J Breast Cancer.
2016 Dec;19(4):417-422. 10.4048/jbc.2016.19.4.417.
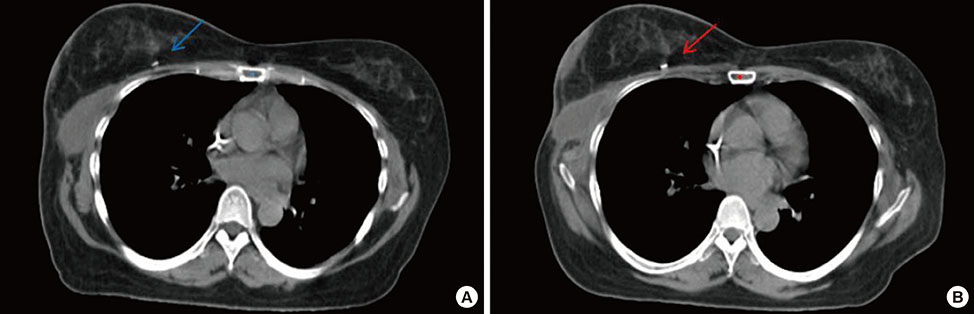
Displacement of Surgical Clips during Postoperative Radiotherapy in Breast Cancer Patients Who Received Breast-Conserving Surgery
- Affiliations
-
- 1Department of Radiation Oncology, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea. koppul@catholic.ac.kr
- 2Department of Surgery, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea.
- KMID: 2362928
- DOI: http://doi.org/10.4048/jbc.2016.19.4.417
Abstract
- PURPOSE
Surgical clips are used as a target for postoperative breast radiotherapy, and displacement of surgical clips would result in inaccurate delivery of radiation. We investigated the displacement range of surgical clips in the breast during postoperative radiotherapy following breast-conserving surgery.
METHODS
A total of 178 patients who received breast-conserving surgery and postoperative radiation of 59.4 Gy in 33 fractions to the involved breast for 6.5 weeks were included. Surgical clips were used to mark the lumpectomy cavity during breast-conserving surgery. Patients undertook planning computed tomography (CT) scan for whole breast irradiation. Five weeks after beginning radiation, when the irradiation dose was 45 Gy, planning CT scan was performed again for a boost radiotherapy plan in all patients. The surgical clips were defined in both CT images and compared in lateromedial (X), anteroposterior (Y), superoinferior (Z), and three-dimensional directions.
RESULTS
The 90th percentile of displacement of surgical clips was 5.31 mm (range, 0.0-22.2 mm) in the lateromedial direction, 7.1 mm (range, 0.0-14.2 mm) in the anteroposterior direction, and 6.0 mm (range, 0.0-10.0 mm) in the superoinferior direction. The 90th percentile of three-dimensional displacement distance was 9.8 mm (range, 0.0-28.2 mm). On the multivariate analysis, seroma ≥15 mL was the only independent factor associated with the displacement of surgical clips. In patients with seroma ≥15 mL, the 90th percentile of displacement of surgical clips was 15.1 mm in the lateromedial direction, 12.7 mm in the anteroposterior direction, 10.0 mm in the superoinferior direction, and 21.8 mm in the three-dimensional distance.
CONCLUSION
A target volume expansion of 10 mm from surgical clips may be sufficient to compensate for the displacement of clips during postoperative radiotherapy after breast-conserving surgery. For patients who had a seroma, a replanning CT scan for a boost radiation should be considered to ensure exact postoperative radiotherapy in breast cancer.
MeSH Terms
Figure
Cited by 1 articles
-
Displacement of Surgical Clips in Patients with Human Acellular Dermal Matrix in the Excision Cavity during Whole Breast Irradiation Following Breast-Conserving Surgery
Wonguen Jung, Kyubo Kim, Nam Sun Paik
Cancer Res Treat. 2020;52(2):388-395. doi: 10.4143/crt.2019.213.
Reference
-
1. Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002; 347:1227–1232.
Article2. Blichert-Toft M, Nielsen M, Düring M, Møller S, Rank F, Overgaard M, et al. Long-term results of breast conserving surgery vs. mastectomy for early stage invasive breast cancer: 20-year follow-up of the Danish randomized DBCG-82TM protocol. Acta Oncol. 2008; 47:672–681.
Article3. Litière S, Werutsky G, Fentiman IS, Rutgers E, Christiaens MR, Van Limbergen E, et al. Breast conserving therapy versus mastectomy for stage I-II breast cancer: 20 year follow-up of the EORTC 10801 phase 3 randomised trial. Lancet Oncol. 2012; 13:412–419.
Article4. Bartelink H, Horiot JC, Poortmans P, Struikmans H, Van den Bogaert W, Barillot I, et al. Recurrence rates after treatment of breast cancer with standard radiotherapy with or without additional radiation. N Engl J Med. 2001; 345:1378–1387.
