Ann Pediatr Endocrinol Metab.
2016 Dec;21(4):199-205. 10.6065/apem.2016.21.4.199.
Leptin and adiponectin levels in girls with central precocious puberty before and during GnRH agonist treatment
- Affiliations
-
- 1Department of Pediatrics, Chungnam National University School of Medicine, Daejeon, Korea. damus@cnuh.or.kr
- KMID: 2366810
- DOI: http://doi.org/10.6065/apem.2016.21.4.199
Abstract
- PURPOSE
The effects of gonadotropin-releasing hormone agonist (GnRHa) treatment on the energy metabolism in girls with central precocious puberty (CPP) are controversial. We focused the changes and related factors of serum levels of leptin and adiponectin in girls with CPP before and during GnRHa treatment.
METHODS
Thirty girls with idiopathic CPP were enrolled in the study. Their auxological data and fasting blood were collected at the baseline and after six months of GnRHa treatment.
RESULTS
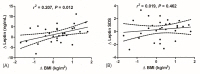
After treatment, height (P<0.001), weight (P<0.001), and serum leptin levels (P=0.033) were significantly increased, whereas body mass index (BMI), homeostasis model of assessment-insulin resistance, serum adiponectin levels, and adiponectin/leptin ratio exhibited no significant changes. A Pearson correlation analysis showed that height, weight, BMI, and their standard deviation scores (SDSs), but not basal LH, FSH, and estradiol, were significantly correlated with serum leptin levels before and after GnRHa treatment. After a multiple linear regression analysis, only BMI was associated with serum leptin levels. Moreover, leptin SDSs adjusted for BMI were not significantly different before and after GnRHa. The Δ leptin levels (r2=0.207, P=0.012), but not with Δ leptin SDS (r2=0.019, P=0.556), during GnRHa treatment were positively correlated with Δ BMI.
CONCLUSION
These results suggest that GnRHa treatment in girls with CPP does not affect serum levels of leptin and adiponectin and insulin resistance. Serum leptin levels were depend on the changes in BMI during GnRHa treatment.
Figure
Reference
-
1. Fuqua JS. Treatment and outcomes of precocious puberty: an update. J Clin Endocrinol Metab. 2013; 98:2198–2207. PMID: 23515450.
Article2. DiVall SA, Radovick S. Endocrinology of female puberty. Curr Opin Endocrinol Diabetes Obes. 2009; 16:1–4. PMID: 19115519.
Article3. Kaplowitz PB, Slora EJ, Wasserman RC, Pedlow SE, Herman-Giddens ME. Earlier onset of puberty in girls: relation to increased body mass index and race. Pediatrics. 2001; 108:347–353. PMID: 11483799.
Article4. Pasquino AM, Pucarelli I, Accardo F, Demiraj V, Segni M, Di Nardo R. Long-term observation of 87 girls with idiopathic central precocious puberty treated with gonadotropin-releasing hormone analogs: impact on adult height, body mass index, bone mineral content, and reproductive function. J Clin Endocrinol Metab. 2008; 93:190–195. PMID: 17940112.
Article5. Taşcilar ME, Bilir P, Akinci A, Köse K, Akçora D, Inceoğlu D, et al. The effect of gonadotropin-releasing hormone analog treatment (leuprolide) on body fat distribution in idiopathic central precocious puberty. Turk J Pediatr. 2011; 53:27–33. PMID: 21534336.6. Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH, Zhang Y, et al. Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med. 1995; 1:1155–1161. PMID: 7584987.
Article7. Lee B, Shao J. Adiponectin and energy homeostasis. Rev Endocr Metab Disord. 2014; 15:149–156. PMID: 24170312.
Article8. Kubota N, Yano W, Kubota T, Yamauchi T, Itoh S, Kumagai H, et al. Adiponectin stimulates AMP-activated protein kinase in the hypothalamus and increases food intake. Cell Metab. 2007; 6:55–68. PMID: 17618856.
Article9. Bohlen TM, Silveira MA, Zampieri TT, Frazão R, Donato J Jr. Fatness rather than leptin sensitivity determines the timing of puberty in female mice. Mol Cell Endocrinol. 2016; 423:11–21. PMID: 26762764.
Article10. Sanchez-Garrido MA, Tena-Sempere M. Metabolic control of puberty: roles of leptin and kisspeptins. Horm Behav. 2013; 64:187–194. PMID: 23998663.
Article11. Abacı A, Çatlı G, Anık A, Küme T, Çalan ÖG, Dündar BN, et al. Significance of serum neurokinin B and kisspeptin levels in the differential diagnosis of premature thelarche and idiopathic central precocious puberty. Peptides. 2015; 64:29–33. PMID: 25572302.
