Korean J Orthod.
2017 Jul;47(4):229-237. 10.4041/kjod.2017.47.4.229.
Comparison of mechanical and biological properties of zirconia and titanium alloy orthodontic micro-implants
- Affiliations
-
- 1Department of Orthodontics, The Institute of Oral Health Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Oral Anatomy, Dental Research Institute and School of Dentistry, Seoul National University, Seoul, Korea.
- 3Department of Dental Biomaterials Science, Dental Research Institute and School of Dentistry, Seoul National University, Seoul, Korea. rhee1213@snu.ac.kr
- 4Department of Orthodontics, Dental Research Institute and School of Dentistry, Seoul National University, Seoul, Korea.
- 5Private Practice, Seoul, Korea.
- 6Section of Orthodontics, School of Dentistry, Center for Health Science, University of California, Los Angeles, USA. wmoon@dentistry.ucla.edu
- KMID: 2379555
- DOI: http://doi.org/10.4041/kjod.2017.47.4.229
Abstract
OBJECTIVE
The aim of this study was to compare the initial stability as insertion and removal torque and the clinical applicability of novel orthodontic zirconia micro-implants made using a powder injection molding (PIM) technique with those parameters in conventional titanium micro-implants.
METHODS
Sixty zirconia and 60 titanium micro-implants of similar design (diameter, 1.6 mm; length, 8.0 mm) were inserted perpendicularly in solid polyurethane foam with varying densities of 20 pounds per cubic foot (pcf), 30 pcf, and 40 pcf. Primary stability was measured as maximum insertion torque (MIT) and maximum removal torque (MRT). To investigate clinical applicability, compressive and tensile forces were recorded at 0.01, 0.02, and 0.03 mm displacement of the implants at angles of 0°, 10°, 20°, 30°, and 40°. The biocompatibility of zirconia micro-implants was assessed via an experimental animal study.
RESULTS
There were no statistically significant differences between zirconia micro-implants and titanium alloy implants with regard to MIT, MRT, or the amount of movement in the angulated lateral displacement test. As angulation increased, the mean compressive and tensile forces required to displace both types of micro-implants increased substantially at all distances. The average bone-to-implant contact ratio of prototype zirconia micro-implants was 56.88 ± 6.72%.
CONCLUSIONS
Zirconia micro-implants showed initial stability and clinical applicability for diverse orthodontic treatments comparable to that of titanium micro-implants under compressive and tensile forces.
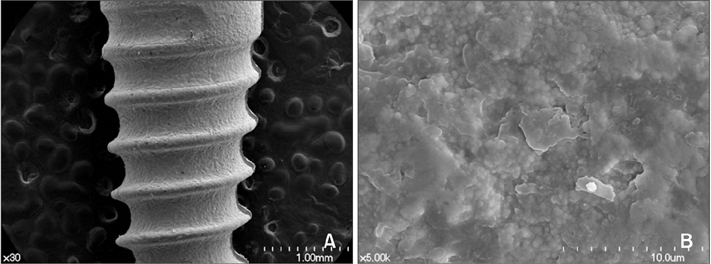
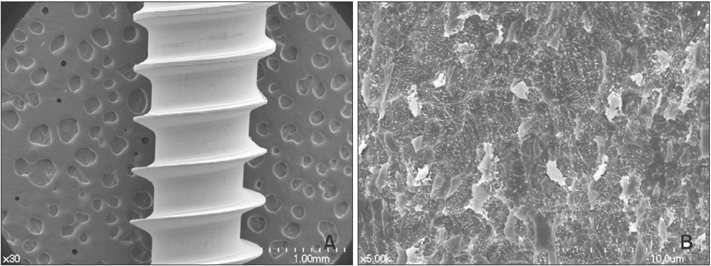
Figure
Cited by 1 articles
-
Histomorphometric evaluation of the bone surrounding orthodontic miniscrews according to their adjacent root proximity
Hyun-Ju Oh, Jung-Yul Cha, Hyung-Seog Yu, Chung-Ju Hwang
Korean J Orthod. 2018;48(5):283-291. doi: 10.4041/kjod.2018.48.5.283.
Reference
-
1. Kanomi R. Mini-implant for orthodontic anchorage. J Clin Orthod. 1997; 31:763–767.2. Reynders R, Ronchi L, Bipat S. Mini-implants in orthodontics: a systematic review of the literature. Am J Orthod Dentofacial Orthop. 2009; 135:564.e1–564.e19. discussion 564-5.
Article3. Lee SJ, Ahn SJ, Lee JW, Kim SH, Kim TW. Survival analysis of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010; 137:194–199.
Article4. Vande Vannet B, Sabzevar MM, Wehrbein H, Asscherickx K. Osseointegration of miniscrews: a histomorphometric evaluation. Eur J Orthod. 2007; 29:437–442.
Article5. Hisbergues M, Vendeville S, Vendeville P. Zirconia: Established facts and perspectives for a biomaterial in dental implantology. J Biomed Mater Res B Appl Biomater. 2009; 88:519–529.
Article6. Nascimento Cd, Pita MS, Fernandes FH, Pedrazzi V, de Albuquerque Junior RF, Ribeiro RF. Bacterial adhesion on the titanium and zirconia abutment surfaces. Clin Oral Implants Res. 2014; 25:337–343.
Article7. Gahlert M, Röhling S, Wieland M, Sprecher CM, Kniha H, Milz S. Osseointegration of zirconia and titanium dental implants: a histological and histomorphometrical study in the maxilla of pigs. Clin Oral Implants Res. 2009; 20:1247–1253.
