J Korean Med Sci.
2016 Jan;31(1):125-130. 10.3346/jkms.2016.31.1.125.
Effects of Dexmedetomidine Infusion on the Recovery Profiles of Patients Undergoing Transurethral Resection
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, St. Vincent Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. ijangh@hanmail.net
- KMID: 2360002
- DOI: http://doi.org/10.3346/jkms.2016.31.1.125
Abstract
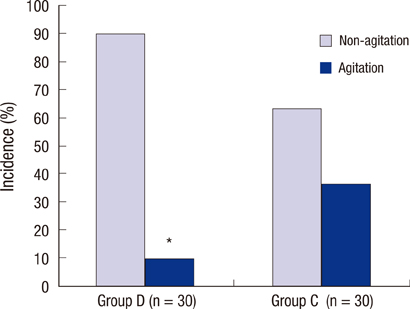
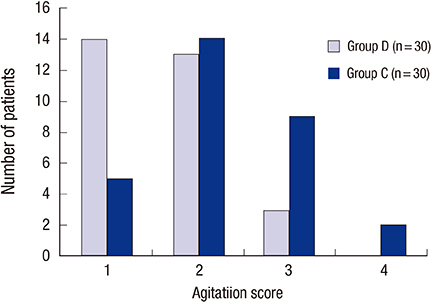
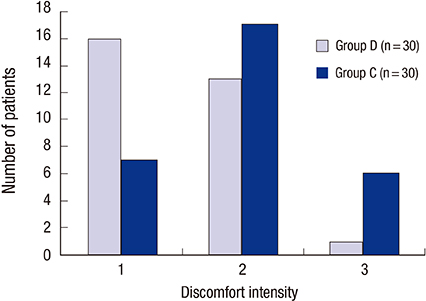
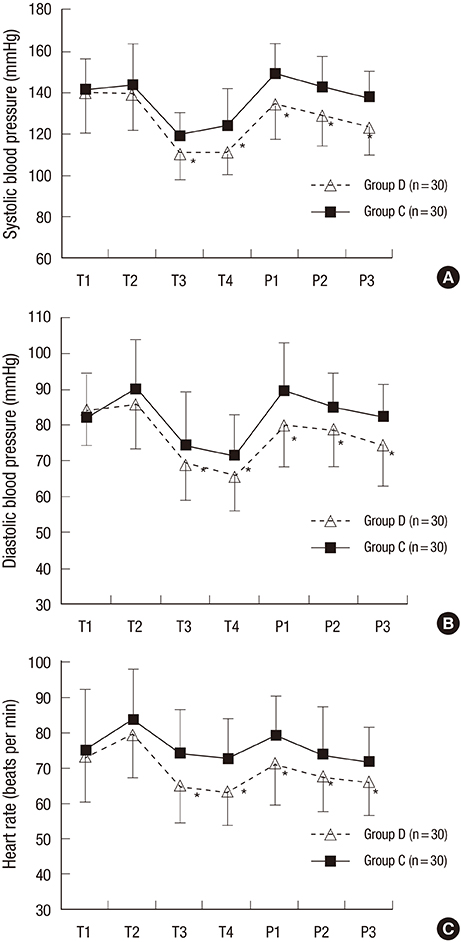
- Transurethral resection has been the gold standard in the operative management of benign prostatic hyperplasia and bladder tumor; however, it is associated with several complications that may cause patient discomfort. We evaluated the usefulness of continuous infusion of dexmedetomidine on emergence agitation, hemodynamic status, and recovery profiles in patients undergoing elective surgery by a randomized clinical trial. Sixty patients aged 30 to 80 yr who were scheduled for elective transurethral resection under general anesthesia were included in this study. Participants were randomly assigned to two groups (control group, group C; dexmedetomidine group, group D). A total of 60 male patients were enrolled in this study and randomly assigned to group C (n=30) or group D (n=30). The quality of emergence in group D was marked by a significantly lower incidence of emergence agitation than in group C (P=0.015). Patients in group D therefore felt less discomfort induced by the indwelling Foley catheter than those in group C (P=0.022). No statistically significant differences were found between the two groups with respect to side effects including bradycardia (P=0.085), hypotension (P=0.640), and postoperative nausea and vomiting (P=0.389). Our study showed that intraoperative dexmedetomidine infusion effectively reduced the incidence and intensity of emergence agitation and catheter-induced bladder discomfort without delaying recovery time and discharge time, thus providing smooth emergence during the recovery period in patients undergoing transurethral resection (Clinical Trial Registry No. KT0001683).
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Blood Pressure
Bradycardia/etiology
Dexmedetomidine/adverse effects/*therapeutic use
Hemodynamics
Humans
Hypnotics and Sedatives/adverse effects/*therapeutic use
Hypotension/etiology
Male
Middle Aged
Nausea/etiology
Prostatic Hyperplasia/*surgery
Psychomotor Agitation/*drug therapy
*Transurethral Resection of Prostate
Vomiting/etiology
Dexmedetomidine
Hypnotics and Sedatives
Figure
Cited by 1 articles
-
Anesthetic considerations for urologic surgeries
Chang-Hoon Koo, Jung-Hee Ryu
Korean J Anesthesiol. 2020;73(2):92-102. doi: 10.4097/kja.19437.
