Ann Surg Treat Res.
2017 Apr;92(4):214-220. 10.4174/astr.2017.92.4.214.
The correlation between preoperative volumetry and real graft weight: comparison of two volumetry programs
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea. kwleegs@gmail.com
- 2Department of Surgery, The Medical City Hospital, Manila, Philippines.
- 3Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2374687
- DOI: http://doi.org/10.4174/astr.2017.92.4.214
Abstract
- PURPOSE
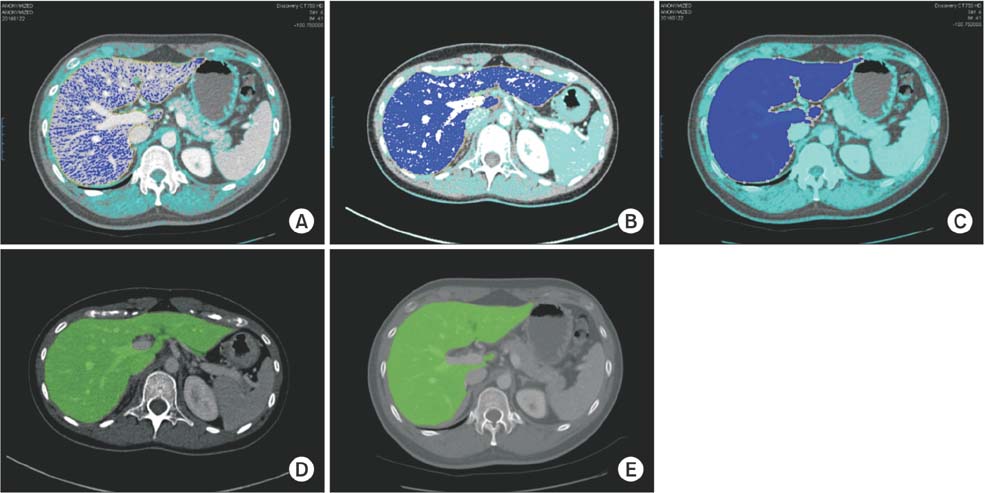
Liver volumetry is a vital component in living donor liver transplantation to determine an adequate graft volume that meets the metabolic demands of the recipient and at the same time ensures donor safety. Most institutions use preoperative contrast-enhanced CT image-based software programs to estimate graft volume. The objective of this study was to evaluate the accuracy of 2 liver volumetry programs (Rapidia vs. Dr. Liver) in preoperative right liver graft estimation compared with real graft weight.
METHODS
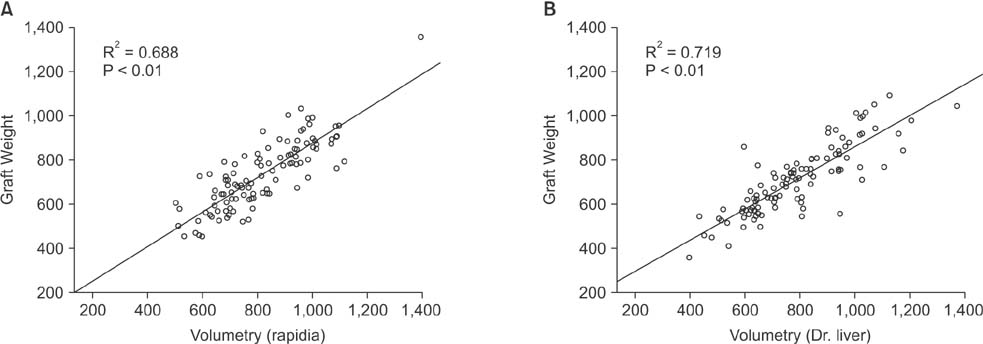
Data from 215 consecutive right lobe living donors between October 2013 and August 2015 were retrospectively reviewed. One hundred seven patients were enrolled in Rapidia group and 108 patients were included in the Dr. Liver group. Estimated graft volumes generated by both software programs were compared with real graft weight measured during surgery, and further classified into minimal difference (≤15%) and big difference (>15%). Correlation coefficients and degree of difference were determined. Linear regressions were calculated and results depicted as scatterplots.
