Yonsei Med J.
2016 Jul;57(4):987-997. 10.3349/ymj.2016.57.4.987.
Standard versus Rotation Technique for Insertion of Supraglottic Airway Devices: Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea. kmsviola@yuhs.ac
- KMID: 2374134
- DOI: http://doi.org/10.3349/ymj.2016.57.4.987
Abstract
- PURPOSE
Supraglottic airway devices have been widely utilized as an alternative to tracheal intubation in various clinical situations. The rotation technique has been proposed to improve the insertion success rate of supraglottic airways. However, the clinical efficacy of this technique remains uncertain as previous results have been inconsistent, depending on the variable evaluated.
MATERIALS AND METHODS
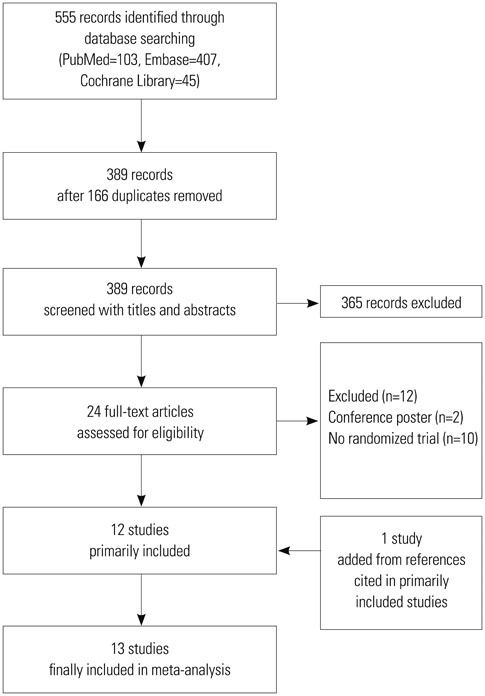
We systematically searched PubMed, Embase, and the Cochrane Central Register of Controlled Trials in April 2015 for randomized controlled trials that compared the rotation and standard techniques for inserting supraglottic airways.
RESULTS
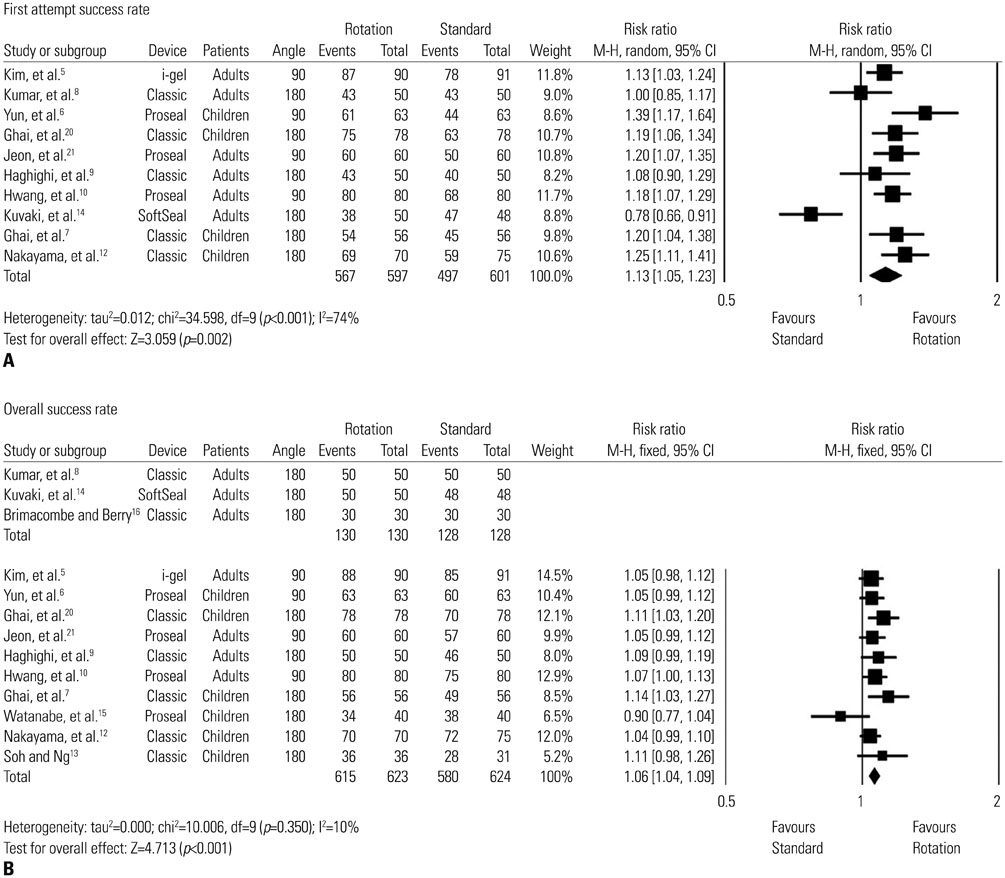
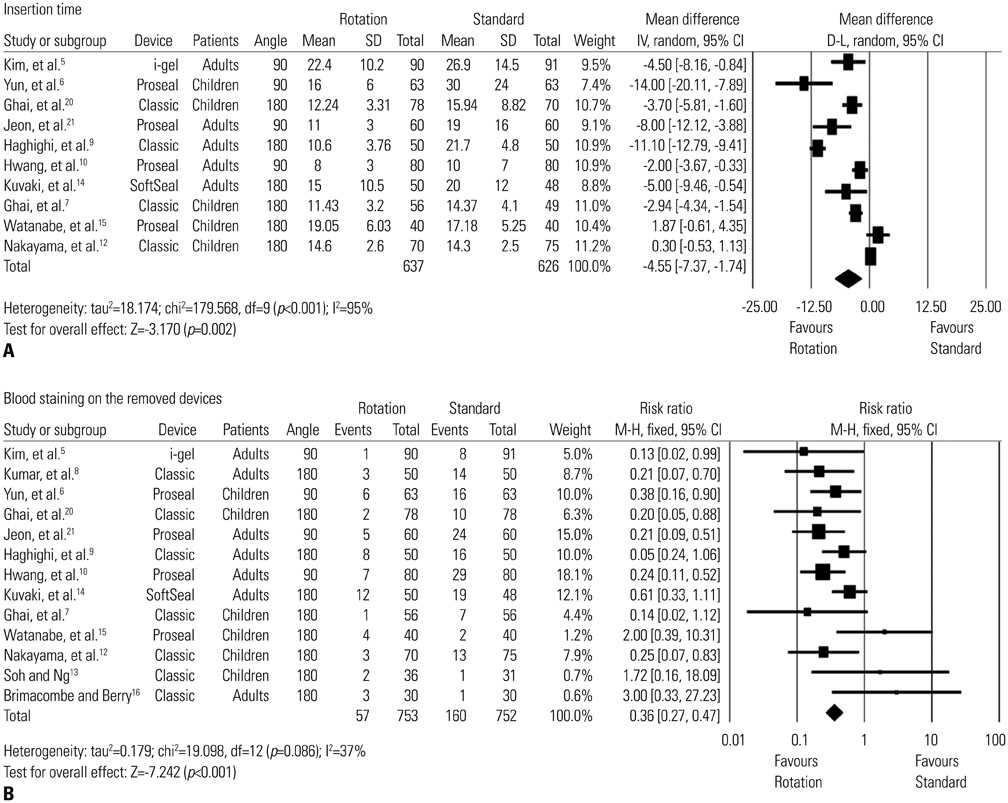
Thirteen randomized controlled trials (1505 patients, 753 with the rotation technique) were included. The success rate at the first attempt was significantly higher with the rotation technique than with the standard technique [relative risk (RR): 1.13; 95% confidence interval (CI): 1.05 to 1.23; p=0.002]. The rotation technique provided significantly higher overall success rates (RR: 1.06; 95% CI: 1.04 to 1.09; p<0.001). Device insertion was completed faster with the rotation technique (mean difference: -4.6 seconds; 95% CI: -7.37 to -1.74; p=0.002). The incidence of blood staining on the removed device (RR: 0.36; 95% CI: 0.27 to 0.47; p<0.001) was significantly lower with the rotation technique.
CONCLUSION
The rotation technique provided higher first-attempt and overall success rates, faster insertion, and a lower incidence of blood on the removed device, reflecting less mucosal trauma. Thus, it may be considered as an alternative to the standard technique when predicting or encountering difficulty in inserting supraglottic airways.
