hofmann MP. Development of Portland cement for orthopedic applications, establishing injectability and decreasing setting times. J Biomed Mater Res B Appl Biomater. 2012; 100:2213–2221.4. Peh WC, Munk PL, Rashid F, Gilula LA. Percutaneous vertebral augmentation: vertebroplasty, kyphoplasty and skyphoplasty. Radiol Clin North Am. 2008; 46:611–635.5. Torabinejad M, Watson TF, Pitt Ford TR. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod. 1993; 19:591–595.6. Camilleri J, Montesin FE, Di Silvio L, Pitt Ford TR. The chemical constitution and biocompatibility of accelerated Portland cement for endodontic use. Int Endod J. 2005; 38:834–842.7. Saidon J, He J, Zhu Q, Safavi K, Spångberg LS. Cell and tissue reactions to mineral trioxide aggregate and Portland cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95:483–489.8. Abdullah D, Ford TR, Papaioannou S, Nicholson J, McDonald F. An evaluation of accelerated Portland cement as a restorative material. Biomaterials. 2002; 23:4001–4010.9. Dokami S, Raoofi S, Ashraf MJ, Khorshidi H. Histological analysis of the effect of accelerated portland cement as a bone graft substitute on experimentally-created three-walled intrabony defects in dogs. J Dent Res Dent Clin Dent Prospects. 2007; 1:131–135.10. Seong WJ, Kim HC, Jeong S, DeVeau DL, Aparicio C, Li Y, Hodges JS. Ex vivo mechanical properties of dental implant bone cement used to rescue initially unstable dental implants: a rabbit study. Int J Oral Maxillofac Implants. 2011; 26:826–836.11. Estrela C, Bammann LL, Estrela CR, Silva RS, Pécora JD. Antimicrobial and chemical study of MTA, Portland cement, calcium hydroxide paste, Sealapex and Dycal. Braz Dent J. 2000; 11:3–9.12. Miyagak DC, de Carvalho EM, Robazza CR, Chavasco JK, Levorato GL. In vitro evaluation of the antimicrobial activity of endodontic sealers. Braz Oral Res. 2006; 20:303–306.13. Samuel U, Guggenbichler JP. Prevention of catheter-related infections: the potential of a new nano-silver impregnated catheter. Int J Antimicrob Agents. 2004; 23:S75–S78.14. Nam KY. In vitro antimicrobial effect of the tissue conditioner containing silver nanoparticles. J Adv Prosthodont. 2011; 3:20–24.15. Jonaidi-Jafari N, Izadi M, Javidi P. The effects of silver nanoparticles on antimicrobial activity of ProRoot mineral trioxide aggregate (MTA) and calcium enriched mixture (CEM). J Clin Exp Dent. 2016; 8:e22–e26.16. Alt V, Bechert T, Steinrücke P, Wagener M, Seidel P, Dingeldein E, Domann E, Schnettler R. An in vitro assessment of the antibacterial properties and cytotoxicity of nanoparticulate silver bone cement. Biomaterials. 2004; 25:4383–4391.17. Kumar R, Howdle S, Münstedt H. Polyamide/silver antimicrobials: effect of filler types on the silver ion release. J Biomed Mater Res B Appl Biomater. 2005; 75:311–319.18. Feng QL, Wu J, Chen GQ, Cui FZ, Kim TN, Kim JO. A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. J Biomed Mater Res. 2000; 52:662–668.19. Durán N, Durán M, de Jesus MB, Seabra AB, Fávaro WJ, Nakazato G. Silver nanoparticles: A new view on mechanistic aspects on antimicrobial activity. Nanomedicine. 2016; 12:789–799.20. Jafari H, Afshar S. Improved photodegradation of organic contaminants using Nano-TiO2 and TiO2-SiO2 deposited on portland cement concrete blocks. Photochem Photobiol. 2016; 92:87–101.21. Guerreiro-Tanomaru JM, Trindade-Junior A, Costa BC, da Silva GF, Drullis Cifali L, Basso Bernardi MI, Tanomaru-Filho M. Effect of zirconium oxide and zinc oxide nanoparticles on physicochemical properties and antibiofilm activity of a calcium silicate-based material. ScientificWorldJournal. 2014; 2014:975213.22. International Organization for Standardization. ISO 9917-1, Dentistry-water-based cements part 1: powder/liquid acid-base cements. Geneva, Switzerland: International Standard Organization;2003.23. Samiei M, Shahi S, Aslaminabadi N, Valizadeh H, Aghazadeh Z, Pakdel SM. A new simulated plasma for assessing the solubility of mineral trioxide aggregate. Iran Endod J. 2015; 10:30–34.24. International Organization for Standardization. ISO 10993-5. In: Biological evaluation of medical devices-Part 5: Tests for in vitro cytotoxicity. Geneva, Switzerland: International Standard Organization;2009.25. Kim YK, Lee JY, Kim SG, Lim SC. Guided bone regeneration using demineralized allogenic bone matrix with calcium sulfate: case series. J Adv Prosthodont. 