Perinatology.
2017 Mar;28(1):20-24. 10.14734/PN.2017.28.1.20.
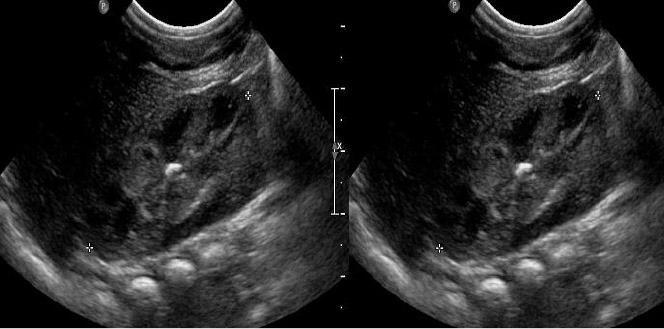
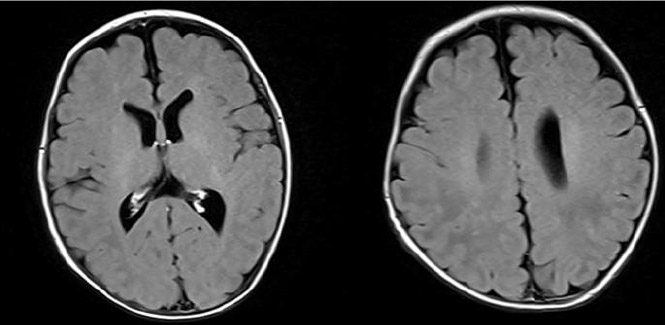
A Case of Incidentally Discovered Multiple Disseminated Fungal Brain Abscess in Asymptomatic Very Low Birth Weight Infant
- Affiliations
-
- 1Department of Pediatrics, Dongguk University Ilsan Hospital, Goyang, Korea. dayeong1@hanmail.net
- KMID: 2376573
- DOI: http://doi.org/10.14734/PN.2017.28.1.20
Abstract
- Neonatal brain abscess is a very rare disease. Despite improvement of survival rate of premature infants due to the development of neonatal intensive therapy, it is still one of the important causes of death or sequelae of neonate. Fungal infection is unusual cause of neonatal brain abscess and the neonatal fungal brain abscess is a secondary result of hematogenous seeding that is rarely discovered primarily. We present a case of incidentally discovered multiple disseminated fungal brain abscess in asymptomatic very low birth weight infant.
Keyword
MeSH Terms
Figure
Reference
-
1. Manzoni P, Farina D, Leonessa M, d'Oulx EA, Galletto P, Mostert M, et al. Risk factors for progression to invasive fungal infection in preterm neonates with fungal colonization. Pediatrics. 2006; 118:2359–2364.
Article2. Kim S, Park H, Park S, Hong Y, Lee Y, Shin J. The etiology of neonatal bacterial meningitis in Busan, Korea. Korean J Pediatr Infect Dis. 2007; 14:43–46.
Article3. Rodriguez D, Almirante B, Park BJ, Cuenca-Estrella M, Planes AM, Sanchez F, et al. Candidemia in neonatal intensive care units: Barcelona, Spain. Pediatr Infect Dis J. 2006; 25:224–229.4. Wilson CB, Nizet V, Remington JS, Klein JO, Maldonado Y. Infectious diseases of the fetus and newborn. 7th ed. Philadelphia: PA Saunders;2010.5. Fridman S, Richardson SE, Jacobs SE, O'Brien K. Systemic Candida infection in extremely low birth weight infants: short term morbidity and long term neurodevelopmental outcome. Pediatr Infect Dis J. 2000; 19:499–505.6. Devlin RK. Invasive fungal infections caused by Candida and Malassezia species in the neonatal intensive care unit. Adv Neonatal Care. 2006; 6:68–77.
Article7. Fridkin SK, Kaufman D, Edwards JR, Shetty S, Horan T. Changing incidence of Candida bloodstream infections among NICU patients in the United States: 1995–2004. Pediatrics. 2006; 117:1680–1687.
Article8. Benjamin DK, Stoll BJ, Gantz MG, Walsh MC, Sánchez PJ, Das A, et al. Neonatal candidiasis: epidemiology, risk factors, and clinical judgment. Pediatrics. 2010; 126:865–873.
Article9. Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002; 110:285–291.
Article10. Kaufman DA, Gurka MJ, Hazen KC, Boyle R, Robinson M, Grossman LB. Patterns of fungal colonization in preterm infants weighing less than 1000 grams at birth. Pediatr Infect Dis J. 2006; 25:733–737.
Article11. Fleming R, Walsh T, Anaissie E. Emerging and less common fungal pathogens. Infect Dis Clin North Am. 2002; 16:915–933.
Article12. Clark TA, Slavinski SA, Morgan J, Lott T, Arthington-Skaggs BA, Brandt ME, et al. Epidemiologic and molecular characterization of an outbreak of Candida parapsilosis bloodstream infections in a community hospital. J Clin Microbiol. 2004; 42:4468–4472.13. Young RC, Bennett JE, Vogel CL, Carbone PP, DeVita VT. The spectrum of the disease in 98 patients. Medicine. 1970; 49:147–173.
Article14. Benjamin DK, Poole C, Steinbach WJ, Rowen JL, Walsh TJ. Neonatal candidemia and end-organ damage: a critical appraisal of the literature using meta-analytic techniques. Pediatrics. 2003; 112:634–640.
Article15. Fernandez M, Moylett EH, Noyola DE, Baker CJ. Candidal meningitis in neonates: a 10-year review. Clin Infect Dis. 2000; 31:458–463.
Article16. Volpe J. Neurology of the Newborn. 4th edit. Philadelphia: WB Saunders;2001.17. Kaufman D, Fairchild KD. Clinical microbiology of bacterial and fungal sepsis in very-low-birth-weight infants. Clin Microbiol Rev. 2004; 17:638–680.
Article18. Baley JE, Kliegman RM, Fanaroff AA. Disseminated fungal infections in very low-birth-weight infants: clinical manifestations and epidemiology. Pediatrics. 1984; 73:144–152.
Article19. Ellepola A, Morrison CJ. Laboratory diagnosis of invasive candidiasis. J Microbiol. 2005; 43:65–84.20. Noyola DE, Fernandez M, Moylett EH, Baker CJ. Ophthalmologic, visceral, and cardiac involvement in neonates with candidemia. Clin Infect Dis. 2001; 32:1018–1023.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Candida albicans Brain Abscesses in Extremely Low Birth Weight Infant Treated with Amphotericin B, Flucytosine, and Fluconazole
- Follow Up Study of the Low Birth Weight Infants Less than Birth Weight 1,500 grams
- Fetal Weight for Gestational Period and Postnatal Weight Gain of Low Birth Weight Gain of Low Birth Wight Infant
- Statistical study on the incidence and mortality rate of low birth weight infant
- Clinical observation on very low birth weight infants