Ann Surg Treat Res.
2016 Dec;91(6):327-331. 10.4174/astr.2016.91.6.327.
Primary hepatic malignant peripheral nerve sheath tumor successfully treated with combination therapy: a case report and literature review
- Affiliations
-
- 1Department of Surgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. bestoperator@schmc.ac.kr
- 2Department of Pathology, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- 3Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- KMID: 2360394
- DOI: http://doi.org/10.4174/astr.2016.91.6.327
Abstract
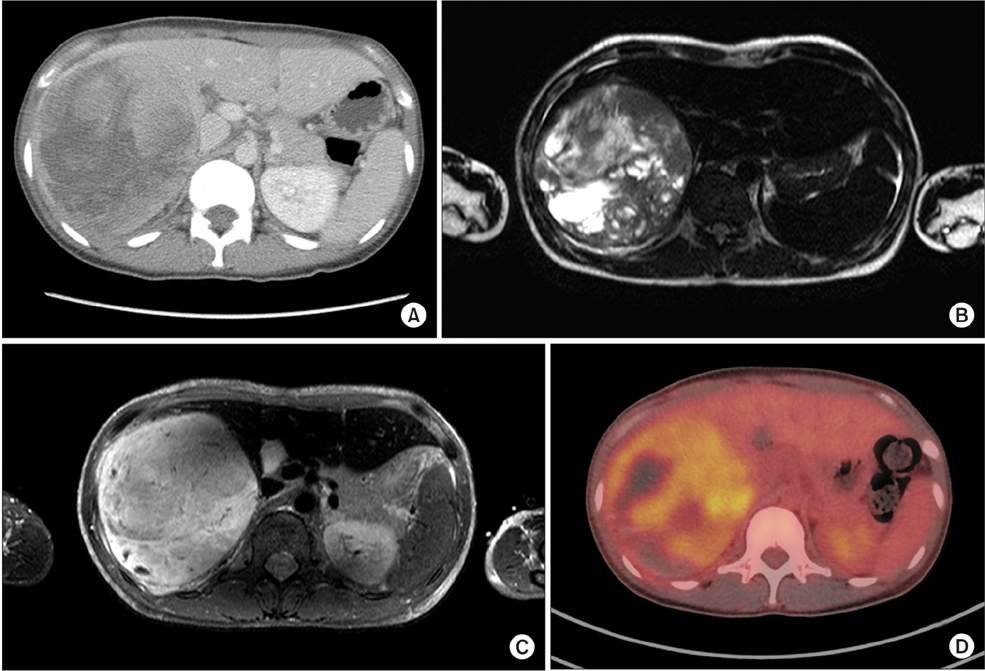
- Primary malignant peripheral nerve sheath tumor (MPNST) in a young female patient, not associated with neurofibromatosis type-I is extremely rare in the liver. A 33-year-old female was admitted with a right flank pain for a weak. The CT scan showed 12.5-cm-sized mass located at the right hepatic lobe. At laparotomy, about 20.0-cm-sized mass was on the right hepatic lobe with attachment to right diaphragmatic pleura. Right hepatic lobe and adherent part of diaphragmatic pleura were resected. On histology and immunohistochemistry, it was diagnosed MPNST. Adjuvant radiotherapy for the right diaphragmatic pleura and adjuvant chemotherapy with adriamycin, ifosfamide and cisplatin were sequentially performed. The prognosis of MPNST is generally poor and it is associated with a highly aggressive course of recurrence, metastases, and death. Our case is probably a first report about combination therapy.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Primary Hepatic Schwannoma
Youn I Choi, Yun Seob Kim, Ju Hyun Kim, Seong Hee Lee, Seong Gak Shin, Yun Soo Kim, Duck Joo Choi, Seung Joon Choi, Dong Hae Chung, Oh Sang Kwon
Korean J Gastroenterol. 2018;72(3):150-154. doi: 10.4166/kjg.2018.72.3.150.
Reference
-
1. Evans DG, Baser ME, McGaughran J, Sharif S, Howard E, Moran A. Malignant peripheral nerve sheath tumours in neurofibromatosis 1. J Med Genet. 2002; 39:311–314.2. Kakizaki S, Horiguchi N, Otsuka T, Takizawa D, Yamazaki Y, Sato K, et al. Malignant Peripheral Nerve Sheath Tumor of the Liver. Intern Med. 2016; 55:245–249.3. Kobori L, Nagy P, Mathe Z, Hartmann E, Doros A, Paku S, et al. Malignant peripheral nerve sheath tumor of the liver: a case report. Pathol Oncol Res. 2008; 14:329–332.4. Iddings DM, Wright BE, Bilchik A. A rare cause of primary hepatic neoplasm: malignant peripheral nerve sheath tumor in the age of modern liver surgery. Am Surg. 2008; 74:47–50.5. Ducatman BS, Scheithauer BW, Piepgras DG, Reiman HM, Ilstrup DM. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer. 1986; 57:2006–2021.6. Johnson MD, Glick AD, Davis BW. Immunohistochemical evaluation of Leu-7, myelin basic-protein, S100-protein, glialfibrillary acidic-protein, and LN3 immunoreactivity in nerve sheath tumors and sarcomas. Arch Pathol Lab Med. 1988; 112:155–160.7. Wanebo JE, Malik JM, VandenBerg SR, Wanebo HJ, Driesen N, Persing JA. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 28 cases. Cancer. 1993; 71:1247–1253.8. Kroep JR, Ouali M, Gelderblom H, Le Cesne A, Dekker TJ, Van Glabbeke M, et al. First-line chemotherapy for malignant peripheral nerve sheath tumor (MPNST) versus other histological soft tissue sarcoma subtypes and as a prognostic factor for MPNST: an EORTC soft tissue and bone sarcoma group study. Ann Oncol. 2011; 22:207–214.9. Carli M, Ferrari A, Mattke A, Zanetti I, Casanova M, Bisogno G, et al. Pediatric malignant peripheral nerve sheath tumor: the Italian and German soft tissue sarcoma cooperative group. J Clin Oncol. 2005; 23:8422–8430.10. Ferner RE, Gutmann DH. International consensus statement on malignant peripheral nerve sheath tumors in neurofibromatosis. Cancer Res. 2002; 62:1573–1577.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Malignant Peripheral Nerve Sheath Tumor of the Larynx
- Malignant Peripheral Nerve Sheath Tumor of the Cauda Equina in Type I Neurofibromatosis: Case Report
- Primary Paraspinal Malignant Peripheral Nerve Sheath Tumor
- A Case of Malignant Peripheral Nerve Sheath Tumor in Parapharyngeal Space
- A Case of Malignant Peripheral Nerve Sheath Tumor on Paranasal Sinus