Yonsei Med J.
2016 Mar;57(2):475-481. 10.3349/ymj.2016.57.2.475.
Intrathecal Morphine Infusion Therapy in Management of Chronic Pain: Present and Future Implementation in Korea
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea. pain@snu.ac.kr
- 2Department of Anesthesiology and Pain Medicine, Chonnam National University Hospital, Gwangju, Korea.
- KMID: 2374056
- DOI: http://doi.org/10.3349/ymj.2016.57.2.475
Abstract
- PURPOSE
Intrathecal morphine pump (ITMP) infusion therapy is efficient in managing malignant and nonmalignant chronic pain refractory to standard treatment. However, the high cost of an ITMP is the greatest barrier for starting a patient on ITMP infusion therapy. Using the revised Korean reimbursement guidelines, we investigated the cost effectiveness of ITMP infusion therapy and conducted a patient survey.
MATERIALS AND METHODS
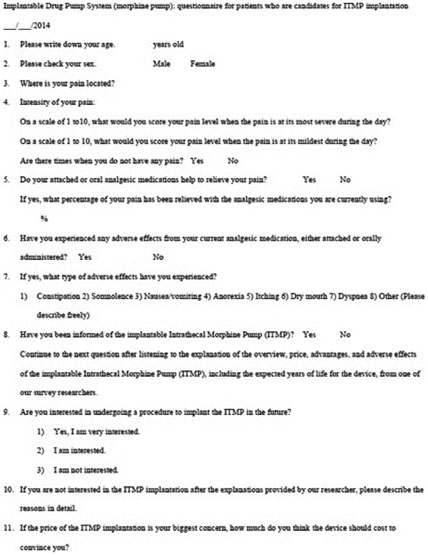
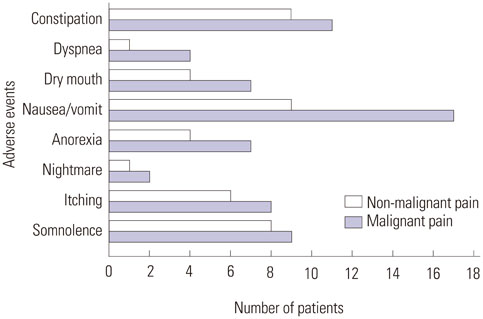
A retrospective chart review of 12 patients who underwent ITMP implantation was performed. Morphine dose escalation rates were calculated, and numeric rating scale (NRS) scores were compared before and after ITMP implantation. We surveyed patients who were already using an ITMP as well as those who were candidates for an ITMP. All survey data were collected through in-person interviews over 3 months. Data on the cost of medical treatment were collected and projected over time.
RESULTS
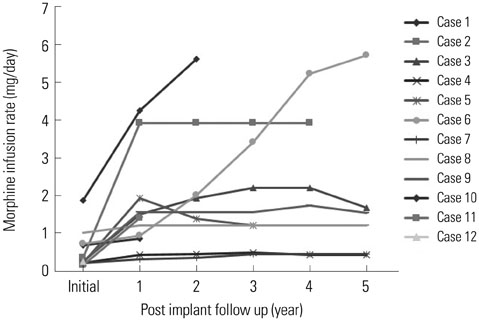
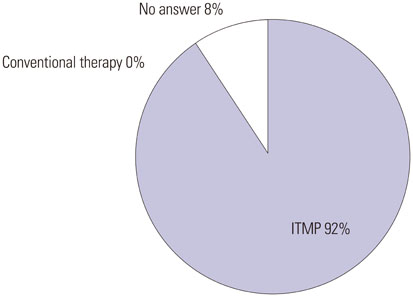
The NRS score decreased during the follow-up period. The median morphine dose increased by 36.9% over the first year, and the median time required to reach a financial break-even point was 24.2 months. Patients were more satisfied with the efficacy of ITMP infusion therapy than with conventional therapy. The expected cost of ITMP implantation was KRW 4000000-5000000 in more than half of ITMP candidates scheduled to undergo implantation.
CONCLUSION
The high cost of initiating ITMP infusion therapy is challenging; however, the present results may encourage more patients to consider ITMP therapy.
Keyword
MeSH Terms
-
Adult
Aged
Analgesics, Opioid/*administration & dosage/economics/therapeutic use
Chronic Pain/*drug therapy
Cost-Benefit Analysis
Female
Humans
Infusion Pumps, Implantable/*economics
Injections, Spinal
Male
Middle Aged
Morphine/*administration & dosage/economics/therapeutic use
Pain Management/*methods/trends
Patient Satisfaction
Republic of Korea
Retrospective Studies
Surveys and Questionnaires
Treatment Outcome
Analgesics, Opioid
Morphine
Figure
Cited by 1 articles
-
Retrospective analysis of the financial break-even point for intrathecal morphine pump use in Korea
Eun Kyoung Kim, Ji Yeon Shin, Anyela Marcela Castañeda, Seung Jae Lee, Hyun Kyu Yoon, Yong Chul Kim, Jee Youn Moon
Korean J Pain. 2017;30(4):272-280. doi: 10.3344/kjp.2017.30.4.272.
