J Adv Prosthodont.
2011 Mar;3(1):20-24. 10.4047/jap.2011.3.1.20.
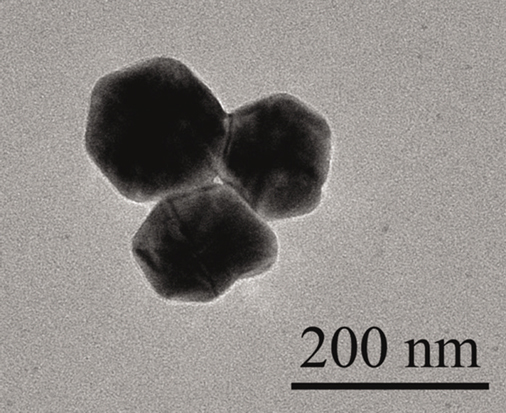
In vitro antimicrobial effect of the tissue conditioner containing silver nanoparticles
- Affiliations
-
- 1Department of Dentistry, School of Medicine, Keimyung University, Daegu, Korea. nky67@korea.com
- KMID: 1975110
- DOI: http://doi.org/10.4047/jap.2011.3.1.20
Abstract
- PURPOSE
The aim of this study was to identify in vitro antimicrobial activity of the tissue conditioner containing silver nanoparticles on microbial strains, Staphylococcus aureus, Streptococcus mutans and Candida albicans.
MATERIALS AND METHODS
Experimental disc samples (20.0x3.0 mm) of tissue conditioner (GC Soft-Liner, GC cooperation, Tokyo, Japan) containing 0.1 - 3.0% silver nanoparticles (0%: control) were fabricated. Samples were placed on separate culture plate dish and microbial suspensions (100 microL) of tested strains were inoculated then incubated at 37degrees C. Microbial growth was verified at 24 hrs and 72 hrs and the antimicrobial effects of samples were evaluated as a percentage of viable cells in withdrawn suspension (100 microL). Data were recorded as the mean of three colony forming unit (CFU) numerations and the borderline of the antimicrobial effect was determined at 0.1% viable cells.
RESULTS
A 0.1% silver nanoparticles combined to tissue conditioner displayed minimal bactericidal effect against Staphylococcus aureus and Streptococcus mutans strains, a 0.5% for fungal strain. Control group did not show any microbial inhibitory effect and there were no statistical difference between 24 hrs and extended 72 hrs incubation time (P > .05).
CONCLUSION
Within the limitation of this in vitro study, the results suggest that the tissue conditioner containing silver nanoparticles could be an antimicrobial dental material in denture plaque control. Further mechanical stability and toxicity studies are still required.
MeSH Terms
Figure
Reference
-
1. Okita N, Orstavik D, Orstavik J, Ostby K. In vivo and in vitro studies on soft denture materials: microbial adhesion and tests for antibacterial activity. Dent Mater. 1991. 7:155–160.2. Radford DR, Challacombe SJ, Walter JD. Denture plaque and adherence of Candida albicans to denture-base materials in vivo and in vitro. Crit Rev Oral Biol Med. 1999. 10:99–116.3. Nair RG, Samaranayake LP. The effect of oral commensal bacteria on candidal adhesion to denture acrylic surfaces. An in vitro study. APMIS. 1996. 104:339–349.4. Wilkieson C, Samaranayake LP, MacFarlane TW, Lamey PJ, MacKenzie D. Oral candidosis in the elderly in long term hospital care. J Oral Pathol Med. 1991. 20:13–16.5. Rossi T, Laine J, Eerola E, Kotilainen P, Peltonen R. Denture carriage of methicillin-resistant Staphylococcus aureus. Lancet. 1995. 345:1577.6. Harrison A, Basker RM, Smith IS. The compatibility of temporary soft materials with immersion denture cleansers. Int J Prosthodont. 1989. 2:254–258.7. Nikawa H, Iwanaga H, Hamada T, Yuhta S. Effects of denture cleansers on direct soft denture lining materials. J Prosthet Dent. 1994. 72:657–662.8. De Visschere LM, Grooten L, Theuniers G, Vanobbergen JN. Oral hygiene of elderly people in long-term care institutions-a cross-sectional study. Gerodontology. 2006. 23:195–204.9. Casemiro LA, Gomes Martins CH, Pires-de-Souza Fde C, Panzeri H. Antimicrobial and mechanical properties of acrylic resins with incorporated silver-zinc zeolite - part I. Gerodontology. 2008. 25:187–194.10. Quinn DM. The effectiveness, in vitro, of miconazole and ketoconazole combined with tissue conditioners in inhibiting the growth of Candida albicans. J Oral Rehabil. 1985. 12:177–182.11. Truhlar MR, Shay K, Sohnle P. Use of a new assay technique for quantification of antifungal activity of nystatin incorporated in denture liners. J Prosthet Dent. 1994. 71:517–524.12. Chow CK, Matear DW, Lawrence HP. Efficacy of antifungal agents in tissue conditioners in treating candidiasis. Gerodontology. 1999. 16:110–118.13. Koopmans AS, Kippuw N, de Graaff J. Bacterial involvement in denture-induced stomatitis. J Dent Res. 1988. 