MeSH Terms
Figure
Cited by 1 articles
-
Standard digit-based versus 90° rotation technique for supraglottic airway device insertion: a meta-analysis of randomized controlled trials
Chang-Hoon Koo, Ah-Young Oh, Young-Tae Jeon, Jung-Won Hwang, Jung-Hee Ryu
Korean J Anesthesiol. 2022;75(3):266-275. doi: 10.4097/kja.21441.
Reference
-
1. Ali A, Canturk S, Turkmen A, Turgut N, Altan A. Comparison of the laryngeal mask airway Supreme and laryngeal mask airway Classic in adults. Eur J Anaesthesiol. 2009; 26:1010–1014.
Article2. An J, Shin SK, Kim KJ. Laryngeal mask airway insertion in adults: comparison between fully deflated and partially inflated technique. Yonsei Med J. 2013; 54:747–751.
Article3. Chen L, Hsiao AL. Randomized trial of endotracheal tube versus laryngeal mask airway in simulated prehospital pediatric arrest. Pediatrics. 2008; 122:e294–e297.
Article4. Goliasch G, Ruetzler A, Fischer H, Frass M, Sessler DI, Ruetzler K. Evaluation of advanced airway management in absolutely inexperienced hands: a randomized manikin trial. Eur J Emerg Med. 2013; 20:310–314.
Article5. Kim HC, Yoo DH, Kim HJ, Jeon YT, Hwang JW, Park HP. A prospective randomised comparison of two insertion methods for igel placement in anaesthetised paralysed patients: standard vs. rotational technique. Anaesthesia. 2014; 69:729–734.
Article6. Yun MJ, Hwang JW, Park SH, Han SH, Park HP, Kim JH, et al. The 90° rotation technique improves the ease of insertion of the ProSeal™ laryngeal mask airway in children. Can J Anaesth. 2011; 58:379–383.
Article7. Ghai B, Makkar JK, Bhardwaj N, Wig J. Laryngeal mask airway insertion in children: comparison between rotational, lateral and standard technique. Paediatr Anaesth. 2008; 18:308–312.
Article8. Kumar D, Khan M, Ishaq M. Rotational vs. standard smooth laryngeal mask airway insertion in adults. J Coll Physicians Surg Pak. 2012; 22:275–279.9. Haghighi M, Mohammadzadeh A, Naderi B, Seddighinejad A, Movahedi H. Comparing two methods of LMA insertion; classic versus simplified (airway). Middle East J Anaesthesiol. 2010; 20:509–514.10. Hwang JW, Park HP, Lim YJ, Do SH, Lee SC, Jeon YT. Comparison of two insertion techniques of ProSeal laryngeal mask airway: standard versus 90-degree rotation. Anesthesiology. 2009; 110:905–907.
Article11. Ghai B, Wig J. Comparison of different techniques of laryngeal mask placement in children. Curr Opin Anaesthesiol. 2009; 22:400–404.
Article12. Nakayama S, Osaka Y, Yamashita M. The rotational technique with a partially inflated laryngeal mask airway improves the ease of insertion in children. Paediatr Anaesth. 2002; 12:416–419.
Article13. Soh CR, Ng AS. Laryngeal mask airway insertion in paediatric anaesthesia: comparison between the reverse and standard techniques. Anaesth Intensive Care. 2001; 29:515–519.
Article14. Kuvaki B, Küc¸ükgüc¸lü S, Iyilikc¸i L, Tuncali BE, Cinar O. The Soft Seal disposable laryngeal mask airway in adults: comparison of two insertion techniques without intra-oral manipulation. Anaesthesia. 2008; 63:1131–1134.
Article15. Watanabe K, Nakayama S, Yamashita M. The rotational technique with ProSeal laryngeal mask airway does not improve the ease of insertion in children. Paediatr Anaesth. 2006; 16:598–599.
Article16. Brimacombe J, Berry A. Insertion of the laryngeal mask airway--a prospective study of four techniques. Anaesth Intensive Care. 1993; 21:89–92.
Article17. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6:e1000097.
Article18. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005; 5:13.
Article19. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928.
