J Dent Anesth Pain Med.
2017 Mar;17(1):71-76. 10.17245/jdapm.2017.17.1.71.
Anesthetic management for simultaneous drug-induced sleep endoscopy and maxillomandibular advancement in a patient with obstructive sleep apnea
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Seoul National University Dental Hospital, Seoul, Korea.
- 2Department of Dental Anesthesiology, Seoul National University Dental Hospital, Seoul, Korea. stone90@snu.ac.kr
- 3Division of Oral and Maxillofacial surgery, Department of Dentistry, Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea.
- KMID: 2374727
- DOI: http://doi.org/10.17245/jdapm.2017.17.1.71
Abstract
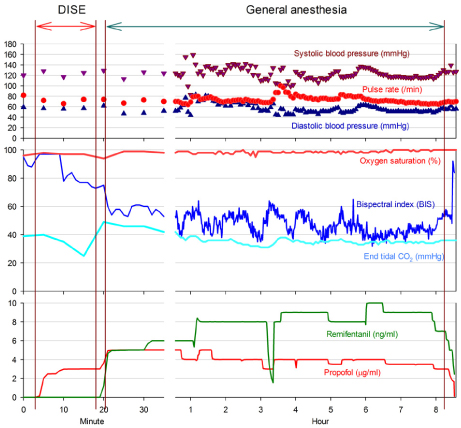
- Drug-induced sleep endoscopy (DISE) is used to identify areas of upper airway obstruction, which occurs when patients with obstructive sleep apnea (OSA) snore. DISE enables effective diagnosis and appropriate treatment of the obstruction site. Among surgical treatment methods for OSA, maxillomandibular advancement surgery (MMA) is performed to move a jaw forward; the surgery has a high success rate for OSA treatment. In DISE, anesthetics such as propofol and midazolam must be administered to induce snoring while the patient is deeply sedated for an accurate diagnosis to be made. When inducing deep sedation in a patient with OSA, airway obstruction may increase, causing oxygen saturation to drop; airway interventions are necessary in such cases. Effective DISE and MMA surgery can be performed by administering propofol through target-controlled infusion while monitoring the bispectral index (BIS).
MeSH Terms
Figure
Reference
-
1. Hong SD, Dhong HJ, Kim HY, Sohn JH, Jung YG, Chung SK, et al. Change of obstruction level during drug-induced sleep endoscopy according to sedation depth in obstructive sleep apnea. Laryngoscope. 2013; 123:2896–2899.
Article2. Croft CB, Pringle M. Sleep nasendoscopy: A technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol Allied Sci. 1991; 16:504–509.
Article3. Yoon JY, Kim EJ. Current trends in intravenous sedative drugs for dental procedures. J Dent Anesth Pain Med. 2016; 16:89–94.
Article4. Chi SI, Kim HJ, Seo KS. Dexmedetomidine intravenous sedation using a patient-controlled sedation infusion pump: A case report. J Dent Anesth Pain Med. 2016; 16:55–59.
Article5. Yoon JY, Kim CH. Dexmedetomidine: Clinical use. J Korean Dent Soc Anesthesiol. 2013; 13:161–166.
Article6. Yoon BW, Hong JM, Hong SL, Koo SK, Roh HJ, Cho KS. A comparison of dexmedetomidine versus propofol during drug-induced sleep endoscopy in sleep apnea patients. Laryngoscope. 2016; 126:763–767.
Article7. Traxdorf M, Tschaikowsky K, Scherl C, Bauer J, Iro H, Angerer F. Drug-induced sleep endoscopy (dise) with target controlled infusion (tci) and bispectral analysis in obstructive sleep apnea. J Vis Exp. 2016.
Article8. Rodrigues AP, Pinto P, Nunes B, Barbara C. Obstructive sleep apnea: Epidemiology and portuguese patients profile. Rev Port Pneumol (2006). 2017; 23:57–61.
Article9. Kim T, Kim HH, Hong S, Baek SH, Kim KW, Suh SH, et al. Change in the upper airway of patients with obstructive sleep apnea syndrome using computational fluid dynamics analysis: Conventional maxillomandibular advancement versus modified maxillomandibular advancement with anterior segmental setback osteotomy. J Craniofac Surg. 2015; 26:e765–e770.10. Doff MH, Jansma J, Schepers RH, Hoekema A. Maxillomandibular advancement surgery as alternative to continuous positive airway pressure in morbidly severe obstructive sleep apnea: A case report. Cranio. 2013; 31:246–251.
Article11. El AS, El H, Palomo JM, Baur DA. A 3-dimensional airway analysis of an obstructive sleep apnea surgical correction with cone beam computed tomography. J Oral Maxillofac Surg. 2011; 69:2424–2436.
Article12. Ratnavadivel R, Chau N, Stadler D, Yeo A, McEvoy RD, Catcheside PG. Marked reduction in obstructive sleep apnea severity in slow wave sleep. J Clin Sleep Med. 2009; 5:519–524.
Article13. Shteamer JW, Dedhia RC. Sedative choice in drug-induced sleep endoscopy: A neuropharmacology-based review. Laryngoscope. 2017; 127:273–279.
Article14. Roblin G, Williams AR, Whittet H. Target-controlled infusion in sleep endoscopy. Laryngoscope. 2001; 111:175–176.
Article15. Gillespie MB, Reddy RP, White DR, Discolo CM, Overdyk FJ, Nguyen SA. A trial of drug-induced sleep endoscopy in the surgical management of sleep-disordered breathing. Laryngoscope. 2013; 123:277–282.
Article16. Rabelo FA, Braga A, Kupper DS, De Oliveira JA, Lopes FM, de Lima Mattos PL, et al. Propofol-induced sleep: Polysomnographic evaluation of patients with obstructive sleep apnea and controls. Otolaryngol Head Neck Surg. 2010; 142:218–224.
Article17. Donaldson M, Goodchild JH. Use of bispectral index system (bis) to monitor enteral conscious (moderate) sedation during general dental procedures. J Can Dent Assoc. 2009; 75:709.18. Lo YL, Ni YL, Wang TY, Lin TY, Li HY, White DP, et al. Bispectral index in evaluating effects of sedation depth on drug-induced sleep endoscopy. J Clin Sleep Med. 2015; 11:1011–1020.
Article19. Eastwood PR, Platt PR, Shepherd K, Maddison K, Hillman DR. Collapsibility of the upper airway at different concentrations of propofol anesthesia. Anesthesiology. 2005; 103:470–477.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Skeletal Surgery in Obstructive Sleep Apnea
- The Emerging Role of Drug-Induced Sleep Endoscopy in the Management of Obstructive Sleep Apnea
- Maxillomandibular Advancement and Upper Airway Stimulation: Extrapharyngeal Surgery for Obstructive Sleep Apnea
- Microimplant mandibular advancement (MiMA) therapy for the treatment of snoring and obstructive sleep apnea (OSA)
- Maxillomandibular advancement surgery after long-term use of a mandibular advancement device in a post-adolescent patient with obstructive sleep apnea