Article12. Korea Centers for Disease Control and Prevention, Division of Chronic Disease Surveillance, Committee for the Development of Growth Standard for Korean Children and Adolescents. Korean Pediatric Society, Committee for School Health and Public Health Statistics. 2007 Korean children and adolescents growth standard (commentary for the development of 2007 growth chart. Cheongju: Korea Centers for Disease Control and Prevention, Division of Chronic Disease Surveillance;2007.13. Blum WF, Englaro P, Hanitsch S, Juul A, Hertel NT, Müller J, et al. Plasma leptin levels in healthy children and adolescents: dependence on body mass index, body fat mass, gender, pubertal stage, and testosterone. J Clin Endocrinol Metab. 1997; 82:2904–2910. PMID: 9284717.
Article14. Lee JM, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH, Lumeng JC. Weight status in young girls and the onset of puberty. Pediatrics. 2007; 119:e624–e630. PMID: 17332182.
Article15. Castellano JM, Bentsen AH, Sánchez-Garrido MA, Ruiz-Pino F, Romero M, Garcia-Galiano D, et al. Early metabolic programming of puberty onset: impact of changes in postnatal feeding and rearing conditions on the timing of puberty and development of the hypothalamic kisspeptin system. Endocrinology. 2011; 152:3396–3408. PMID: 21712362.
Article16. Cheung CC, Thornton JE, Nurani SD, Clifton DK, Steiner RA. A reassessment of leptin's role in triggering the onset of puberty in the rat and mouse. Neuroendocrinology. 2001; 74:12–21. PMID: 11435754.
Article17. Tommaselli GA, Di Carlo C, Bifulco G, Di Spiezio, Pellicano M, Nappi C. Serum leptin levels in patients with premenstrual syndrome treated with GnRH analogues alone and in association with tibolone. Clin Endocrinol (Oxf). 2003; 59:716–722. PMID: 14974912.
Article18. Su PH, Wang SL, Lin CY, Chen JY, Changlai CP, Jian SH, et al. Leptin changes in Taiwanese girls with central precocious puberty before and during the GnRH agonist treatment. Acta Paediatr Taiwan. 2005; 46:278–283. PMID: 16640001.19. Verrotti A, Basciani F, Trotta D, De Simone M, Morgese G, Chiarelli F. Serum leptin levels in girls with precocious puberty. Diabetes Nutr Metab. 2003; 16:125–129. PMID: 12846452.20. Mølgaard C, Michaelsen KF. Changes in body composition during growth in healthy school-age children. Appl Radiat Isot. 1998; 49:577–579. PMID: 9569546.
Article21. Davison KK, Susman EJ, Birch LL. Percent body fat at age 5 predicts earlier pubertal development among girls at age 9. Pediatrics. 2003; 111(4 Pt 1):815–821. PMID: 12671118.
Article22. Boot AM, De Muinck, Pols HA, Krenning EP, Drop SL. Bone mineral density and body composition before and during treatment with gonadotropin-releasing hormone agonist in children with central precocious and early puberty. J Clin Endocrinol Metab. 1998; 83:370–373. PMID: 9467543.
Article23. Sørensen K, Andersson AM, Skakkebaek NE, Juul A. Serum sex hormone-binding globulin levels in healthy children and girls with precocious puberty before and during gonadotropin-releasing hormone agonist treatment. J Clin Endocrinol Metab. 2007; 92:3189–3196. PMID: 17519314.
Article24. Landgraf K, Rockstroh D, Wagner IV, Weise S, Tauscher R, Schwartze JT, et al. Evidence of early alterations in adipose tissue biology and function and its association with obesity-related inflammation and insulin resistance in children. Diabetes. 2015; 64:1249–1261. PMID: 25392242.
Article25. Sørensen K, Mouritsen A, Mogensen SS, Aksglaede L, Juul A. Insulin sensitivity and lipid profiles in girls with central precocious puberty before and during gonadal suppression. J Clin Endocrinol Metab. 2010; 95:3736–3744. PMID: 20484471.
Article26. Inoue M, Yano M, Yamakado M, Maehata E, Suzuki S. Relationship between the adiponectin-leptin ratio and parameters of insulin resistance in subjects without hyperglycemia. Metabolism. 2006; 55:1248–1254. PMID: 16919546.
Article27. Böttner A, Kratzsch J, Müller G, Kapellen TM, Blüher S, Keller E, et al. Gender differences of adiponectin levels develop during the progression of puberty and are related to serum androgen levels. J Clin Endocrinol Metab. 2004; 89:4053–4061. PMID: 15292348.
Article28. Itoh H, Kawano Y, Furukawa Y, Matsumoto H, Yuge A, Narahara H. The role of serum adiponectin levels in women with polycystic ovarian syndrome. Clin Exp Obstet Gynecol. 2013; 40:531–535. PMID: 24597249.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Treatment of Central Precocious Puberty
- Serum Anti-Müllerian Hormone Levels in Precocious Puberty Girls according to Stage of GnRH Agonist Treatment
- Prediction of 1 Year Growth in Girls with Precocious Puberty with GnRH Agonist Treatment by Measurement of Growth Velocity at 3 Months after Treatment
- Auxological Effects of Gonadotropin-releasing Hormone Agonist Treatment for Central Precocious Puberty
- The Effect of Gonadotropin Releasing Hormone Agonist and Growth Hormone on Predicted Adult Height in Girls with Precocious Puberty