Article5. Vrieling C, Collette L, Fourquet A, Hoogenraad WJ, Horiot JH, Jager JJ, et al. The influence of patient, tumor and treatment factors on the cosmetic results after breast-conserving therapy in the EORTC ‘boost vs. no boost’ trial. EORTC Radiotherapy and Breast Cancer Cooperative Groups. Radiother Oncol. 2000; 55:219–232.
Article6. Bartelink H, Horiot JC, Poortmans PM, Struikmans H, Van den Bogaert W, Fourquet A, et al. Impact of a higher radiation dose on local control and survival in breast-conserving therapy of early breast cancer: 10-year results of the randomized boost versus no boost EORTC 22881-10882 trial. J Clin Oncol. 2007; 25:3259–3265.
Article7. Romestaing P, Lehingue Y, Carrie C, Coquard R, Montbarbon X, Ardiet JM, et al. Role of a 10-Gy boost in the conservative treatment of early breast cancer: results of a randomized clinical trial in Lyon, France. J Clin Oncol. 1997; 15:963–968.
Article8. Hunter MA, McFall TA, Hehr KA. Breast-conserving surgery for primary breast cancer: necessity for surgical clips to define the tumor bed for radiation planning. Radiology. 1996; 200:281–282.
Article9. Harrington KJ, Harrison M, Bayle P, Evans K, Dunn PA, Lambert HE, et al. Surgical clips in planning the electron boost in breast cancer: a qualitative and quantitative evaluation. Int J Radiat Oncol Biol Phys. 1996; 34:579–584.
Article10. Bra size. Wikipedia;Accessed June 10th, 2016. https://en.wikipedia.org/wiki/Bra_size.11. Chung MJ, Lee GJ, Suh YJ, Lee HC, Lee SW, Jeong S, et al. Setup error and effectiveness of weekly image-guided radiation therapy of TomoDirect for early breast cancer. Cancer Res Treat. 2015; 47:774–780.
Article12. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002; 347:1233–1241.
Article13. Jin GH, Chen LX, Deng XW, Liu XW, Huang Y, Huang XB. A comparative dosimetric study for treating left-sided breast cancer for small breast size using five different radiotherapy techniques: conventional tangential field, filed-in-filed, tangential-IMRT, multi-beam IMRT and VMAT. Radiat Oncol. 2013; 8:89.
Article14. Mansouri S, Naim A, Glaria L, Marsiglia H. Dosimetric evaluation of 3-D conformal and intensity-modulated radiotherapy for breast cancer after conservative surgery. Asian Pac J Cancer Prev. 2014; 15:4727–4732.
Article15. Kim KS, Shin KH, Choi N, Lee SW. Hypofractionated whole breast irradiation: new standard in early breast cancer after breast-conserving surgery. Radiat Oncol J. 2016; 34:81–87.
Article16. Chung MJ, Suh YJ, Lee HC, Kang DG, Kim EJ, Kim SH, et al. Tumor bed volumetric changes during breast irradiation for the patients with breast cancer. Radiat Oncol J. 2013; 31:228–233.
Article17. Sharma R, Spierer M, Mutyala S, Thawani N, Cohen HW, Hong L, et al. Change in seroma volume during whole-breast radiation therapy. Int J Radiat Oncol Biol Phys. 2009; 75:89–93.
Article18. Oh KS, Kong FM, Griffith KA, Yanke B, Pierce LJ. Planning the breast tumor bed boost: changes in the excision cavity volume and surgical scar location after breast-conserving surgery and whole-breast irradiation. Int J Radiat Oncol Biol Phys. 2006; 66:680–686.
Article19. Petersen RP, Truong PT, Kader HA, Berthelet E, Lee JC, Hilts ML, et al. Target volume delineation for partial breast radiotherapy planning: clinical characteristics associated with low interobserver concordance. Int J Radiat Oncol Biol Phys. 2007; 69:41–48.
Article20. Lee SW, Hwang TK, Hong SH, Lee JY, Chung MJ, Jeong SM, et al. Outcome of postoperative radiotherapy following radical prostatectomy: a single institutional experience. Radiat Oncol J. 2014; 32:138–146.
Article21. Sung KC, Chang Y, Ryu S, Chung HK. High levels of serum vitamin D are associated with a decreased risk of metabolic diseases in both men and women, but an increased risk for coronary artery calcification in Korean men. Cardiovasc Diabetol. 2016; 15:112.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Displacement of Surgical Clips in Patients with Human AcellularDermal Matrix in the Excision Cavity during Whole Breast IrradiationFollowing Breast-Conserving Surgery
- Body Image and Physical suffering during Radiotherapy in Breast Cancer Patients Following Breast Conserving Operations
- Analysis of the Movement of Surgical Clips Implanted in Tumor Bed during Normal Breathing for Breast Cancer Patients
- Radiotherapy for Breast Cancer
- Oncoplastic Breast Surgery