J Gastric Cancer.
2014 Mar;14(1):47-53.
Clinical Application of Electrogastrography in Patients with Stomach Cancer Who Undergo Distal Gastrectomy
- Affiliations
-
- 1Department of Surgery, Kyung Hee University School of Medicine, Seoul, Korea. kyjho@khmc.or.kr
Abstract
- PURPOSE
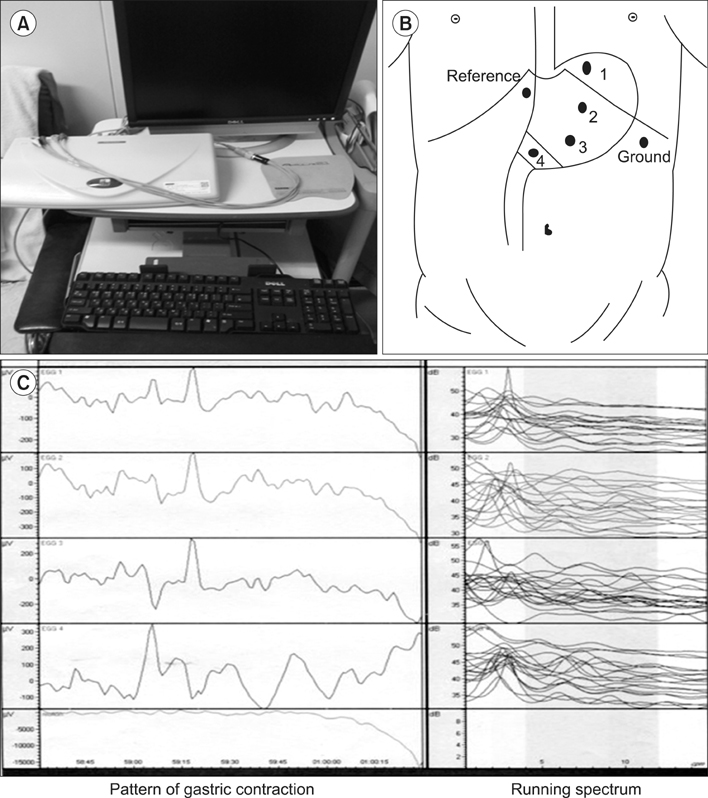
Electrogastrography is a method of measuring action potentials of the stomach. The purpose of this study was to investigate early postoperative changes in the electrogastrography and determine the correlation between electrogastrography and quality of life of patients with stomach cancer who underwent distal gastrectomy.
MATERIALS AND METHODS
This study analyzed 20 patients with stomach cancer who underwent electrogastrography and quality of life was measured 1, 12, and 24 weeks after the operation. Quality of life-C30 version 3.0 and quality of life-STO22, were used.
RESULTS
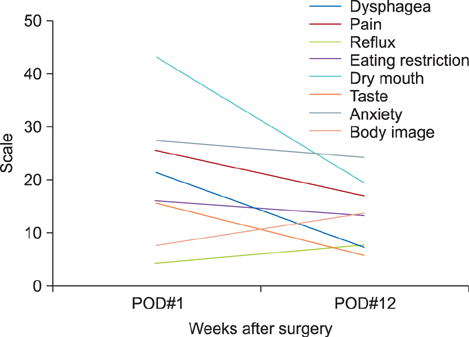
Fasting and postprandial mean dominant frequency at 1 week after the operation was 2.7 and 2.7 cycles per minute, and 2.8 and 2.7 cycles per minute at 12 weeks, 2.6 and 2.8 cycles per minute at 24 weeks. Fasting and postprandial mean dominant power at 1 week was 36.5 and 36.4 dB, 36.3 and 40.1 dB at 12 weeks and 40.9 and 42.3 dB at 24 weeks. The percentage of tachygastria was increased whereas the percentage of bradygradia was decreased during the postoperative periods (P<0.05). Global health, physical, emotional and social functioning scales were improved, but role and cognitive functioning were not changed. Pain, insomnia, diarrhea and financial difficulties were significantly improved according to the postoperative periods (P<0.05). The correlation between the STO22 and electrogastrography parameters was not significant (P>0.05).
CONCLUSIONS
These may suggest that electrogastrography is a simple and noninvasive method and may be applicated for evaluating motility and autonomic functions of the remnant stomach.
MeSH Terms
Figure
Reference
-
1. Quigley EMM. Gastric motor and sensory function and motor disorders of the stomach. In : Feldman M, Friedman LS, Brandt LJ, editors. Sleisenger & Fordtran's Gastrointestinal and Liver Disease Pathophysiology/Diagnosis/Management. 8th ed. Philadelphia: WB Saunders/Elsevier;2006. p. 999–1028.2. Parkman HP, Hasler WL, Barnett JL, Eaker EY. American Motility Society Clinical GI Motility Testing Task Force. Electrogastrography: a document prepared by the gastric section of the American Motility Society Clinical GI Motility Testing Task Force. Neurogastroenterol Motil. 2003; 15:89–102.
Article3. Alvarez WC. The electrogastrogram and what it shows. JAMA. 1922; 78:1116–1119.
Article4. Yin J, Chen JD. Roles of interstitial cells of Cajal in regulating gastrointestinal motility: in vitro versus in vivo studies. J Cell Mol Med. 2008; 12:1118–1129.
Article5. Smout AJPM, Jebbink HJA, Samson JM. Acquisition and analysis of electrogastrographic data, the Dutch experience. In : Chen JZ, McCallum RW, editors. Electrogastrography, Principles and Applications. New York: Raven Press;1994. p. 3–30.6. Chang FY. Electrogastrography: basic knowledge, recording, processing and its clinical applications. J Gastroenterol Hepatol. 2005; 20:502–516.