Article20. Ghai B, Ram J, Makkar JK, Wig J. Fiber-optic assessment of LMA position in children: a randomized crossover comparison of two techniques. Paediatr Anaesth. 2011; 21:1142–1147.
Article21. Jeon YT, Na HS, Park SH, Oh AY, Park HP, Yun MJ, et al. Insertion of the ProSeal laryngeal mask airway is more successful with the 90 degrees rotation technique. Can J Anaesth. 2010; 57:211–215.
Article22. Maitra S, Khanna P, Baidya DK. Comparison of laryngeal mask airway Supreme and laryngeal mask airway Pro-Seal for controlled ventilation during general anaesthesia in adult patients: systematic review with meta-analysis. Eur J Anaesthesiol. 2014; 31:266–273.
Article23. Ruetzler K, Roessler B, Potura L, Priemayr A, Robak O, Schuster E, et al. Performance and skill retention of intubation by paramedics using seven different airway devices--a manikin study. Resuscitation. 2011; 82:593–597.
Article24. Taxak S, Gopinath A. Insertion of the i-gel airway obstructed by the tongue. Anesthesiology. 2010; 112:500–501.
Article25. Cook TM, Trümpelmann P, Beringer R, Stedeford J. A randomised comparison of the Portex Softseal laryngeal mask airway with the LMA-Unique during anaesthesia. Anaesthesia. 2005; 60:1218–1225.
Article26. Brimacombe J, Keller C. Insertion of the LMA-Unique with and without digital intraoral manipulation by inexperienced personnel after manikin-only training. J Emerg Med. 2004; 26:1–5.
Article27. Aoyama K, Takenaka I, Sata T, Shigematsu A. The triple airway manoeuvre for insertion of the laryngeal mask airway in paralyzed patients. Can J Anaesth. 1995; 42:1010–1016.
Article28. Lee JJ. Laryngeal mask and trauma to uvula. Anaesthesia. 1989; 44:1014–1015.
Article29. Brain AI. An evaluation of the laryngeal mask airway during routine paediatric anaesthesia. Paediatr Anaesth. 1995; 5:75.30. Choi KW, Lee JR, Oh JT, Kim DW, Kim MS. The randomized crossover comparison of airway sealing with the laryngeal mask airway Supreme(™) at three different intracuff pressures in children. Paediatr Anaesth. 2014; 24:1080–1087.
Article31. Kim MS, Lee JH, Han SW, Im YJ, Kang HJ, Lee JR. A randomized comparison of the i-gel with the self-pressurized air-Q intubating laryngeal airway in children. Paediatr Anaesth. 2015; 25:405–412.
Article32. Brimacombe J, Berry A. A proposed fiber-optic scoring system to standardize the assessment of laryngeal mask airway position. Anesth Analg. 1993; 76:457.33. Jagannathan N, Sohn L, Ramsey M, Huang A, Sawardekar A, Sequera-Ramos L, et al. A randomized comparison between the igel™ and the air-Q™ supraglottic airways when used by anesthesiology trainees as conduits for tracheal intubation in children. Can J Anaesth. 2015; 62:587–594.
Article34. Maitra S, Baidya DK, Bhattacharjee S, Khanna P. Evaluation of igel(™) airway in children: a meta-analysis. Paediatr Anaesth. 2014; 24:1072–1079.
Article35. Brimacombe J, Keller C. The ProSeal laryngeal mask airway: a randomized, crossover study with the standard laryngeal mask airway in paralyzed, anesthetized patients. Anesthesiology. 2000; 93:104–109.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Standard digit-based versus 90° rotation technique for supraglottic airway device insertion: a meta-analysis of randomized controlled trials
- Clinical Effectiveness of Laryngeal Mask Airway ProSeal(TM), Laryngeal Tube and PAxpressTM as a Supraglottic Airway
- Use of supraglottic airway devices in children
- Comparison of the Clinical Effectiveness of the CobraTM Perilaryngeal Airway and the ProSealTM Laryngeal Mask Airway during Anesthesia with Controlled Ventilation
- Comparison of the clinical performance of the i-gelTM, LMA SupremeTM, and Ambu AuraGainTM in adult patients during general anesthesia: a prospective and randomized study