Yonsei Med J.
2015 Jul;56(4):1122-1127. 10.3349/ymj.2015.56.4.1122.
Head Elevation in Spinal-Epidural Anesthesia Provides Improved Hemodynamics and Appropriate Sensory Block Height at Caesarean Section
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. emchoi96@hallym.or.kr
- 2Department of Obstetrics and Gynecology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- KMID: 2366356
- DOI: http://doi.org/10.3349/ymj.2015.56.4.1122
Abstract
- PURPOSE
We aimed to determine whether head elevation during combined spinal-epidural anesthesia (CSE) and Caesarean section provided improved hemodynamics and appropriate sensory block height.
MATERIALS AND METHODS
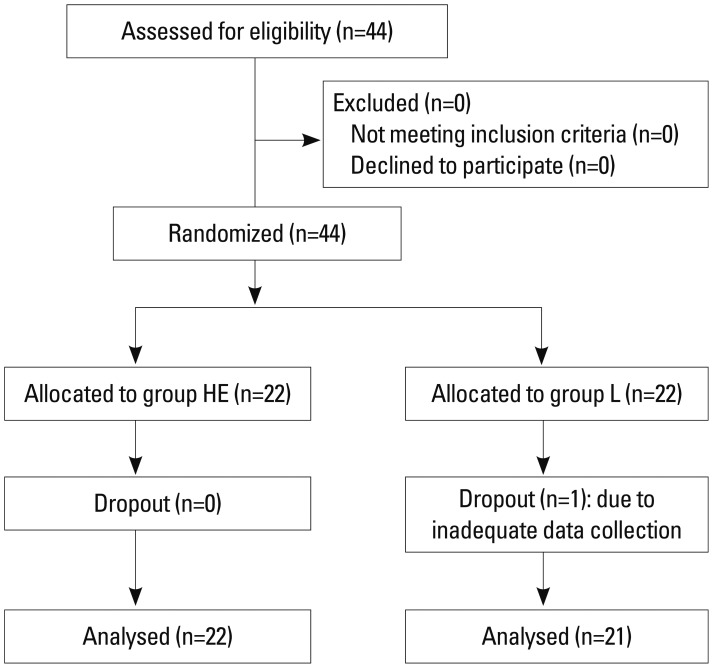
Forty-four parous women undergoing CSE for elective Caesarean section were randomly assigned to one of two groups: right lateral (group L) or right lateral and head elevated (group HE) position, for insertion of the block. Patients were positioned in the supine wedged position (group L) or the left lateral and head elevated position (group HE) until a block height of T5 to light touch was reached. Group HE was then turned to the supine wedged position with maintenance of head elevation until the end of surgery. Hemodynamics, including the incidence of hypotension, ephedrine dose required, and characteristics of the sensory blocks were analyzed.
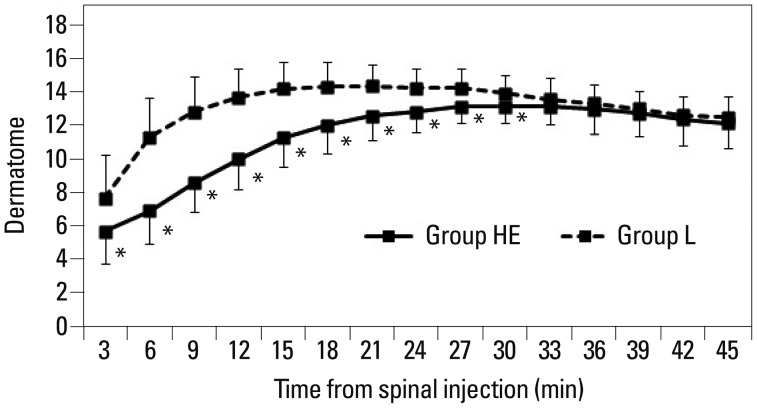
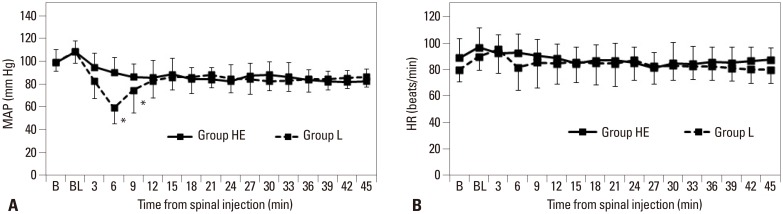
RESULTS
The incidence of hypotension (16 versus 7, p=0.0035) and the required dose of ephedrine [24 (0-40) versus 0 (0-20), p<0.0001] were greater in group L compared to group HE. In group L, the time to achieve maximal sensory block level (MSBL) was shorter (11.8+/-5.4 min versus 20.1+/-6.3 min, p<0.0001) and MSBL was also higher than in group HE [14 (T2) versus 12 (T4), p=0.0015].
