J Korean Neurosurg Soc.
2017 Feb;60(2):181-188. 10.3340/jkns.2016.0707.015.
What Effects Does Necrotic Area of Contrast-Enhanced MRI in Osteoporotic Vertebral Fracture Have on Further Compression and Clinical Outcome?
- Affiliations
-
- 1Department of Neurosurgery, Gyeongsang National University School of Medicine, Jinju, Korea. leeys1026@hanmail.net
- 2Department of Neurosurgery, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2374879
- DOI: http://doi.org/10.3340/jkns.2016.0707.015
Abstract
OBJECTIVE
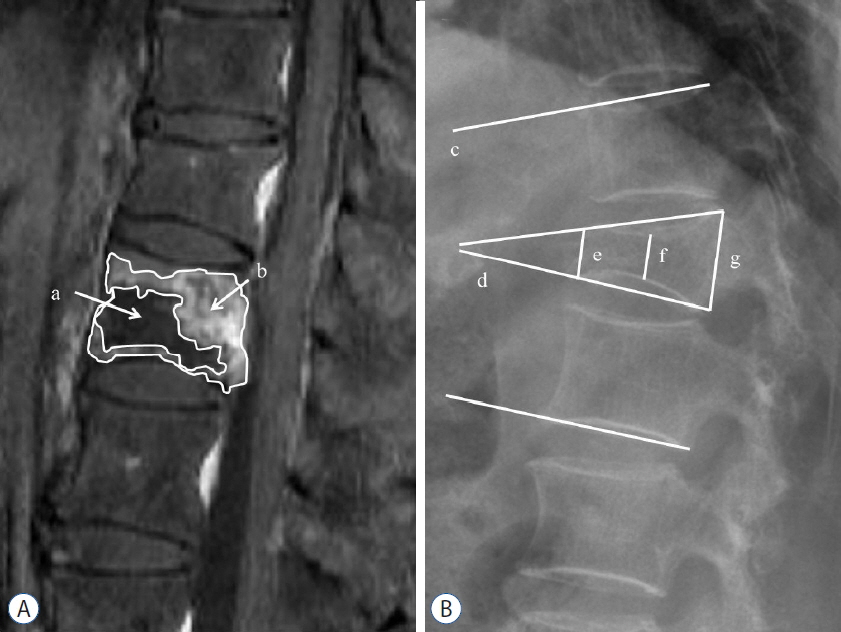
The objective of this study was to analyze the correlation between further compression and necrotic area in osteoporotic vertebral fracture (OVF) patients with contrast-enhanced magnetic resonance imaging (CEMRI). In addition, we investigated the radiological and clinical outcome according to the range of the necrotic area.
METHODS
Between 2012 and 2014, the study subjects were 82 OVF patients who did not undergo vertebroplasty or surgical treatment. The fracture areas examined on CEMRI at admission were defined as edematous if enhancement was seen and as necrotic if no enhancement was seen. The correlation between further compression and the necrotic and edematous areas of CEMRI, age, and bone mineral density was examined. Also, necrotic areas were classified into those with less than 25% (non-necrosis group) and those with more than 25% (necrosis group) according to the percentages of the entire vertebral body. For both groups, further compression and the changes in wedge and kyphotic angles were examined at admission and at 1 week, 3 months, and 6 months after admission, while the clinical outcomes were compared using the visual analog scale (VAS) and Eastern Cooperative Oncology Group (ECOG) performance status grade.
RESULTS
Further compression was 14.78±11.11% at 1 month and 21.75±14.43% at 6 months. There was a very strong correlation between the necrotic lesion of CEMRI and further compression (r=0.690, p<0.001). The compression of the necrosis group was 33.52±12.96%, which was higher than that of the non-necrosis group, 14.96±10.34% (p<0.005). Also, there was a statistically significantly higher number of intervertebral cleft development and surgical treatments being performed in the necrosis group than in the non-necrosis group (p<0.005). Moreover, there was a statistical difference in the decrease in the height of the vertebral body, and an increase was observed in the kyphotic change of wedge angle progression. There was also a difference in the VAS and ECOG performance scales.
CONCLUSION
The necrotic area of CEMRI in OVF had a strong correlation with further compression over time. In addition, with increasing necrosis, intervertebral clefts occurred more frequently, which induced kyphotic changes and resulted in poor clinical outcomes. Therefore, identifying necrotic areas by performing CEMRI on OVF patients would be helpful in determining their prognosis and treatment course.
