J Korean Soc Radiol.
2017 Jan;76(1):67-72. 10.3348/jksr.2017.76.1.67.
MRI Findings of Spinal Angiomyolipoma: A Case Report and Literature Review
- Affiliations
-
- 1Department of Radiology, Yonsei University Wonju College of Medicine, Wonju Severance Christian Hospital, Wonju, Korea. kim0328@yonsei.ac.kr
- 2Department of Radiology, Kangwon National University Hospital, Kangwon National University School of Medicine, Chuncheon, Korea.
- 3Department of Pathology, Yonsei University Wonju College of Medicine, Wonju Severance Christian Hospital, Wonju, Korea.
- KMID: 2365054
- DOI: http://doi.org/10.3348/jksr.2017.76.1.67
Abstract
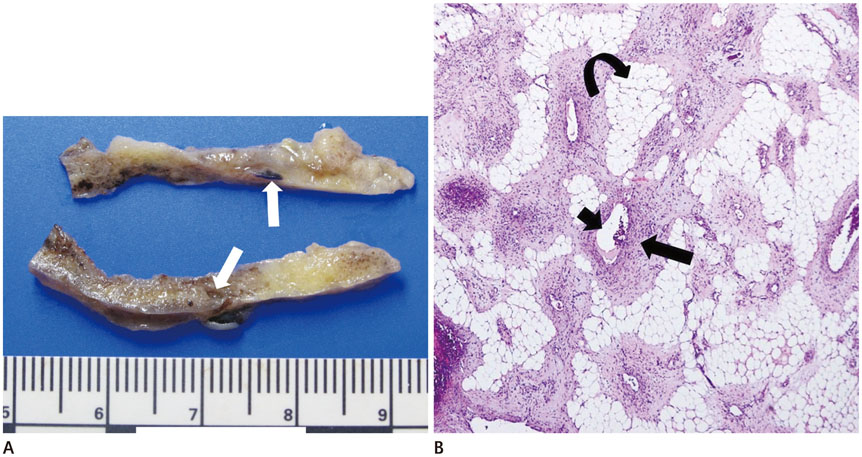
- Spinal angiomyolipoma (AML) is a rare disease. It is often reviewed with spinal angiolipoma. Both are composed of vascular and mature adipose elements. However, only AML contains broader array of mesenchymal component. They are accounting for 0.14% to 1.2% of spinal tumors. They appear as fat containing hypervascular tumor located at epidural space of thoracic spine. Spinal AML is more frequently infiltrative and ofted occurs more ventrally than angiolipoma. Previous studies have employed conventional radiograph, myelogram, and CT scan for spinal AML studies. Recently, MRI has been used for spinal AML in a few studies. Here, we describe a case of typical thoracic spinal AML with a review of its MRI findings and other differential diagnosis for epidural spinal mass with similar characteristics.
MeSH Terms
Figure
Reference
-
1. von Hanwehr R, Apuzzo ML, Ahmadi J, Chandrasoma P. Thoracic spinal angiomyolipoma: case report and literature review. Neurosurgery. 1985; 16:406–411.2. Provenzale JM, McLendon RE. Spinal angiolipomas: MR features. AJNR Am J Neuroradiol. 1996; 17:713–719.3. Preul MC, Leblanc R, Tampieri D, Robitaille Y, Pokrupa R. Spinal angiolipomas. Report of three cases. J Neurosurg. 1993; 78:280–286.4. Sakaida H, Waga S, Kojima T, Kubo Y, Matsubara T, Yamamoto J. Thoracic spinal angiomyolipoma with extracanal extension to the thoracic cavity. A case report. Spine (Phila Pa 1976). 1998; 23:391–394.5. Goldblum JR, Weiss SW, Folpe AL. Enzinger and Weiss's soft tissue tumors. 6th ed. Philadelphia: Elsevier Saunders;2013. p. 897–899.6. Pearson J, Stellar S, Feigin I. Angiomyolipoma: long-term cure following radical approach to malignant-appearing benign intraspinal tumor. Report of three cases. J Neurosurg. 1970; 33:466–470.7. Hu S, Hu CH, Hu XY, Wang XM, Dai H, Fang XM, et al. MRI features of spinal epidural angiolipomas. Korean J Radiol. 2013; 14:810–817.8. Geers C, Lecouvet FE, Behets C, Malghem J, Cosnard G, Lengelé BG. Polygonal deformation of the dural sac in lumbar epidural lipomatosis: anatomic explanation by the presence of meningovertebral ligaments. AJNR Am J Neuroradiol. 2003; 24:1276–1282.9. Lee JW, Cho EY, Hong SH, Chung HW, Kim JH, Chang KH, et al. Spinal epidural hemangiomas: various types of MR imaging features with histopathologic correlation. AJNR Am J Neuroradiol. 2007; 28:1242–1248.