CONCLUSION
Head elevation during CSE and Caesarean section is superior to positioning without head elevation in the lateral to supine position, as it is associated with a more gradual onset, appropriate block height, and improved hemodynamics.
MeSH Terms
Figure
Reference
-
1. Phelan DM, MacEvilly M. A comparison of hyper- and isobaric solutions of bupivacaine for subarachnoid block. Anaesth Intensive Care. 1984; 12:101–107. PMID: 6476342.
Article2. Carrie LE, O'Sullivan G. Subarachnoid bupivacaine 0.5% for caesarean section. Eur J Anaesthesiol. 1984; 1:275–283. PMID: 6536516.3. Patel M, Samsoon G, Swami A, Morgan B. Posture and the spread of hyperbaric bupivacaine in parturients using the combined spinal epidural technique. Can J Anaesth. 1993; 40:943–946. PMID: 8222034.
Article4. James KS, McGrady E, Patrick A. Combined spinal-extradural anaesthesia for preterm and term caesarean section: is there a difference in local anaesthetic requirements? Br J Anaesth. 1997; 78:498–501. PMID: 9175961.
Article5. Carrie LE. Spinal and/or epidural blockade for Caesarean section. In : Reynolds F, editor. Epidural and spinal blockade in obstetrics. London: Bailliere-Tindall;1990. p. 139–150.6. Yun EM, Marx GF, Santos AC. The effects of maternal position during induction of combined spinal-epidural anesthesia for cesarean delivery. Anesth Analg. 1998; 87:614–618. PMID: 9728840.
Article7. Stoneham MD, Eldridge J, Popat M, Russell R. Oxford positioning technique improves haemodynamic stability and predictability of block height of spinal anaesthesia for elective caesarean section. Int J Obstet Anesth. 1999; 8:242–248. PMID: 15321118.
Article8. Russell R, Popat M, Richards E, Burry J. Combined spinal epidural anaesthesia for caesarean section: a randomised comparison of Oxford, lateral and sitting positions. Int J Obstet Anesth. 2002; 11:190–195. PMID: 15321547.
Article9. Rucklidge MW, Paech MJ, Yentis SM. A comparison of the lateral, Oxford and sitting positions for performing combined spinal-epidural anaesthesia for elective Caesarean section. Anaesthesia. 2005; 60:535–540. PMID: 15918823.
Article10. Lewis NL, Ritchie EL, Downer JP, Nel MR. Left lateral vs. supine, wedged position for development of block after combined spinal-epidural anaesthesia for Caesarean section. Anaesthesia. 2004; 59:894–898. PMID: 15310354.
Article11. Gizzo S, Noventa M, Fagherazzi S, Lamparelli L, Ancona E, Di Gangi S, et al. Update on best available options in obstetrics anaesthesia: perinatal outcomes, side effects and maternal satisfaction. Fifteen years systematic literature review. Arch Gynecol Obstet. 2014; 290:21–34. PMID: 24659334.
Article12. Craig JR, Swales H. Oxford positioning technique vs. sitting-to-wedged supine position for caesarean section under spinal anaesthesia. Int J Obstet Anesth. 2001; 10:151. PMID: 15321640.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Epidural "Top-up" on Spinal Block during Combined Spinal Epidural Anesthesia for Cesarean Section
- Comparison of Intrathecal Isobaric and Hyperbaric Bupivacaine during Combined Spinal Epidural Anesthesia for Cesarean Section
- Management of hypotension after spinal anesthesia administered for caesarean section
- Prevention of Nausea and Vomiting during Spinal or Epidural Anesthesia for Cesarean Section - The Efficacy of Metoclopramide and Droperidol -
- How Changing Lumbar Epidural Pressure Affects the Distribution of Local Anesthetics and the Level of Spinal Anesthesia