2013; 5:167–171.26. Ber BS, Hatton JF, Stewart GP. Chemical modification of proroot mta to improve handling characteristics and decrease setting time. J Endod. 2007; 33:1231–1234.27. Alves HL, Dos Santos LA, Bergmann CP. Injectability evaluation of tricalcium phosphate bone cement. J Mater Sci Mater Med. 2008; 19:2241–2246.28. Wang X, Chen L, Xiang H, Ye J. Influence of anti-washout agents on the rheological properties and injectability of a calcium phosphate cement. J Biomed Mater Res B Appl Biomater. 2007; 81:410–418.29. Machado DF, Bertassoni LE, Souza EM, Almeida JB, Rached RN. Effect of additives on the compressive strength and setting time of a Portland cement. Braz Oral Res. 2010; 24:158–164.30. Wang C, Li KZ, Li HJ, Jiao GS, Lua J, Houa DS. Effect of carbon fiber dispersion on the mechanical properties of carbon fiber-reinforced cement-based composites. Mater Sci Eng. 2008; 487:52–57.31. Ye Q. The study and development of the nano-composite cement structure materials. New Build Mater. 2001; 1:4–6.32. Bortoluzzi EA, Broon NJ, Bramante CM, Felippe WT, Tanomaru Filho M, Esberard RM. The influence of calcium chloride on the setting time, solubility, disintegration, and pH of mineral trioxide aggregate and white Portland cement with a radiopacifier. J Endod. 2009; 35:550–554.33. Tobias RS. Antibacterial properties of dental restorative materials: a review. Int Endod J. 1988; 21:155–160.34. Hotta M, Nakajima H, Yamamoto K, Aono M. Antibacterial temporary filling materials: the effect of adding various ratios of Ag-Zn-Zeolite. J Oral Rehabil. 1998; 25:485–489.35. Yoshida K, Tanagawa M, Atsuta M. Characterization and inhibitory effect of antibacterial dental resin composites incorporating silver-supported materials. J Biomed Mater Res. 1999; 47:516–522.36. Imazato S, Ebi N, Takahashi Y, Kaneko T, Ebisu S, Russell RR. Antibacterial activity of bactericide-immobilized filler for resin-based restoratives. Biomaterials. 2003; 24:3605–3609.37. Monteiro DR, Gorup LF, Takamiya AS, de Camargo ER, Filho AC, Barbosa DB. Silver distribution and release from an antimicrobial denture base resin containing silver colloidal nanoparticles. J Prosthodont. 2012; 21:7–15.38. Ribeiro CS, Scelza MF, Hirata Júnior R, Buarque de. The antimicrobial activity of gray-colored mineral trioxide aggregate (GMTA) and white-colored MTA (WMTA) under aerobic and anaerobic conditions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e109–e112.39. Estrela C, Bammann LL, Estrela CR, Silva RS, Pécora JD. Antimicrobial and chemical study of MTA, Portland cement, calcium hydroxide paste, Sealapex and Dycal. Braz Dent J. 2000; 11:3–9.40. Bahador A, Pourakbari B, Bolhari B, Hashemi FB. In vitro evaluation of the antimicrobial activity of nanosilver-mineral trioxide aggregate against frequent anaerobic oral pathogens by a membrane-enclosed immersion test. Biomed J. 2015; 38:77–83.41. Zand V, Lotfi M, Aghbali A, Mesgariabbasi M, Janani M, Mokhtari H, Tehranchi P, Pakdel SM. Tissue reaction and biocompatibility of implanted mineral trioxide aggregate with silver nanoparticles in a rat model. Iran Endod J. 2016; 11:13–16.42. Gomes-Filho JE, Silva FO, Watanabe S, Cintra LT, Tendoro KV, Dalto LG, Pacanaro SV, Lodi CS, de Melo FF. Tissue reaction to silver nanoparticles dispersion as an alternative irrigating solution. J Endod. 2010; 36:1698–1702.43. Chaloupka K, Malam Y, Seifalian AM. Nanosilver as a new generation of nanoproduct in biomedical applications. Trends Biotechnol. 2010; 28:580–588.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Silver Nanoparticles as a Smart Antimicrobial Agent
- In vitro antimicrobial effect of the tissue conditioner containing silver nanoparticles
- Characterization of tissue conditioner containing chitosan-doped silver nanoparticles
- In Vitro Study Evaluating the Antimicrobial Activity of Vancomycin-Impregnated Cement Stored at Room Temperature in Methicillin-Resistant Staphylococcus aureus
- Mineral trioxied aggregate and its substitutes