Reference
-
1. Ministry of Health and Welfare. accessed on 2014 Jul 2. Available at: http://www.mohw.go.kr.2. Jo HS, Kwon MS, Jung SM, Lee BY. Awareness of cancer and cancer screening by Korean community residents. Asian Pac J Cancer Prev. 2014; 15:4939–4944.
Article3. Nuland SB. Physician-assisted suicide and euthanasia in practice. N Engl J Med. 2000; 342:583–584.
Article4. Von Roenn JH, Cleeland CS, Gonin R, Hatfield AK, Pandya KJ. Physician attitudes and practice in cancer pain management. A survey from the Eastern Cooperative Oncology Group. Ann Intern Med. 1993; 119:121–126.
Article5. Cleeland CS. Undertreatment of cancer pain in elderly patients. JAMA. 1998; 279:1914–1915.
Article6. Wang JK, Nauss LA, Thomas JE. Pain relief by intrathecally applied morphine in man. Anesthesiology. 1979; 50:149–151.
Article7. Wiffen PJ, Wee B, Moore RA. Oral morphine for cancer pain. Cochrane Database Syst Rev. 2013; 7:CD003868.
Article8. Onofrio BM. Treatment of chronic pain of malignant origin with intrathecal opiates. Clin Neurosurg. 1983; 31:304–315.
Article9. Nguyen H, Hassenbusch SJ. Cost-effectiveness of intraspinal drug delivery for chronic pain. Semin Pain Med. 2004; 2:43–45.
Article10. Lee SJ, Nam SK, Kim JH, Kim HJ, Lee SC, Kim YC. Implantation of an intrathecal drug administration system - a report of two cases. Korean J Pain. 2009; 22:68–73.
Article11. Roberts LJ, Finch PM, Goucke CR, Price LM. Outcome of intrathecal opioids in chronic non-cancer pain. Eur J Pain. 2001; 5:353–361.
Article12. Rauck RL, Cherry D, Boyer MF, Kosek P, Dunn J, Alo K. Long-term intrathecal opioid therapy with a patient-activated, implanted delivery system for the treatment of refractory cancer pain. J Pain. 2003; 4:441–447.
Article13. Upadhyay SP, Mallick PN. Intrathecal drug delivery system (IDDS) for cancer pain management: a review and updates. Am J Hosp Palliat Care. 2012; 29:388–398.
Article14. Deer TR, Krames E, Levy RM, Hassenbusch SJ 3rd, Prager JP. Practice choices and challenges in the current intrathecal therapy environment: an online survey. Pain Med. 2009; 10:304–309.
Article15. Duarte RV, Raphael JH, Haque MS, Southall JL, Ashford RL. A predictive model for intrathecal opioid dose escalation for chronic non-cancer pain. Pain Physician. 2012; 15:363–369.16. Mekhail N, Mahboobi R, Farajzadeh Deroee A, Costandi S, Dalton J, Guirguis M, et al. Factors that might impact intrathecal drug delivery (IDD) dose escalation: a longitudinal study. Pain Pract. 2014; 14:301–308.
Article17. Foley KM. The treatment of cancer pain. N Engl J Med. 1985; 313:84–95.
Article18. Atli A, Theodore BR, Turk DC, Loeser JD. Intrathecal opioid therapy for chronic nonmalignant pain: a retrospective cohort study with 3-year follow-up. Pain Med. 2010; 11:1010–1016.
Article19. Malhotra VT, Root J, Kesselbrenner J, Njoku I, Cubert K, Gulati A, et al. Intrathecal pain pump infusions for intractable cancer pain: an algorithm for dosing without a neuraxial trial. Anesth Analg. 2013; 116:1364–1370.20. Brogan SE, Winter NB, Abiodun A, Safarpour R. A cost utilization analysis of intrathecal therapy for refractory cancer pain: identifying factors associated with cost benefit. Pain Med. 2013; 14:478–486.
Article21. Mueller-Schwefe G, Hassenbusch SJ, Reig E. Cost effectiveness of intrathecal therapy for pain. Neuromodulation. 1999; 2:77–87.
Article22. Ver Donck A, Vranken JH, Puylaert M, Hayek S, Mekhail N, Van Zundert J. Intrathecal drug administration in chronic pain syndromes. Pain Pract. 2014; 14:461–476.
Article23. Hayek SM, Deer TR, Pope JE, Panchal SJ, Patel VB. Intrathecal therapy for cancer and non-cancer pain. Pain Physician. 2011; 14:219–248.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Continuous Intraventricular Morphine Infusion for Control of Pain in Terminal Cancer Patients
- Implantation of an Intrathecal Drug Administration System : A report of two cases
- Catheter Obstruction of Intrathecal Drug Administration System: A Case Report
- Intrathecal and Epidural Morphine for Postoperative Pain Control after Lumbar Laminectomy
- Treatment of Urinary Rstsntion due to Intrathecal Injection of Morphine