J Korean Soc Radiol.
2013 Jun;68(6):503-510. 10.3348/jksr.2013.68.6.503.
Magnetic Resonance Enhancement Patterns at the Different Ages of Symptomatic Osteoporotic Vertebral Compression Fractures
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea. joonwoo2@gmail.com
- KMID: 2002903
- DOI: http://doi.org/10.3348/jksr.2013.68.6.503
Abstract
- PURPOSE
To investigate the magnetic resonance (MR) enhancement patterns of symptomatic osteoporotic vertebral compression fracture (VCF) according to the fracture age, based on the successful single-level percutaneous vertebroplasty (PVP) cases.
MATERIALS AND METHODS
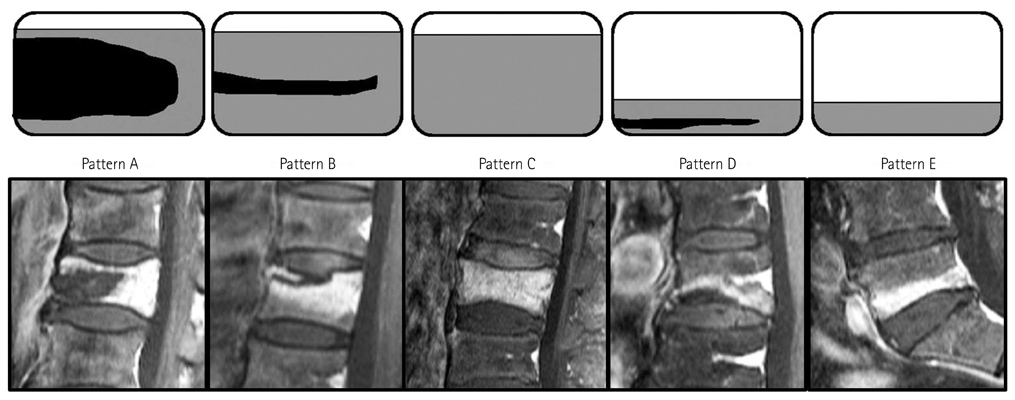
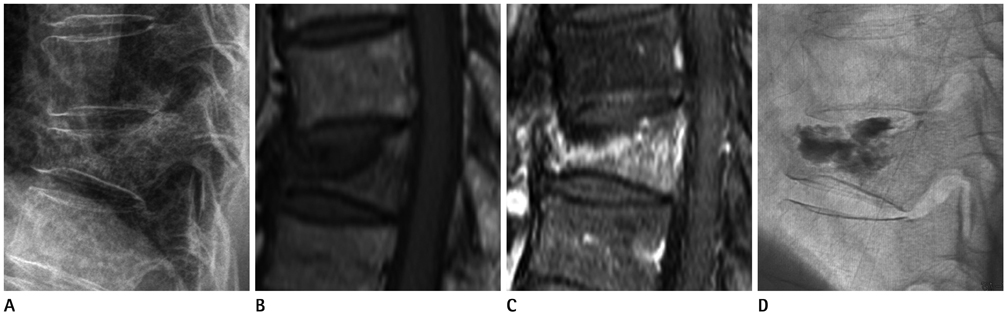
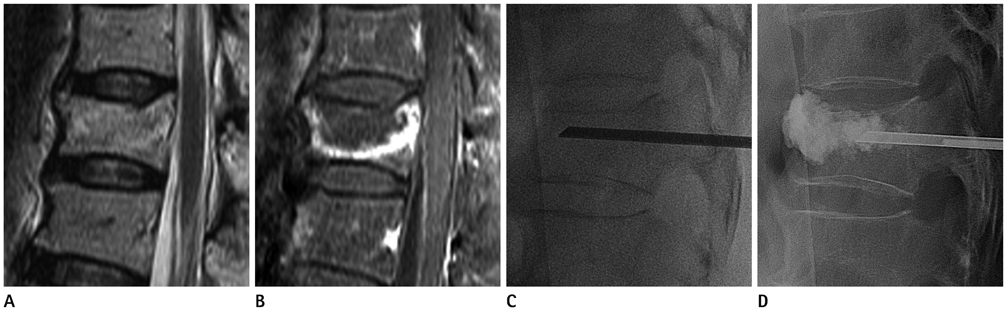
The study included 135 patients who underwent contrast-enhanced MR imaging and successful PVP from 2005 to 2010 due to a single-level osteoporotic VCF. Two radiologists blinded to the fracture age evaluated the MR enhancement patterns in consensus. The MR enhancement patterns were classified according to the enhancing proportion to the vertebral height and the presence or extent of a non-enhancing cleft within the enhancing area on sagittal plane. The Fisher' exact test, Kruskal-Wallis test and Mann-Whitney U test were performed to assess the differences in the MR enhancement patterns according to the fracture age.
