J Korean Ophthalmol Soc.
2017 Apr;58(4):455-458. 10.3341/jkos.2017.58.4.455.
A Case of Fungal Ball Causing Acute Dacryocystitis
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. yswoph@hanmail.net
- KMID: 2376602
- DOI: http://doi.org/10.3341/jkos.2017.58.4.455
Abstract
- PURPOSE
We report a case of fungal ball after Endoscopic Dacryocystorhinostomy (DCR) in a 40-year-old female patient.
CASE SUMMARY
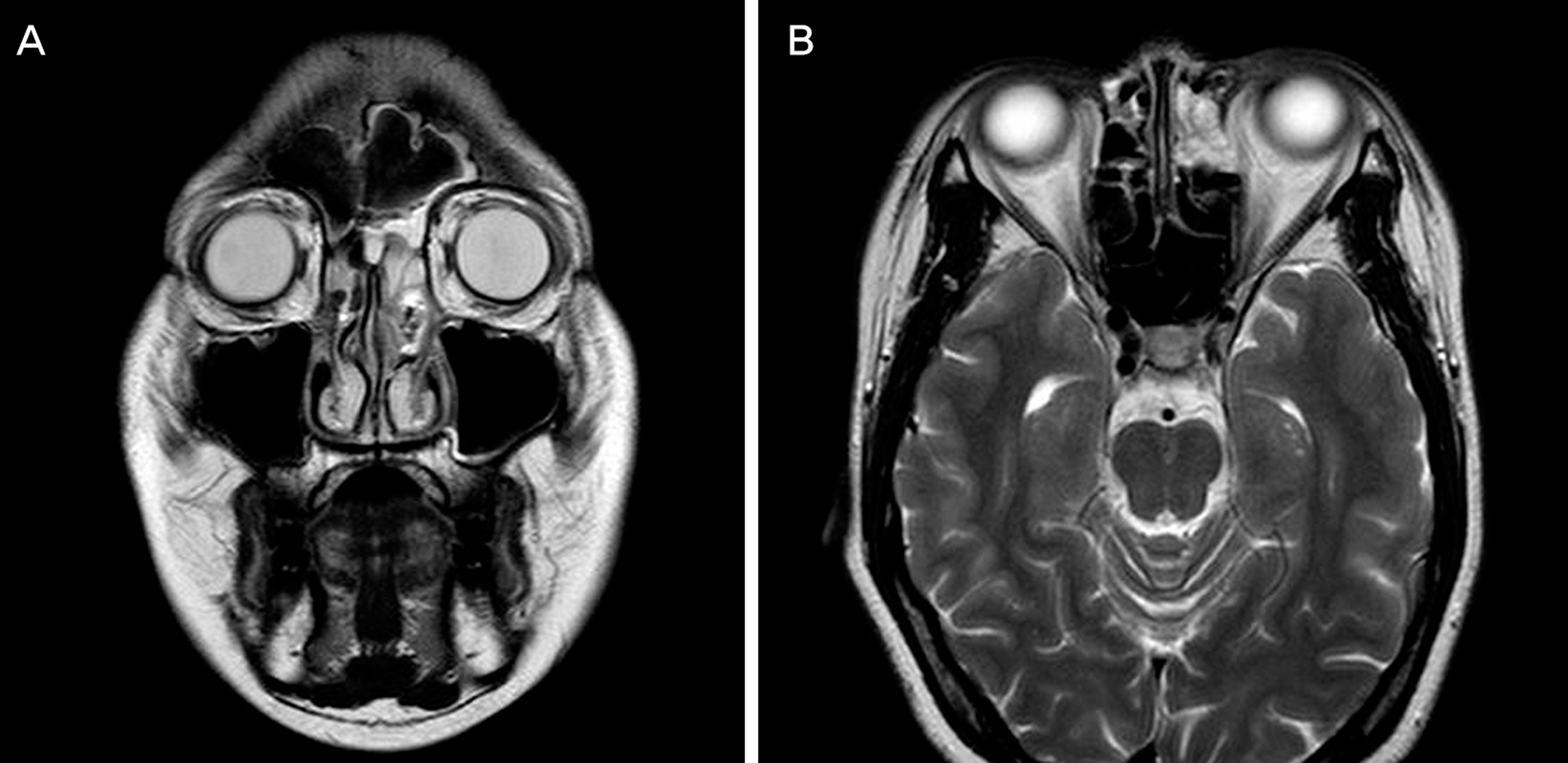
A 40-year-old female patient was admitted to our hospital for left lower eyelid tenderness and bloody discharge from the lacrimal punctum. During a planned endoscopic DCR, the sac was opened after the osteotomy, and 2 fungal balls were found in the lacrimal sac. The masses were 7 × 5 mm and, 9 × 5 mm sized, irregularly shaped, and red in color. Aspergillus fumigatus was diagnosed pathologically. Postoperative paranasal sinus magnetic resonance imaging showed no residual fungal ball. During follow-up, the patient showed patent rhinostomy opening, and there was no evidence of fungal infection on nasal endoscopic finding.
CONCLUSIONS
Although Aspergillus fumigatus is a rare cause of canalicular obstruction, fungal ball development in the lacrimal sac can cause acute dacryocystitis.
MeSH Terms
Figure
Reference
-
References
1. Ali MJ, Joshi SD, Naik MN, Honavar SG. . Clinical profile and management outcome of acute dacryocystitis: two decades of experience in a tertiary eye care center. Semin Ophthalmol. 2015; 30:118–23.
Article2. Gregg KS, Kauffman CA. . Invasive Aspergillosis: epidemiology, clinical aspects, and treatment. Semin Respir Crit Care Med. 2015; 36:662–72.
Article3. Brightbill FS, Fraser LK. . Unilateral keratoconjunctivitis with ca-nalicular obstruction by Aspergillus fumigatus. Arch Ophthalmol. 1974; 91:421–2.4. Bartley GB. . Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 1. Ophthal Plast Reconstr Surg. 1992; 8:237–42.5. Obi E, Roy A, Bates V, Sandy C. . Bilateral chronic fungal dacryo-cystitis caused by Candida dubliniensis in a neutropenic patient. J Clin Pathol. 2006; 59:1194–5.
Article6. Davies BW, Gonzalez MO, Vaughn RC. . Dacryocystitis as the initial presentation of invasive fungal sinusitis in immunocompro-mised children. Ophthal Plast Reconstr Surg. 2016; 32:e79–81.
Article7. Kubo M, Sakuraba T, Wada R. . Clinicopathological features of da-cryolithiasis in Japanese patients: frequent association with in-fection in aged patients. ISRN Ophthalmol. 2013; 2013:406153.
Article8. Lim JW, Suh JW, Lee SJ. . A case of fungall ball after external dacryocystorhinostomy. J Korean Ophthalmol Soc. 2006; 47:1481–5.9. Han MS, Kim YH, Lee JH. . The fungal infection of nasal cavity af-ter endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2003; 44:1433–6.10. Cho HS, Lee KE, Kim KS. . Two cases of fungus ball in bilateral paranasal sinuses. Korean J Otorhinolaryngology-Head Neck Surg. 2014; 57:185–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Actinomycosis of the Maxillary Sinus Accompanied with Fungal Ball
- A Case of Fungal Ball with Cholesterol Granuloma in the Middle Ear Cavity
- Bacterial Urosepsis by a Fungal Ball Mimicking a Ureteral Stone
- A Case of Fungall Ball after External Dacryocystorhinostomy
- A Case of Fungal Ball Caused by Retained Glass Foreign Body in Maxillary Sinus for 30 Years