Ann Rehabil Med.
2016 Dec;40(6):1100-1107. 10.5535/arm.2016.40.6.1100.
Change of Swallowing in Patients With Head and Neck Cancer After Concurrent Chemoradiotherapy
- Affiliations
-
- 1Department of Rehabilitation Medicine, Chungnam National University Hospital, Daejeon, Korea. drjeesungju@cnuh.co.kr
- 2Department of Otolaryngology-Head and Neck Surgery, Chungnam National University Hospital, Daejeon, Korea.
- KMID: 2371343
- DOI: http://doi.org/10.5535/arm.2016.40.6.1100
Abstract
OBJECTIVE
To evaluate the functional characteristics of swallowing and to analyze the parameters of dysphagia in head and neck cancer patients after concurrent chemoradiotherapy (CCRT).
METHODS
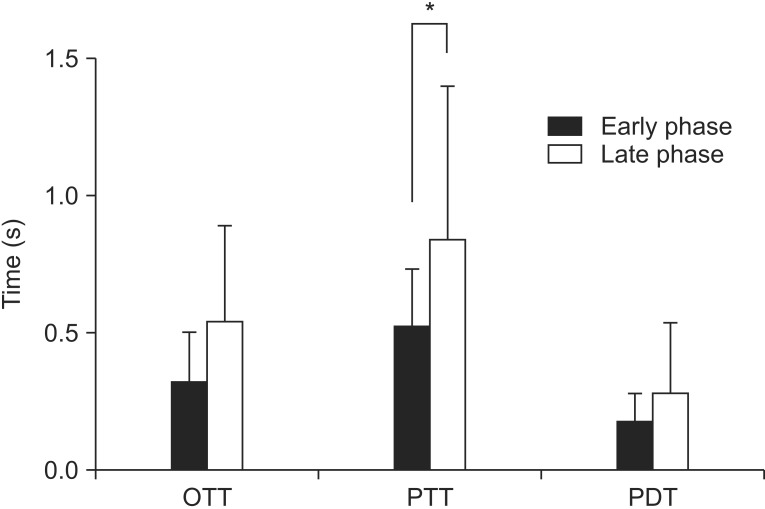
The medical records of 32 patients with head and neck cancer who were referred for a videofluoroscopic swallowing study from January 2012 to May 2015 were retrospectively reviewed. The patients were allocated by duration after starting CCRT into early phase (<1 month after radiation therapy) and late phase (>1 month after radiation therapy) groups. We measured the modified penetration aspiration scale (MPAS) and American Speech-Language-Hearing Association National Outcome Measurement System swallowing scale (ASHA-NOMS). The oral transit time (OTT), pharyngeal delay time (PDT), and pharyngeal transit time (PTT) were recorded to assess the swallowing physiology.
RESULTS
Among 32 cases, 18 cases (56%) were of the early phase. In both groups, the most common tumor site was the hypopharynx (43.75%) with a histologic type of squamous cell carcinoma (75%). PTT was significantly longer in the late phase (p=0.03). With all types of boluses, except for soup, both phases showed a statistically significant difference in MPAS results. The mean ASHA-NOMS level for the early phase was 5.83±0.78 and that for the late phase was 3.79±1.80, with statistical significance (p=0.01). The PTT and ASHA-NOMS level showed a statistically significant correlation (correlation coefficient=-0.52, p=0.02). However, it showed no relationship with the MPAS results.
CONCLUSION
The results of our study suggest that in the late phase that after CCRT, the OTT, PDT, and PTT were longer than in the early phase and the PTT prolongation was statistically significant. Therefore, swallowing therapy targeting the pharyngeal phase is recommended after CCRT.
MeSH Terms
Figure
Cited by 1 articles
-
Acoustic Voice Analysis in Patients with Penetration/Aspiration Via Videofluoroscopic Swallowing Study
Young Ae Kang, Sung Ju Jee, Bon Seok Koo
Korean J Otorhinolaryngol-Head Neck Surg. 2017;60(9):454-462. doi: 10.3342/kjorl-hns.2017.00213.
Reference
-
1. Parsons JT, Mendenhall WM, Million RR, Stringer SP, Cassisi NJ. The management of primary cancers of the oropharynx: combined treatment or irradiation alone? Semin Radiat Oncol. 1992; 2:142–148. PMID: 10717029.
Article2. Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, Leemans CR, Aaronson NK, Slotman BJ. Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol. 2008; 26:3770–3776. PMID: 18669465.
Article3. Kao J, Lavaf A, Teng MS, Huang D, Genden EM. Adjuvant radiotherapy and survival for patients with node-positive head and neck cancer: an analysis by primary site and nodal stage. Int J Radiat Oncol Biol Phys. 2008; 71:362–370. PMID: 18164833.
Article4. Lavaf A, Genden EM, Cesaretti JA, Packer S, Kao J. Adjuvant radiotherapy improves overall survival for patients with lymph node-positive head and neck squamous cell carcinoma. Cancer. 2008; 112:535–543. PMID: 18076014.
Article5. Epstein JB, Robertson M, Emerton S, Phillips N, Stevenson-Moore P. Quality of life and oral function in patients treated with radiation therapy for head and neck cancer. Head Neck. 2001; 23:389–398. PMID: 11295813.
Article6. Rosenthal DI, Lewin JS, Eisbruch A. Prevention and treatment of dysphagia and aspiration after chemoradiation for head and neck cancer. J Clin Oncol. 2006; 24:2636–2643. PMID: 16763277.
