Anesth Pain Med.
2017 Jan;12(1):15-22. 10.17085/apm.2017.12.1.15.
Does acute normovolemic hemodilution affect intraoperative value of serum-creatinine concentration in patients undergoing cardiac surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. taeyop@gmail.com
- 2Department of Anesthesiology and Pain Medicine, Korea University Guro Hospital, Seoul, Korea.
- 3Department of Business, Sungkyunkwan University, Seoul, Korea.
- 4Department of Anesthesiology and Pain Medicine, The Catholic University of Korea, College of Medicine, Seoul, Korea.
- KMID: 2369660
- DOI: http://doi.org/10.17085/apm.2017.12.1.15
Abstract
- BACKGROUND
The possible impact of hemodilution during acute normovolemic hemodilution (ANH) using hydroxyethyl starch (HES) on intraoperative serum concentration of creatinine (s-Cr) has not been well investigated.
METHODS
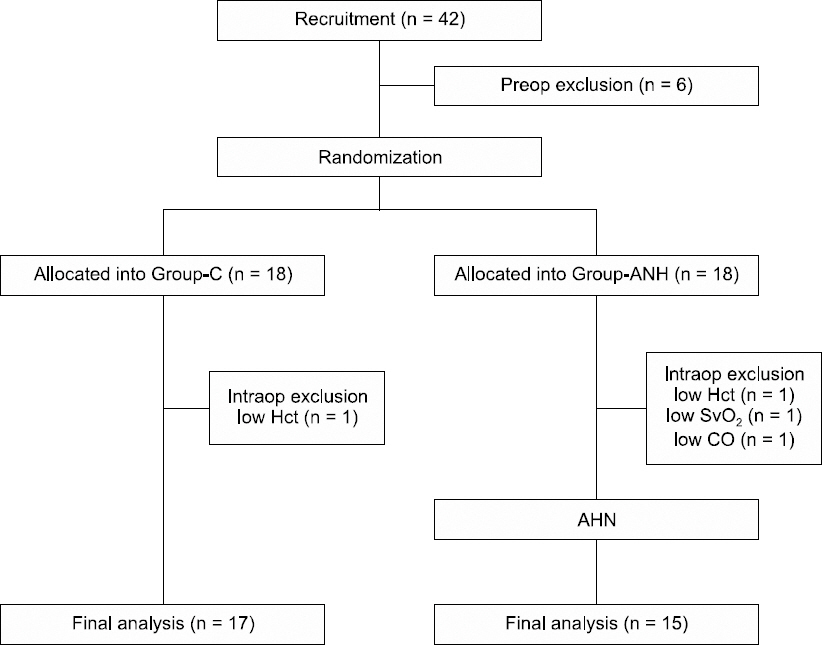
Patients undergoing cardiac surgery were randomly allocated into Group-ANH (n = 15) or Group-C (control; n = 17). In Group-ANH, 5 ml/kg whole blood was collected, and they were administered 5 ml/kg of HES 130/0.4 after anesthesia induction and before initiating cardiopulmonary bypass (CPB). In both groups, moderate hypothermic CPB was initiated using 1,600-1,800 ml of bloodless priming solution. The changes of s-Cr, blood urea nitrogen, hematocrit (Hct), electrolytes, and osmolality were determined before ANH administration (T1), after administering ANH 5 ml/kg (T2), 30 and 60 s after the initiation of CPB (T3, T4), and at the end of surgery (T5).
RESULTS
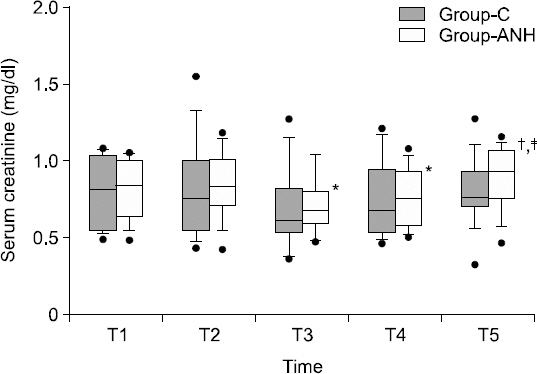
In Group-ANH, the s-Cr values at T2 (median [IQR25-75%], 0.83 [0.71-1.00] mg/dl) were not significantly different compared to those at T1 (0.84 [0.64-1.00] mg/dl), while those at T3 and T4 (0.68 [0.61-0.80] and 0.76 [0.59-0.92] mg/dl, respectively) were significantly lower than those at T2 (0.83 [0.71-1.00] mg/dl, P < 0.001). Hct at T3, T4 and T5 were significantly lower than those of T1 in both groups, and those at T2 and T4 of Group-ANH were significantly lower than those of Group-C (P < 0.001). There was no significant inter-group difference in all other parameters.
CONCLUSIONS
Intraoperative s-Cr was not affected by the administration of ANH 5 ml/kg, although it reduced transiently at the beginning of CPB. Further study is needed to determine the clinical relevancy of our results.