Article7. Hinder RA, Kelly KA. Human gastric pacesetter potential. Site of origin, spread, and response to gastric transection and proximal gastric vagotomy. Am J Surg. 1977; 133:29–33.8. Sarna SK, Bowes KL, Daniel EE. Gastric pacemakers. Gastroenterology. 1976; 70:226–231.
Article9. Chen JD, McCallum RW. Clinical applications of electrogastrography. Am J Gastroenterol. 1993; 88:1324–1336.10. Chen JD, Richards RD, McCallum RW. Identification of gastric contractions from the cutaneous electrogastrogram. Am J Gastroenterol. 1994; 89:79–85.11. Sun WM, Smout A, Malbert C, Edelbroek MA, Jones K, Dent J, et al. Relationship between surface electrogastrography and antropyloric pressures. Am J Physiol. 1995; 268:G424–G430.
Article12. van Dielen FM, de Cock AF, Daams F, Brummer RJ, Greve JW. Gastric myoelectrical activity in morbidly obese patients before and 3 months after gastric restrictive surgery. Obes Surg. 2003; 13:721–727.
Article13. Richter HM 3rd. Physiologic consequences of vagotomy and gastric resection. Gastroenterol Clin North Am. 1994; 23:193–213.
Article14. Mackay S, Hayes T, Yeo A. Management of gastric cancer. Aust Fam Physician. 2006; 35:208–211.15. Houghton J, Wang TC. Tumors of the stomach. In : Feldman M, Friedman LS, Brandt LJ, editors. Sleisenger & Fordtran's Gastrointestinal and Liver disease, Pathophysiology/Diagnosis/Management. 8th ed. Philadelphia: WB Saunders/Elsevier;2006. p. 1139–1170.16. Carter DC. Carcinoma of the stomach and other tumors. In : Shearman DJC, Finlayson N, Camilleri M, Carter SD, editors. Diseases of the Gastrointestinal Tract and Liver. 3rd ed. New York: Churchill Livingstone;1997. p. 293–322.17. Zhang Q, Yu JC, Ma ZQ, Kang WM, Ke MY, Qian JM. The effects of enteral nutrition vs parenteral nutrition on gastric motility and gastroenteric hormones after subtotal gastrectomy: a perspective randomized compared clinical trial. Zhonghua Wai Ke Za Zhi. 2006; 44:728–732.18. Lee HF, Chang FY, Lu CL, Luo JC, Chen CY, Wu HC. Electrogastrographic characteristics in subjects with stomach remnant. J Gastroenterol Hepatol. 2010; 25:339–344.
Article19. Homma S, Kobayashi Y, Kosugi S, Ohashi M, Kanda T, Okamoto H, et al. Postoperative reorganization of gastric pacemaker activity in patients after an extended period following distal gastrectomy. J Smooth Muscle Res. 2008; 44:113–122.
Article20. Imai K, Sakita M. Pre- and postoperative electrogastrography in patients with gastric cancer. Hepatogastroenterology. 2005; 52:639–644.21. Hayashi T, Kinami S, Fushida S, Fujimura T, Miwa K, Inoue K. Evaluation of residual stomach motility after proximal gastrectomy for gastric cancer by electrogastrography. Dig Dis Sci. 2006; 51:268–273.
Article22. Koch KL. Electrogastrography: physiological basis and clinical application in diabetic gastropathy. Diabetes Technol Ther. 2001; 3:51–62.
Article23. Camilleri M, Hasler WL, Parkman HP, Quigley EM, Soffer E. Measurement of gastrointestinal motility in the GI laboratory. Gastroenterology. 1998; 115:747–762.
Article24. Riezzo G, Chiloiro M, Guerra V. Electrogastrography in healthy children: evaluation of normal values, influence of age, gender, and obesity. Dig Dis Sci. 1998; 43:1646–1651.25. Cheung B, Vaitkus P. Perspectives of electrogastrography and motion sickness. Brain Res Bull. 1998; 47:421–431.
Article26. You CH, Chey WY, Lee KY, Menguy R, Bortoff A. Gastric and small intestinal myoelectric dysrhythmia associated with chronic intractable nausea and vomiting. Ann Intern Med. 1981; 95:449–451.
Article27. van der Schee EJ, Grashuis JL. Contraction-related, low-frequency components in canine electrogastrographic signals. Am J Physiol. 1983; 245:G470–G475.
Article28. Bracci F, Matarazzo E, Mosiello G, Caione P, Cianchi D, Ponticelli A. Preliminary report of electrogastrography in pediatric gastroresection: can it be predictive of alteration of gastric motility? J Pediatr Surg. 2001; 36:1157–1159.
Article29. Bures J, Kabelác K, Kopácová M, Vorísek V, Siroký M, Palicka V, et al. Electrogastrography in patients with Roux-en-Y reconstruction after previous Billroth gastrectomy. Hepatogastroenterology. 2008; 55:1492–1496.30. Murakami H, Matsumoto H, Kubota H, Higashida M, Nakamura M, Hirai T. Evaluation of electrical activity after vagus nerve-preserving distal gastrectomy using multichannel electrogastrography. J Smooth Muscle Res. 2013; 49:1–14.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Distal Gastrectomy for Gastric Cancer
- Comparison of a Postoperative Pain in Laparoscopy-Assisted Distal Gastrectomy and Totally Laparoscopic Distal Gastrectomy according to the Location of the Mini-Laparotomy Site
- Clinical analysis of 123 cases of total gastrectomy in the treatment of stomach cancer
- Setting the Stomach Transection Line Based on Anatomical Landmarks in Laparoscopic Distal Gastrectomy
- Comparison of Post-Operative Nutritional Status according to the Extent of Gastrectomy and the Reconstruction Method in Patients with Gastric Cancer