Article7. Rademaker AW, Vonesh EF, Logemann JA, Pauloski BR, Liu D, Lazarus CL, et al. Eating ability in head and neck cancer patients after treatment with chemoradiation: a 12-month follow-up study accounting for dropout. Head Neck. 2003; 25:1034–1041. PMID: 14648862.
Article8. Caudell JJ, Schaner PE, Meredith RF, Locher JL, Nabell LM, Carroll WR, et al. Factors associated with long-term dysphagia after definitive radiotherapy for locally advanced head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2009; 73:410–415. PMID: 18635320.
Article9. Garcia-Peris P, Paron L, Velasco C, de la Cuerda C, Camblor M, Breton I, et al. Long-term prevalence of oropharyngeal dysphagia in head and neck cancer patients: impact on quality of life. Clin Nutr. 2007; 26:710–717. PMID: 17954003.10. Eisbruch A, Lyden T, Bradford CR, Dawson LA, Haxer MJ, Miller AE, et al. Objective assessment of swallowing dysfunction and aspiration after radiation concurrent with chemotherapy for head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2002; 53:23–28. PMID: 12007937.
Article11. Dysphagia Section, Oral Care Study Group, Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO). Raber-Durlacher JE, Brennan MT, Verdonck-de Leeuw IM, et al. Swallowing dysfunction in cancer patients. Support Care Cancer. 2012; 20:433–443. PMID: 22205548.
Article12. Delanian S, Lefaix JL, Pradat PF. Radiation-induced neuropathy in cancer survivors. Radiother Oncol. 2012; 105:273–282. PMID: 23245644.
Article13. Jensen K, Lambertsen K, Grau C. Late swallowing dysfunction and dysphagia after radiotherapy for pharynx cancer: frequency, intensity and correlation with dose and volume parameters. Radiother Oncol. 2007; 85:74–82. PMID: 17673322.
Article14. Nguyen NP, Frank C, Moltz CC, Vos P, Smith HJ, Bhamidipati PV, et al. Aspiration rate following chemoradiation for head and neck cancer: an underreported occurrence. Radiother Oncol. 2006; 80:302–306. PMID: 16890314.
Article15. Lazarus CL, Logemann JA, Pauloski BR, Colangelo LA, Kahrilas PJ, Mittal BB, et al. Swallowing disorders in head and neck cancer patients treated with radiotherapy and adjuvant chemotherapy. Laryngoscope. 1996; 106(9 Pt 1):1157–1166. PMID: 8822723.
Article16. Nguyen NP, Moltz CC, Frank C, Vos P, Smith HJ, Karlsson U, et al. Dysphagia following chemoradiation for locally advanced head and neck cancer. Ann Oncol. 2004; 15:383–388. PMID: 14998839.
Article17. Eisbruch A, Schwartz M, Rasch C, Vineberg K, Damen E, Van As CJ, et al. Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys. 2004; 60:1425–1439. PMID: 15590174.
Article18. Kotz T, Costello R, Li Y, Posner MR. Swallowing dysfunction after chemoradiation for advanced squamous cell carcinoma of the head and neck. Head Neck. 2004; 26:365–372. PMID: 15054740.
Article19. Murphy BA. Clinical and economic consequences of mucositis induced by chemotherapy and/or radiation therapy. J Support Oncol. 2007; 5(9 Suppl 4):13–21.20. Terk AR, Leder SB, Burrell MI. Hyoid bone and laryngeal movement dependent upon presence of a tracheotomy tube. Dysphagia. 2007; 22:89–93. PMID: 17287926.
Article21. Mullen R, Schooling T. The National Outcomes Measurement System for pediatric speech-language pathology. Lang Speech Hear Serv Sch. 2010; 41:44–60. PMID: 19833827.
Article22. Hutcheson KA, Lewin JS, Barringer DA, Lisec A, Gunn GB, Moore MW, et al. Late dysphagia after radiotherapy-based treatment of head and neck cancer. Cancer. 2012; 118:5793–5799. PMID: 23640737.
Article23. Nguyen NP, Sallah S. Combined chemotherapy and radiation in the treatment of locally advanced head and neck cancers. In Vivo. 2000; 14:35–39. PMID: 10757059.24. Logemann JA, Rademaker AW, Pauloski BR, Lazarus CL, Mittal BB, Brockstein B, et al. Site of disease and treatment protocol as correlates of swallowing function in patients with head and neck cancer treated with chemoradiation. Head Neck. 2006; 28:64–73. PMID: 16302193.
Article25. Sonis ST, Elting LS, Keefe D, Peterson DE, Schubert M, Hauer-Jensen M, et al. Perspectives on cancer therapy-induced mucosal injury: pathogenesis, measurement, epidemiology, and consequences for patients. Cancer. 2004; 100(9 Suppl):1995–2025. PMID: 15108222.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Organ Preservation for the Management of Locally Advanced Head and Neck Cancer
- The Usefulness of Flexible Endoscopic Evaluation of Swallowing in Head and Neck Cancer Patients
- Delayed Onset Severe Dysphagia Due to Radiation Neuropathy -A Case Report-
- Swallow Syncope following Chemoradiotherapy in a Patient with Lung Cancer
- Peri-Treatment Evaluation of Swallowing in Head and Neck Cancer Patients