J Gastric Cancer.
2015 Mar;15(1):53-57. 10.5230/jgc.2015.15.1.53.
Setting the Stomach Transection Line Based on Anatomical Landmarks in Laparoscopic Distal Gastrectomy
- Affiliations
-
- 1Department of Surgery, Toyooka Hospital, Hyogo, Japan. hisahoso@kuhp.kyoto-u.ac.jp
- 2Department of Surgery, Osaka Red Cross Hospital, Osaka, Japan.
- KMID: 2372371
- DOI: http://doi.org/10.5230/jgc.2015.15.1.53
Abstract
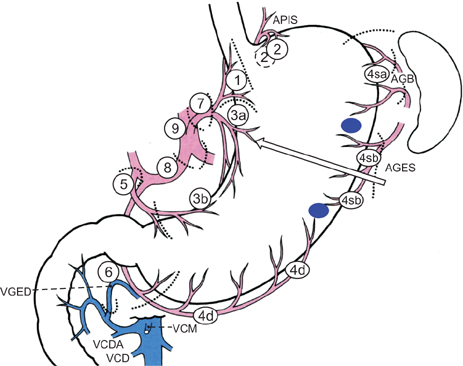
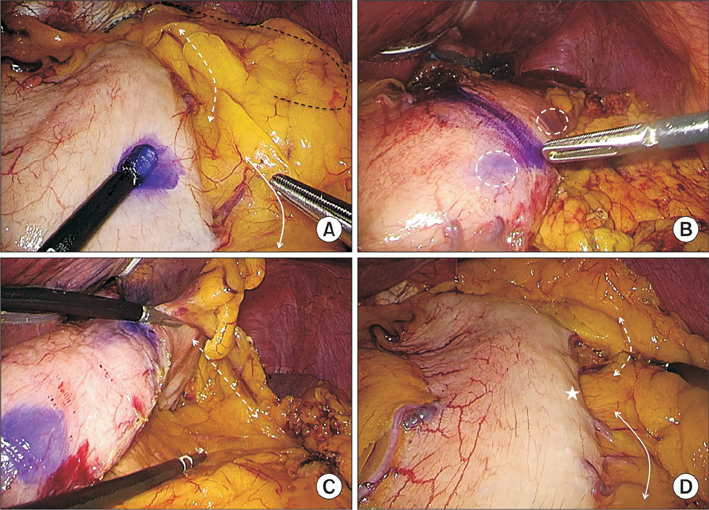
- Laparoscopic distal gastrectomy has become widespread as a treatment for early gastric cancer in eastern Asia, but a standard method for setting the stomach transection line has not been established. Here we report a novel method of setting this line based on anatomical landmarks. At the start of the operation, two anatomical landmarks along the greater curvature of the stomach were marked with ink: the proximal landmark at the avascular area between the last branch of the short gastric artery and the first branch of the left gastroepiploic artery, and the distal landmark at the point of communication between the right and left gastroepiploic arteries. Just before specimen retrieval, the stomach was transected from the center of these two landmarks toward the lesser curvature. Then, about two-third of the stomach was reproducibly resected, and gastroduodenostomy was successfully performed in 26 consecutive cases. This novel method could be used as a standard technique for setting the transection line in laparoscopic distal gastrectomy.
Figure
Reference
-
1. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg. 2002; 195:284–287.2. Kanaya S, Haruta S, Kawamura Y, Yoshimura F, Inaba K, Hiramatsu Y, et al. Video: laparoscopy distinctive technique for suprapancreatic lymph node dissection: medial approach for laparoscopic gastric cancer surgery. Surg Endosc. 2011; 25:3928–3929.3. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.4. UICC International Union Against Cancer. TNM classification of malignant tumours. 7th ed. New York: Wiley;2009. p. 73–77.5. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196.6. Kanaya S, Kawamura Y, Kawada H, Iwasaki H, Gomi T, Satoh S, et al. The delta-shaped anastomosis in laparoscopic distal gastrectomy: analysis of the initial 100 consecutive procedures of intracorporeal gastroduodenostomy. Gastric Cancer. 2011; 14:365–371.7. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112.8. Nomura E, Lee SW, Bouras G, Tokuhara T, Hayashi M, Hiramatsu M, et al. Functional outcomes according to the size of the gastric remnant and type of reconstruction following laparoscopic distal gastrectomy for gastric cancer. Gastric Cancer. 2011; 14:279–284.9. Takeda FR, Cecconello I, Szachnowicz S, Tacconi MR, Gama-Rodrigues J. Anatomic study of gastric vascularization and its relationship to cervical gastroplasty. J Gastrointest Surg. 2005; 9:132–137.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of a Postoperative Pain in Laparoscopy-Assisted Distal Gastrectomy and Totally Laparoscopic Distal Gastrectomy according to the Location of the Mini-Laparotomy Site
- Laparoscopic Distal Gastrectomy for Gastric Cancer
- Comparison of Laparoscopy-Assisted and Totally Laparoscopic Distal Gastrectomy: The Short-Term Outcome at a Low Volume Center
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Comparison of laparoscopy-assisted and totally laparoscopic Billroth-II distal gastrectomy for gastric cancer