Tuberc Respir Dis.
2016 Oct;79(4):302-306. 10.4046/trd.2016.79.4.302.
Pulmonary Leukocytoclastic Vasculitis as an Initial Presentation of Myelodysplastic Syndrome
- Affiliations
-
- 1Department of Internal Medicine, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea. gusrud9@paik.ac.kr
- 2Department of Pathology, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea.
- KMID: 2365323
- DOI: http://doi.org/10.4046/trd.2016.79.4.302
Abstract
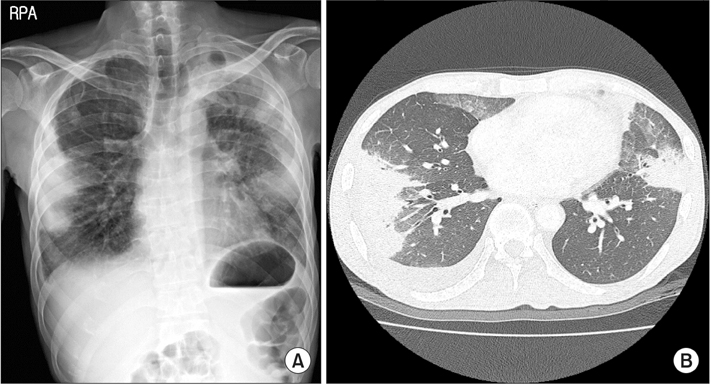
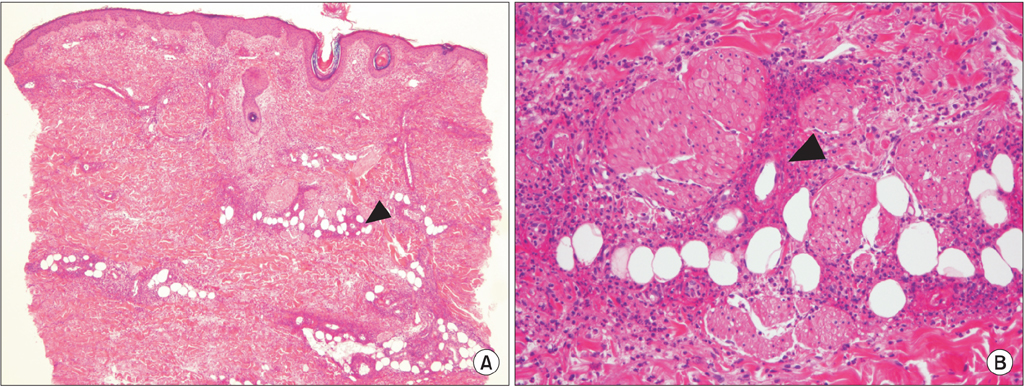
- Systemic vasculitis involving the lung is a rare manifestation of myelodysplastic syndrome (MDS), and secondary vasculitis is considered to have poor prognosis. A 44-year-old man presented with fever and dyspnea of 1 month duration. A chest radiograph revealed bilateral multiple wedge shaped consolidations. In addition, the results of a percutaneous needle biopsy for non-resolving pneumonia were compatible with pulmonary vasculitis. Bone marrow biopsy was performed due to the persistence of unexplained anemia and the patient was diagnosed with MDS. We reported a case of secondary vasculitis presenting as non-resolving pneumonia, later diagnosed as paraneoplastic syndrome of undiagnosed MDS. The cytopenia and vasculitis improved after a short course of glucocorticoid treatment, and there was no recurrence despite the progression of underlying MDS.
Keyword
MeSH Terms
Figure
Reference
-
1. Dreyfus B, Vernant JP, Wechsler J, Imbert M, De Prost Y, Reyes F, et al. Refractory anaemia with an excess of myeloblasts and cutaneous vasculitis (author's transl). Nouv Rev Fr Hematol. 1981; 23:115–121.2. Enright H, Jacob HS, Vercellotti G, Howe R, Belzer M, Miller W. Paraneoplastic autoimmune phenomena in patients with myelodysplastic syndromes: response to immunosuppressive therapy. Br J Haematol. 1995; 91:403–408.3. Giannouli S, Voulgarelis M, Zintzaras E, Tzioufas AG, Moutsopoulos HM. Autoimmune phenomena in myelodysplastic syndromes: a 4-yr prospective study. Rheumatology (Oxford). 2004; 43:626–632.4. Belizna C, Subra JF, Henrion D, Ghali A, Renier G, Royer M, et al. Prognosis of vasculitis associated myelodysplasia. Autoimmun Rev. 2013; 12:943–946.5. de Hollanda A, Beucher A, Henrion D, Ghali A, Lavigne C, Levesque H, et al. Systemic and immune manifestations in myelodysplasia: a multicenter retrospective study. Arthritis Care Res (Hoboken). 2011; 63:1188–1194.6. Enright H, Miller W. Autoimmune phenomena in patients with myelodysplastic syndromes. Leuk Lymphoma. 1997; 24:483–489.7. van Rijn RS, Wittebol S, Graafland AD, Kramer MH. Immunologic phenomena as the first sign of myelodysplastic syndrome. Ned Tijdschr Geneeskd. 2001; 145:1529–1533.8. Al Ustwani O, Ford LA, Sait SJ, Block AM, Barcos M, Vigil CE, et al. Myelodysplastic syndromes and autoimmune diseases: case series and review of literature. Leuk Res. 2013; 37:894–899.9. Saif MW, Hopkins JL, Gore SD. Autoimmune phenomena in patients with myelodysplastic syndromes and chronic myelomonocytic leukemia. Leuk Lymphoma. 2002; 43:2083–2092.10. Braun T, Fenaux P. Myelodysplastic syndromes (MDS) and autoimmune disorders (AD): cause or consequence? Best Pract Res Clin Haematol. 2013; 26:327–336.11. Ma X, Does M, Raza A, Mayne ST. Myelodysplastic syndromes: incidence and survival in the United States. Cancer. 2007; 109:1536–1542.12. Jin J, Yu M, Hu C, Ye L, Xie L, Chen F, et al. Alcohol consumption and risk of myelodysplastic syndromes: a meta-analysis of epidemiological studies. Mol Clin Oncol. 2014; 2:1115–1120.13. Du Y, Fryzek J, Sekeres MA, Taioli E. Smoking and alcohol intake as risk factors for myelodysplastic syndromes (MDS). Leuk Res. 2010; 34:1–5.14. Kiladjian JJ, Visentin G, Viey E, Chevret S, Eclache V, Stirnemann J, et al. Activation of cytotoxic T-cell receptor gammadelta T lymphocytes in response to specific stimulation in myelodysplastic syndromes. Haematologica. 2008; 93:381–389.15. Kordasti SY, Ingram W, Hayden J, Darling D, Barber L, Afzali B, et al. CD4+CD25high Foxp3+ regulatory T cells in myelodysplastic syndrome (MDS). Blood. 2007; 110:847–850.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Leukocytoclastic Vasculitis Associated with Pulmonary Tuberculosis
- A Case of Leukocytoclastic Vasculitis Associated with Antiphospholipid Antibody Syndorme
- A Case of Leukocytoclastic Vasculitis Following COVID-19 Vaccination
- Warfarin-induced Leukocytoclastic Vasculitis
- A Case of Leukocytoclastic Vasculitis Induced by Leuprolide Acetate