Article8. Park YS, Chung SH, Shon WJ. Peri-implant bone formation and surface characteristics of rough surface zirconia implants manufactured by powder injection molding technique in rabbit tibiae. Clin Oral Implants Res. 2013; 24:586–591.
Article9. Song HN, Hong C, Banh R, Ohebsion T, Asatrian G, Leung HY, et al. Mechanical stability and clinical applicability assessment of novel orthodontic mini-implant design. Angle Orthod. 2013; 83:832–841.
Article10. Tsaousidis G, Bauss O. Influence of insertion site on the failure rates of orthodontic miniscrews. J Orofac Orthop. 2008; 69:349–356.
Article11. Mouhyi J, Dohan Ehrenfest DM, Albrektsson T. The peri-implantitis: implant surfaces, microstructure, and physicochemical aspects. Clin Implant Dent Relat Res. 2012; 14:170–183.
Article12. Yokoyama K, Ichikawa T, Murakami H, Miyamoto Y, Asaoka K. Fracture mechanisms of retrieved titanium screw thread in dental implant. Biomaterials. 2002; 23:2459–2465.
Article13. Sicilia A, Cuesta S, Coma G, Arregui I, Guisasola C, Ruiz E, et al. Titanium allergy in dental implant patients: a clinical study on 1500 consecutive patients. Clin Oral Implants Res. 2008; 19:823–835.
Article14. Özkurt Z, Kazazoğlu E. Zirconia dental implants: a literature review. J Oral Implantol. 2011; 37:367–376.
Article15. Butz F, Heydecke G, Okutan M, Strub JR. Survival rate, fracture strength and failure mode of ceramic implant abutments after chewing simulation. J Oral Rehabil. 2005; 32:838–843.
Article16. Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A. Bacterial adhesion on commercially pure titanium and zirconium oxide disks: an in vivo human study. J Periodontol. 2004; 75:292–296.
Article17. Teughels W, Van Assche N, Sliepen I, Quirynen M. Effect of material characteristics and/or surface topography on biofilm development. Clin Oral Implants Res. 2006; 17:Suppl 2. 68–81.
Article18. Ikeda H, Rossouw PE, Campbell PM, Kontogiorgos E, Buschang PH. Three-dimensional analysis of peri-bone-implant contact of rough-surface miniscrew implants. Am J Orthod Dentofacial Orthop. 2011; 139:e153–e163.
Article19. Aboushelib MN, Salem NA, Taleb AL, El Moniem NM. Influence of surface nano-roughness on osseointegration of zirconia implants in rabbit femur heads using selective infiltration etching technique. J Oral Implantol. 2013; 39:583–590.
Article20. Zinelis S, Thomas A, Syres K, Silikas N, Eliades G. Surface characterization of zirconia dental implants. Dent Mater. 2010; 26:295–305.
Article21. Wilmes B, Rademacher C, Olthoff G, Drescher D. Parameters affecting primary stability of orthodontic mini-implants. J Orofac Orthop. 2006; 67:162–174.
Article22. Kim YK, Kim YJ, Yun PY, Kim JW. Effects of the taper shape, dual-thread, and length on the mechanical properties of mini-implants. Angle Orthod. 2009; 79:908–914.
Article23. Hong C, Lee H, Webster R, Kwak J, Wu BM, Moon W. Stability comparison between commercially available mini-implants and a novel design: part 1. Angle Orthod. 2011; 81:692–699.
Article24. Meursinge Reynders RA, Ronchi L, Ladu L, van Etten-Jamaludin F, Bipat S. Insertion torque and success of orthodontic mini-implants: a systematic review. Am J Orthod Dentofacial Orthop. 2012; 142:596–614.e5.
Article25. Motoyoshi M, Hirabayashi M, Uemura M, Shimizu N. Recommended placement torque when tightening an orthodontic mini-implant. Clin Oral Implants Res. 2006; 17:109–114.
Article26. Lee NK, Baek SH. Effects of the diameter and shape of orthodontic mini-implants on microdamage to the cortical bone. Am J Orthod Dentofacial Orthop. 2010; 138:8.e1–8.e8. discussion 8-9.
Article27. Kim JW, Ahn SJ, Chang YI. Histomorphometric and mechanical analyses of the drill-free screw as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2005; 128:190–194.
Article28. Holst AI, Karl M, Karolczak M, Goellner M, Holst S. Quantitative assessment of orthodontic mini-implant displacement: the effect of initial force application. Quintessence Int. 2010; 41:59–66.29. Pickard MB, Dechow P, Rossouw PE, Buschang PH. Effects of miniscrew orientation on implant stability and resistance to failure. Am J Orthod Dentofacial Orthop. 2010; 137:91–99.
Article30. Kim TW, Baek SH, Kim JW, Chang YI. Effects of microgrooves on the success rate and soft tissue adaptation of orthodontic miniscrews. Angle Orthod. 2008; 78:1057–1064.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mechanical properties of nickel titanium and steel alloys under stress- strain test
- Comparison of Titanium Micro Mesh(R) with Titanium Mesh Screen 1.3(R) in the Reconstruction of Medial Orbital wall Fracture
- Comparison of marginal and internal fit of zirconia abutments with titanium abutments in internal hexagonal implants
- Comparison of biofilm on titanium and zirconia surfaces: in vivo study
- Evaluation of Osseointegration around Tibial Implants in Rats by Ibandronate-Treated Nanotubular Ti-32Nb-5Zr Alloy