Reference
-
1. De Nunzio C, Aronson W, Freedland SJ, Giovannucci E, Parsons JK. The correlation between metabolic syndrome and prostatic diseases. Eur Urol. 2012; 61:560–570.2. Chrysostomou C, Schmitt CG. Dexmedetomidine: sedation, analgesia and beyond. Expert Opin Drug Metab Toxicol. 2008; 4:619–627.3. Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970; 49:924–934.4. Cohen IT, Hannallah RS, Hummer KA. The incidence of emergence agitation associated with desflurane anesthesia in children is reduced by fentanyl. Anesth Analg. 2001; 93:88–91.5. Andersson KE, Wein AJ. Pharmacology of the lower urinary tract: basis for current and future treatments of urinary incontinence. Pharmacol Rev. 2004; 56:581–631.6. Andersson KE. Advances in the pharmacological control of the bladder. Exp Physiol. 1999; 84:195–213.7. Yarker YE, Goa KL, Fitton A. Oxybutynin. A review of its pharmacodynamic and pharmacokinetic properties, and its therapeutic use in detrusor instability. Drugs Aging. 1995; 6:243–262.8. Benner JS, Nichol MB, Rovner ES, Jumadilova Z, Alvir J, Hussein M, Fanning K, Trocio JN, Brubaker L. Patient-reported reasons for discontinuing overactive bladder medication. BJU Int. 2010; 105:1276–1282.9. Maze M, Scarfini C, Cavaliere F. New agents for sedation in the intensive care unit. Crit Care Clin. 2001; 17:881–897.10. Ji F, Li Z, Nguyen H, Young N, Shi P, Fleming N, Liu H. Perioperative dexmedetomidine improves outcomes of cardiac surgery. Circulation. 2013; 127:1576–1584.11. Sato M, Shirakami G, Tazuke-Nishimura M, Matsuura S, Tanimoto K, Fukuda K. Effect of single-dose dexmedetomidine on emergence agitation and recovery profiles after sevoflurane anesthesia in pediatric ambulatory surgery. J Anesth. 2010; 24:675–682.12. Guler G, Akin A, Tosun Z, Ors S, Esmaoglu A, Boyaci A. Single-dose dexmedetomidine reduces agitation and provides smooth extubation after pediatric adenotonsillectomy. Paediatr Anaesth. 2005; 15:762–766.13. Yu D, Chai W, Sun X, Yao L. Emergence agitation in adults: risk factors in 2,000 patients. Can J Anaesth. 2010; 57:843–848.14. Agarwal A, Raza M, Singhal V, Dhiraaj S, Kapoor R, Srivastava A, Gupta D, Singh PK, Pandey CK, Singh U. The efficacy of tolterodine for prevention of catheter-related bladder discomfort: a prospective, randomized, placebo-controlled, double-blind study. Anesth Analg. 2005; 101:1065–1067.15. Agarwal A, Dhiraaj S, Pawar S, Kapoor R, Gupta D, Singh PK. An evaluation of the efficacy of gabapentin for prevention of catheter-related bladder discomfort: a prospective, randomized, placebo-controlled, double-blind study. Anesth Analg. 2007; 105:1454–1457.16. Kim NY, Kim SY, Yoon HJ, Kil HK. Effect of dexmedetomidine on sevoflurane requirements and emergence agitation in children undergoing ambulatory surgery. Yonsei Med J. 2014; 55:209–215.17. Shukry M, Clyde MC, Kalarickal PL, Ramadhyani U. Does dexmedetomidine prevent emergence delirium in children after sevoflurane-based general anesthesia. Paediatr Anaesth. 2005; 15:1098–1104.18. Afonso J, Reis F. Dexmedetomidine: current role in anesthesia and intensive care. Rev Bras Anestesiol. 2012; 62:118–133.19. Venn RM, Bradshaw CJ, Spencer R, Brealey D, Caudwell E, Naughton C, Vedio A, Singer M, Feneck R, Treacher D, et al. Preliminary UK experience of dexmedetomidine, a novel agent for postoperative sedation in the intensive care unit. Anaesthesia. 1999; 54:1136–1142.20. Kamibayashi T, Maze M. Clinical uses of alpha2 -adrenergic agonists. Anesthesiology. 2000; 93:1345–1349.21. Ingersoll-Weng E, Manecke GR Jr, Thistlethwaite PA. Dexmedetomidine and cardiac arrest. Anesthesiology. 2004; 100:738–739.22. Aho M, Erkola O, Kallio A, Scheinin H, Korttila K. Comparison of dexmedetomidine and midazolam sedation and antagonism of dexmedetomidine with atipamezole. J Clin Anesth. 1993; 5:194–203.23. Short J. Use of dexmedetomidine for primary sedation in a general intensive care unit. Crit Care Nurse. 2010; 30:29–38.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of intraoperative dexmedetomidine infusion on visualization of the surgical field in endoscopic sinus surgery
- Effect of Dexmedetomidine on Sevoflurane Requirements and Emergence Agitation in Children Undergoing Ambulatory Surgery
- Preanesthetic dexmedetomidine 1 microg/kg single infusion is a simple, easy, and economic adjuvant for general anesthesia
- Postoperative infusion of a low dose of dexmedetomidine reduces intravenous consumption of sufentanil in patient-controlled analgesia
- Effects of remimazolam versus dexmedetomidine on recovery after transcatheter aortic valve replacement under monitored anesthesia care: a propensity score-matched, non-inferiority study