RESULTS
Symptomatic VCFs show variable MR enhancement patterns in all fracture ages. A diffuse enhancing area can be seen in not only the hyperacute and acute VCFs but also the chronic symptomatic VCFs. Symptomatic VCFs having a segmental enhancing area were all included in the hyperacute or acute stage. Most symptomatic osteoporotic VCFs had a non-enhancing cleft in the enhanced vertebral body (128/135, 94.8%). There was no statistical difference of the enhancement pattern according to the fracture age.
CONCLUSION
Symptomatic VCFs show variable MR enhancement patterns in all fracture ages. The most common pattern is a non-enhancing cleft within a diffuse enhanced vertebra.
MeSH Terms
Figure
Reference
-
1. Kallmes DF, Jensen ME. Percutaneous vertebroplasty. Radiology. 2003; 229:27–36.2. Ensrud KE, Thompson DE, Cauley JA, Nevitt MC, Kado DM, Hochberg MC, et al. Fracture Intervention Trial Research Group. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. J Am Geriatr Soc. 2000; 48:241–249.3. Tanigawa N, Komemushi A, Kariya S, Kojima H, Shomura Y, Ikeda K, et al. Percutaneous vertebroplasty: relationship between vertebral body bone marrow edema pattern on MR images and initial clinical response. Radiology. 2006; 239:195–200.4. Kobayashi K, Shimoyama K, Nakamura K, Murata K. Percutaneous vertebroplasty immediately relieves pain of osteoporotic vertebral compression fractures and prevents prolonged immobilization of patients. Eur Radiol. 2005; 15:360–367.5. Chen WT, Shih TT, Chen RC, Lo SY, Chou CT, Lee JM, et al. Vertebral bone marrow perfusion evaluated with dynamic contrast-enhanced MR imaging: significance of aging and sex. Radiology. 2001; 220:213–218.6. Yamato M, Nishimura G, Kuramochi E, Saiki N, Fujioka M. MR appearance at different ages of osteoporotic compression fractures of the vertebrae. Radiat Med. 1998; 16:329–334.7. Riggs BL, Melton LJ 3rd. The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone. 1995; 17:5 Suppl. 505S–511S.8. Brown DB, Gilula LA, Sehgal M, Shimony JS. Treatment of chronic symptomatic vertebral compression fractures with percutaneous vertebroplasty. AJR Am J Roentgenol. 2004; 182:319–322.9. Cuénod CA, Laredo JD, Chevret S, Hamze B, Naouri JF, Chapaux X, et al. Acute vertebral collapse due to osteoporosis or malignancy: appearance on unenhanced and gadolinium-enhanced MR images. Radiology. 1996; 199:541–549.10. Shih TT, Huang KM, Li YW. Solitary vertebral collapse: distinction between benign and malignant causes using MR patterns. J Magn Reson Imaging. 1999; 9:635–642.11. Jung HS, Jee WH, McCauley TR, Ha KY, Choi KH. Discrimination of metastatic from acute osteoporotic compression spinal fractures with MR imaging. Radiographics. 2003; 23:179–187.12. Tan SB, Kozak JA, Mawad ME. The limitations of magnetic resonance imaging in the diagnosis of pathologic vertebral fractures. Spine (Phila Pa 1976). 1991; 16:919–923.13. Oka M, Matsusako M, Kobayashi N, Uemura A, Numaguchi Y. Intravertebral cleft sign on fat-suppressed contrast-enhanced MR: correlation with cement distribution pattern on percutaneous vertebroplasty. Acad Radiol. 