67:1246–1250.14. Budtz-Jörgensen E, Theilade E, Theilade J, Zander HA. Method for studying the development, structure and microflora of denture plaque. Scand J Dent Res. 1981. 89:149–156.15. Fu J, Ji J, Fan D, Shen J. Construction of antibacterial multilayer films containing nanosilver via layer-by-layer assembly of heparin and chitosan-silver ions complex. J Biomed Mater Res A. 2006. 79:665–674.16. Slawson RM, Lee H, Trevors JT. Bacterial interactions with silver. Biol Met. 1990. 3:151–154.17. Zhao G, Stevens SE Jr. Multiple parameters for the comprehensive evaluation of the susceptibility of Escherichia coli to the silver ion. Biometals. 1998. 11:27–32.18. Alt V, Bechert T, Steinrücke P, Wagener M, Seidel P, Dingeldein E, Domann E, Schnettler R. An in vitro assessment of the antibacterial properties and cytotoxicity of nanoparticulate silver bone cement. Biomaterials. 2004. 25:4383–4391.19. Samuel U, Guggenbichler JP. Prevention of catheter-related infections: the potential of a new nano-silver impregnated catheter. Int J Antimicrob Agents. 2004. 23:S75–S78.20. Wright JB, Lam K, Hansen D, Burrell RE. Efficacy of topical silver against fungal burn wound pathogens. Am J Infect Control. 1999. 27:344–350.21. Chandra J, Mukherjee PK, Leidich SD, Faddoul FF, Hoyer LL, Douglas LJ, Ghannoum MA. Antifungal resistance of candidal biofilms formed on denture acrylic in vitro. J Dent Res. 2001. 80:903–908.22. Bruns W, Keppeler H, Baucks R. Suppression of intrinsic resistance to penicillins in Staphylococcus aureus by polidocanol, a dodecyl polyethyleneoxid ether. Antimicrob Agents Chemother. 1985. 27:632–639.23. Gristina AG, Jennings RA, Naylor PT, Myrvik QN, Webb LX. Comparative in vitro antibiotic resistance of surface-colonizing coagulase-negative staphylococci. Antimicrob Agents Chemother. 1989. 33:813–816.24. Reverdy ME, Martra A, Fleurette J. Application of a micromethod to the study of the bactericidal activity of 2 antiseptics based on chlorhexidine gluconate. Pathol Biol (Paris). 1986. 34:688–693.25. Steinberg D, Eyal S. Early formation of Streptococcus sobrinus biofilm on various dental restorative materials. J Dent. 2002. 30:47–51.26. Satou J, Fukunaga A, Morikawa A, Matsumae I, Satou N, Shintani H. Streptococcal adherence to uncoated and saliva-coated restoratives. J Oral Rehabil. 1991. 18:421–429.27. Hahnel S, Rosentritt M, Bürgers R, Handel G. Adhesion of Streptococcus mutans NCTC 10449 to artificial teeth: an in vitro study. J Prosthet Dent. 2008. 100:309–315.28. Abe Y, Ishii M, Takeuchi M, Ueshige M, Tanaka S, Akagawa Y. Effect of saliva on an antimicrobial tissue conditioner containing silver-zeolite. J Oral Rehabil. 2004. 31:568–573.29. Baehni PC, Takeuchi Y. Anti-plaque agents in the prevention of biofilm-associated oral diseases. Oral Dis. 2003. 9:23–29.30. Christensen M, Rungby J, Mogensen SC. Effects of selenium on toxicity and ultrastructural localization of mercury in cultured murine macrophages. Toxicol Lett. 1989. 47:259–270.31. Matsuura T, Abe Y, Sato Y, Okamoto K, Ueshige M, Akagawa Y. Prolonged antimicrobial effect of tissue conditioners containing silver-zeolite. J Dent. 1997. 25:373–377.32. Mäkilä E, Hopsu-Havu VK. Mycotic growth and soft denture lining materials. Acta Odontol Scand. 1977. 35:197–205.33. Feng QL, Wu J, Chen GQ, Cui FZ, Kim TN, Kim JO. A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. J Biomed Mater Res. 2000. 52:662–668.34. Geerts GA, Stuhlinger ME, Basson NJ. Effect of an antifungal denture liner on the saliva yeast count in patients with denture stomatitis: a pilot study. J Oral Rehabil. 2008. 35:664–669.35. Petering HG. Pharmacology and toxicology of heavy metals: Silver. Pharmacol Ther. 1976. 1:127–130.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characterization of tissue conditioner containing chitosan-doped silver nanoparticles
- Silver Nanoparticles as a Smart Antimicrobial Agent
- Application of Silver Nanoparticles for the Control of Colletotrichum Species In Vitro and Pepper Anthracnose Disease in Field
- Inhibition Effects of Silver Nanoparticles against Powdery Mildews on Cucumber and Pumpkin
- Evaluation of the efficiency of chitosan and silver nanoparticles in the treatment of lice experimental infestation in local chickens