MeSH Terms
Figure
Reference
-
1. Bennett SR. Perioperative autologous blood transfusion in elective total hip prosthesis operations. Ann R Coll Surg Engl. 1994; 76:95–8. DOI: 10.1097/00132586-199412000-00057.2. Bennett J, Haynes S, Torella F, Grainger H, McCollum C. Acute normovolemic hemodilution in moderate blood loss surgery: a randomized controlled trial. Transfusion. 2006; 46:1097–103. DOI: 10.1111/j.1537-2995.2006.00857.x. PMID: 16836555.3. Berg KS, Stenseth R, Wahba A, Pleym H, Videm V. How can we best predict acute kidney injury following cardiac surgery?: a prospective observational study. Eur J Anaesthesiol. 2013; 30:704–12. DOI: 10.1097/EJA.0b013e328365ae64. PMID: 24067536.4. Mangano CM, Diamondstone LS, Ramsay JG, Aggarwal A, Herskowitz A, Mangano DT. Renal dysfunction after myocardial revascularization: risk factors, adverse outcomes, and hospital resource utilization. The Multicenter Study of Perioperative Ischemia Research Group. Ann Intern Med. 1998; 128:194–203. DOI: 10.7326/0003-4819-128-3-199802010-00005. PMID: 9454527.5. Jung HS, Kim CS, Kim TY. The relationship of serum creatinine and cardiac troponin I after off-pump coronary artery bypass graft surgery. Anesth Pain Med. 2009; 4:124–8.6. Lee EH. Acute kidney injury in cardiac surgery. Anesth Pain Med. 2016; 11:225–35. DOI: 10.17085/apm.2016.11.3.225.7. Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007; 71:1028–35. DOI: 10.1038/sj.ki.5002231. PMID: 17396113.8. Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004; 8:R204–12. DOI: 10.1186/cc2671. DOI: 10.1186/cc2872. PMID: 15312219. PMCID: PMC522841.9. Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007; 11:R31. DOI: 10.1186/cc5713. PMID: 17331245. PMCID: PMC2206446.10. Parolari A, Pesce LL, Pacini D, Mazzanti V, Salis S, Sciacovelli C, et al. Risk factors for perioperative acute kidney injury after adult cardiac surgery: role of perioperative management. Ann Thorac Surg. 2012; 93:584–91. DOI: 10.1016/j.athoracsur.2011.09.073. PMID: 22269725.11. Kumar AB, Suneja M, Bayman EO, Weide GD, Tarasi M. Association between postoperative acute kidney injury and duration of cardiopulmonary bypass: a meta-analysis. J Cardiothorac Vasc Anesth. 2012; 26:64–9. DOI: 10.1053/j.jvca.2011.07.007. PMID: 21924633.12. Rosner MH, Okusa MD. Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol. 2006; 1:19–32. DOI: 10.2215/CJN.00240605. PMID: 17699187.13. Bojan M, Lopez-Lopez V, Pouard P, Falissard B, Journois D. Limitations of early serum creatinine variations for the assessment of kidney injury in neonates and infants with cardiac surgery. PLoS One. 2013; 8:e79308. DOI: 10.1371/journal.pone.0079308. PMID: 24244476. PMCID: PMC3823616.14. Waikar SS, Liu KD, Chertow GM. Diagnosis, epidemiology and outcomes of acute kidney injury. Clin J Am Soc Nephrol. 2008; 3:844–61. DOI: 10.2215/CJN.05191107. PMID: 18337550.15. Lassnigg A, Schmid ER, Hiesmayr M, Falk C, Druml W, Bauer P, et al. Impact of minimal increases in serum creatinine on outcome in patients after cardiothoracic surgery: do we have to revise current definitions of acute renal failure? Crit Care Med. 2008; 36:1129–37. DOI: 10.1097/CCM.0b013e318169181a. PMID: 18379238.16. Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol. 2004; 15:1597–605. DOI: 10.1097/01.ASN.0000130340.93930.DD. PMID: 15153571.17. Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005; 16:3365–70. DOI: 10.1681/ASN.2004090740. PMID: 16177006.18. Swaminathan M, Phillips-Bute BG, Conlon PJ, Smith PK, Newman MF, Stafford-Smith M. The association of lowest hematocrit during cardiopulmonary bypass with acute renal injury after coronary artery bypass surgery. Ann Thorac Surg. 2003; 76:784–91. DOI: 10.1016/S0003-4975(03)00558-7.19. Gross JB. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983; 58:277–80. DOI: 10.1097/00000542-198303000-00016. PMID: 6829965.20. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976; 16:31–41. DOI: 10.1159/000180580.21. Edwards KD, Whyte HM. Plasma creatinine level and creatinine clearance as tests of renal function. Australas Ann Med. 1959; 8:218–24. PMID: 13819423.22. Stafford-Smith M. Perioperative renal dysfunction: Implications and strategies for protection. Perioperative Organ Protection. Newman MF, editor. Richmond, Society of Cardiovascular Anesthesiologists. 2003; 89–124.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraoperative Normovolemic Hemodilution in Patients Undergonig Posterolateral Spinal Fusion: Safety and Efficacy
- Acute normovolemic hemodilution for a patient with secondary polycythemia undergoing aortic valve replacement due to severe aortic stenosis - A case report -
- An Experiment on Intraoperative Autotransgusion and Normovolemic Hemodilution with hartmann`s Solution and Rheomacrodex
- Effect of Acute Normovolemic Hemodilution on Homologous Blood Saving during Off-Pump CABG
- An Experimental Study of Acute Normovolemic Hemodilution on Cardiopulmonary Vsscular System in Autotransfusions