RESULTS
Minimal difference was observed in 69.4% of cases from Dr. Liver group and big difference was seen in 44.9% of cases from Rapidia group (P = 0.035). Linear regression analysis showed positive correlation in both groups (P < 0.01). However, the correlation coefficient was better for the Dr. Liver group (R² = 0.719), than for the Rapidia group (R² = 0.688).
CONCLUSION
Dr. Liver can accurately predict right liver graft size better and faster than Rapidia, and can facilitate preoperative planning in living donor liver transplantation.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
What are the most important predictive factors for clinically relevant posthepatectomy liver failure after right hepatectomy for hepatocellular carcinoma?
Jonathan Geograpo Navarro, Seok Jeong Yang, Incheon Kang, Gi Hong Choi, Dai Hoon Han, Kyung Sik Kim, Jin Sub Choi
Ann Surg Treat Res. 2020;98(2):62-71. doi: 10.4174/astr.2020.98.2.62.
Reference
-
1. Hashikura Y, Makuuchi M, Kawasaki S, Matsunami H, Ikegami T, Nakazawa Y, et al. Successful living-related partial liver transplantation to an adult patient. Lancet. 1994; 343:1233–1234.2. Kawasaki S, Makuuchi M, Matsunami H, Hashikura Y, Ikegami T, Nakazawa Y, et al. Living related liver transplantation in adults. Ann Surg. 1998; 227:269–274.3. Tanaka K, Uemoto S, Tokunaga Y, Fujita S, Sano K, Nishizawa T, et al. Surgical techniques and innovations in living related liver transplantation. Ann Surg. 1993; 217:82–91.4. Lee SG, Park KM, Lee YJ, Hwang S, Choi DR, Ahn CS, et al. 157 adult-to-adult living donor liver transplantation. Transplant Proc. 2001; 33:1323–1325.5. Chen CL, Fan ST, Lee SG, Makuuchi M, Tanaka K. Living-donor liver transplantation: 12 years of experience in Asia. Transplantation. 2003; 75:3 Suppl. S6–S11.6. Makuuchi M, Sugawara Y. Technical progress in living donor liver transplantation for adults. HPB (Oxford). 2004; 6:95–98.7. Lo CM, Fan ST, Liu CL, Wei WI, Lo RJ, Lai CL, et al. Adult-to-adult living donor liver transplantation using extended right lobe grafts. Ann Surg. 1997; 226:261–269.8. Dahm F, Georgiev P, Clavien PA. Small-for-size syndrome after partial liver transplantation: definition, mechanisms of disease and clinical implications. Am J Transplant. 2005; 5:2605–2610.9. Nakayama Y, Li Q, Katsuragawa S, Ikeda R, Hiai Y, Awai K, et al. Automated hepatic volumetry for living related liver transplantation at multisection CT. Radiology. 2006; 240:743–748.10. Suzuki K, Epstein ML, Kohlbrenner R, Garg S, Hori M, Oto A, et al. Quantitative radiology: automated CT liver volumetry compared with interactive volumetry and manual volumetry. AJR Am J Roentgenol. 2011; 197:W706–W712.11. Bae KT, Giger ML, Chen CT, Kahn CE Jr. Automatic segmentation of liver structure in CT images. Med Phys. 1993; 20:71–78.12. Gao L, Heath DG, Kuszyk BS, Fishman EK. Automatic liver segmentation technique for three-dimensional visualization of CT data. Radiology. 1996; 201:359–364.13. Hermoye L, Laamari-Azjal I, Cao Z, Annet L, Lerut J, Dawant BM, et al. Liver segmentation in living liver transplant donors: comparison of semiautomatic and manual methods. Radiology. 2005; 234:171–178.14. Okada T, Shimada R, Hori M, Nakamoto M, Chen YW, Nakamura H, et al. Automated segmentation of the liver from 3D CT images using probabilistic atlas and multilevel statistical shape model. Acad Radiol. 2008; 15:1390–1403.15. Kim KW, Lee J, Lee H, Jeong WK, Won HJ, Shin YM, et al. Right lobe estimated blood-free weight for living donor liver transplantation: accuracy of automated blood-free CT volumetry-- preliminary results. Radiology. 