2005; 12:992–999.14. Layton KF, Thielen KR, Cloft HJ, Kallmes DF. Acute vertebral compression fractures in patients with multiple myeloma: evaluation of vertebral body edema patterns on MR imaging and the implications for vertebroplasty. AJNR Am J Neuroradiol. 2006; 27:1732–1734.15. Baur A, Stäbler A, Arbogast S, Duerr HR, Bartl R, Reiser M. Acute osteoporotic and neoplastic vertebral compression fractures: fluid sign at MR imaging. Radiology. 2002; 225:730–735.16. Do HM. Magnetic resonance imaging in the evaluation of patients for percutaneous vertebroplasty. Top Magn Reson Imaging. 2000; 11:235–244.17. Dupuy DE, Palmer WE, Rosenthal DI. Vertebral fluid collection associated with vertebral collapse. AJR Am J Roentgenol. 1996; 167:1535–1538.18. Stallmeyer MJ, Zoarski GH, Obuchowski AM. Optimizing patient selection in percutaneous vertebroplasty. J Vasc Interv Radiol. 2003; 14:683–696.19. Kümmel HB. Some meandering rivers of Wisconsin. Science. 1895; 1:714–716.20. Hasegawa K, Homma T, Uchiyama S, Takahashi H. Vertebral pseudarthrosis in the osteoporotic spine. Spine (Phila Pa 1976). 1998; 23:2201–2206.21. Ito Y, Hasegawa Y, Toda K, Nakahara S. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J. 2002; 2:101–106.22. Mochida J, Toh E, Chiba M, Nishimura K. Treatment of osteoporotic late collapse of a vertebral body of thoracic and lumbar spine. J Spinal Disord. 2001; 14:393–398.23. Baba H, Maezawa Y, Kamitani K, Furusawa N, Imura S, Tomita K. Osteoporotic vertebral collapse with late neurological complications. Paraplegia. 1995; 33:281–289.24. Lane JI, Maus TP, Wald JT, Thielen KR, Bobra S, Luetmer PH. Intravertebral clefts opacified during vertebroplasty: pathogenesis, technical implications, and prognostic significance. AJNR Am J Neuroradiol. 2002; 23:1642–1646.25. Mathis JM. Percutaneous vertebroplasty: complication avoidance and technique optimization. AJNR Am J Neuroradiol. 2003; 24:1697–1706.26. Peh WC, Gelbart MS, Gilula LA, Peck DD. Percutaneous vertebroplasty: treatment of painful vertebral compression fractures with intraosseous vacuum phenomena. AJR Am J Roentgenol. 2003; 180:1411–1417.27. Kim DY, Lee SH, Jang JS, Chung SK, Lee HY. Intravertebral vacuum phenomenon in osteoporotic compression fracture: report of 67 cases with quantitative evaluation of intravertebral instability. J Neurosurg. 2004; 100:1 Suppl Spine. 24–31.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Benign compression fractures of the spine: signal patterns
- The Comparison of Bone Scan and MRI in Osteoporotic Compression Fractures
- The Factors between the Progression of the Compression Rate and Magnetic Resonance Imaging Findings in Osteoporotic Vertebral Fracture Patients Treated with Teriparatide
- Vertebroplasty in the Multiple Osteoporotic Compression Fracture
- Magnetic Resonance Enhancement Pattern as a Predictor of Cement Volume in Vertebroplasty Procedures for Osteoporotic Fractures