MeSH Terms
Figure
Reference
-
References
1. Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 361:557–568. 2009.
Article2. Carlier RY, Gordji H, Mompoint DM, Vernhet N, Feydy A, Vallee C. Osteoporotic vertebral collapse: percutaneous vertebroplasty and local kyphosis correction. Radiology. 233:891–898. 2004.
Article3. Chou KN, Lin BJ, Wu YC, Liu MY, Hueng DY. Progressive kyphosis after vertebroplasty in osteoporotic vertebral compression fracture. Spine (Phila Pa 1976). 39:68–73. 2014.
Article4. Ha KY, Lee JS, Kim KW, Chon JS. Percutaneous vertebroplasty for vertebral compression fractures with and without intravertebral clefts. J Bone Joint Surg Br. 88:629–633. 2006.
Article5. Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O. European Vertebral Osteoporosis Study. Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int. 14:61–68. 2003.
Article6. Jang JS, Kim DY, Lee SH. Efficacy of percutaneous vertebroplasty in the treatment of intravertebral pseudarthrosis associated with noninfected avascular necrosis of the vertebral body. Spine (Phila Pa 1976). 28:1588–1592. 2003.
Article7. Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 361:569–579. 2009.
Article8. Kim DY, Lee SH, Jang JS, Chung SK, Lee HY. Intravertebral vacuum phenomenon in osteoporotic compression fracture: report of 67 cases with quantitative evaluation of intravertebral instability. J Neurosurg. 100(1 Suppl Spine):24–31. 2004.
Article9. McKiernan F, Jensen R, Faciszewski T. The dynamic mobility of vertebral compression fractures. J Bone Miner Res. 18:24–29. 2003.
Article10. Nieuwenhuijse MJ, van Rijswijk CS, van Erkel AR, Dijkstra SP. The intravertebral cleft in painful long-standing osteoporotic vertebral compression fractures treated with percutaneous vertebroplasty: diagnostic assessment and clinical significance. Spine (Phila Pa 1976). 37:974–981. 2012.
Article11. Oka M, Matsusako M, Kobayashi N, Uemura A, Numaguchi Y. Intravertebral cleft sign on fat-suppressed contrast-enhanced MR: correlation with cement distribution pattern on percutaneous vertebroplasty. Acad Radiol. 12:992–999. 2005.12. Ryu CW, Han H, Lee YM, Lim MK. The intravertebral cleft in benign vertebral compression fracture: the diagnostic performance of non-enhanced MRI and fat-suppressed contrast-enhanced MRI. Br J Radiol. 82:976–981. 2009.
Article13. Silverman SL, Minshall ME, Shen W, Harper KD, Xie S. Health-Related Quality of Life Subgroup of the Multiple Outcomes of Raloxifene Evaluation Study. The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: results from the Multiple Outcomes of Raloxifene Evaluation Study. Arthritis Rheum. 44:2611–2619. 2001.
Article14. Theodorou DJ. The intravertebral vacuum cleft sign. Radiology. 221:787–788. 2001.
Article15. Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 38:2028–2037. 2013.16. Vaccaro AR, Lehman RA Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 30:2325–2333. 2005.17. Wang G, Yang H, Chen K. Osteoporotic vertebral compression fractures with an intravertebral cleft treated by percutaneous balloon kyphoplasty. J Bone Joint Surg Br. 92:1553–1557. 2010.
Article18. Wang H, Sribastav SS, Ye F, Yang C, Wang J, Liu H, et al. Comparison of percutaneous vertebroplasty and balloon kyphoplasty for the treatment of single level vertebral compression fractures: a meta-analysis of the literature. Pain Physician. 18:209–222. 2015.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral Biportal Endoscopy as a Treatment for Acute Radiculopathy after Osteoporotic Lumbar Compression Fracture: A Case Report
- Magnetic Resonance Enhancement Patterns at the Different Ages of Symptomatic Osteoporotic Vertebral Compression Fractures
- Vertebroplasty in the Multiple Osteoporotic Compression Fracture
- Intraspinal Extradural Cyst Subsequent to a Vertebral Compression Fracture - A Case Report -
- The Comparison of Bone Scan and MRI in Osteoporotic Compression Fractures