2010; 256:433–440.16. Karlo C, Reiner CS, Stolzmann P, Breitenstein S, Marincek B, Weishaupt D, et al. CT- and MRI-based volumetry of resected liver specimen: comparison to intraoperative volume and weight measurements and calculation of conversion factors. Eur J Radiol. 2010; 75(1):e107–e111.17. Jung EJ, Ryu CG, Kim G, Kim SR, Park HS, Kim YJ, et al. Splenomegaly during oxaliplatin-based chemotherapy for colorectal carcinoma. Anticancer Res. 2012; 32:3357–3362.18. Perandini S, Faccioli N, Zaccarella A, Re T, Mucelli RP. The diagnostic contribution of CT volumetric rendering techniques in routine practice. Indian J Radiol Imaging. 2010; 20:92–97.19. Yang X, Yu HC, Choi Y, Lee W, Wang B, Yang J, et al. A hybrid semi-automatic method for liver segmentation based on level-set methods using multiple seed points. Comput Methods Programs Biomed. 2014; 113:69–79.20. Pomposelli JJ, Tongyoo A, Wald C, Pomfret EA. Variability of standard liver volume estimation versus software-assisted total liver volume measurement. Liver Transpl. 2012; 18:1083–1092.21. Sakamoto S, Uemoto S, Uryuhara K, Kim Id, Kiuchi T, Egawa H, et al. Graft size assessment and analysis of donors for living donor liver transplantation using right lobe. Transplantation. 2001; 71:1407–1413.22. Mokry T, Bellemann N, Muller D, Lorenzo Bermejo J, Klauß M, Stampfl U, et al. Accuracy of estimation of graft size for living-related liver transplantation: first results of a semi-automated interactive software for CT-volumetry. PLoS One. 2014; 9:e110201.23. Luciani A, Rusko L, Baranes L, Pichon E, Loze B, Deux JF, et al. Automated liver volumetry in orthotopic liver transplantation using multiphase acquisitions on MDCT. AJR Am J Roentgenol. 2012; 198:W568–W574.24. Yang X, Lee W, Choi Y, You H. Development of a user-centered virtual liver surgery planning system. In : Proceedings of the 56th Human Factors and Ergonomics Society Annual Meeting; 2012 Oct 22-26; Boston (MA), USA. Santa Monica (CA): Human Factors and Ergonomics Society;2012. p. 772–776.25. Yonemura Y, Taketomi A, Soejima Y, Yoshizumi T, Uchiyama H, Gion T, et al. Validity of preoperative volumetric analysis of congestion volume in living donor liver transplantation using three-dimensional computed tomography. Liver Transpl. 2005; 11:1556–1562.26. Kayashima H, Taketomi A, Yonemura Y, Ijichi H, Harada N, Yoshizumi T, et al. Accuracy of an age-adjusted formula in assessing the graft volume in living donor liver transplantation. Liver Transpl. 2008; 14:1366–1371.27. Choi Y, Lee JM, Yi NJ, Kim H, Park MS, Hong G, et al. Heterogeneous living donor hepatic fat distribution on MRI chemical shift imaging. Ann Surg Treat Res. 2015; 89:37–42.28. D'Onofrio M, De Robertis R, Demozzi E, Crosara S, Canestrini S, Pozzi Mucelli R. Liver volumetry: is imaging reliable? Personal experience and review of the literature. World J Radiol. 2014; 6:62–71.29. Yoneyama T, Asonuma K, Okajima H, Lee KJ, Yamamoto H, Takeichi T, et al. Coefficient factor for graft weight estimation from preoperative computed tomography volumetry in living donor liver transplantation. Liver Transpl. 2011; 17:369–372.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multivariable linear model for predicting graft weight based on 3-dimensional volumetry in regards to body weight change of living liver donor: an observational cohort study
- Multivariable linear model for predicting graft weight based on three-dimensional volumetry in regards of body weight change of living liver donor
- Clinical implication of hepatic volumetry for living donor liver transplantation
- Resection plane-dependent error in computed tomography volumetry of the right hepatic lobe in living liver donors
- Comparison of Predicted Postoperative Lung Function in Pneumonectomy Using Computed Tomography and Lung Perfusion Scans