Anesth Pain Med.
2016 Apr;11(2):195-200. 10.17085/apm.2016.11.2.195.
Palonosetron might not attenuate spinal anesthesia-induced hypotension during orthopedic surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Gachon University Gil Medical Center, Incheon, Korea. endless37@gilhospital.com
- KMID: 2358485
- DOI: http://doi.org/10.17085/apm.2016.11.2.195
Abstract
- BACKGROUND
5-Hydroxytryptamine3 (5-HT3) receptor antagonists have been reported to attenuate spinal anesthesia-induced hemodynamic changes. This study was conducted to determine whether the second generation 5-HT3, antagonist palonosetron attenuates hypotension and bradycardia during spinal anesthesia.
METHODS
Sixty adult patients scheduled for lower limb surgery were enrolled in this study. Patients were randomly assigned to receive either normal saline (Control group, N = 30) or palonosetron (0.075 mg, i.v.) (Palonosetron group, N = 30) prior to spinal anesthesia. Hemodynamic variables were recorded during anesthesia.
RESULTS
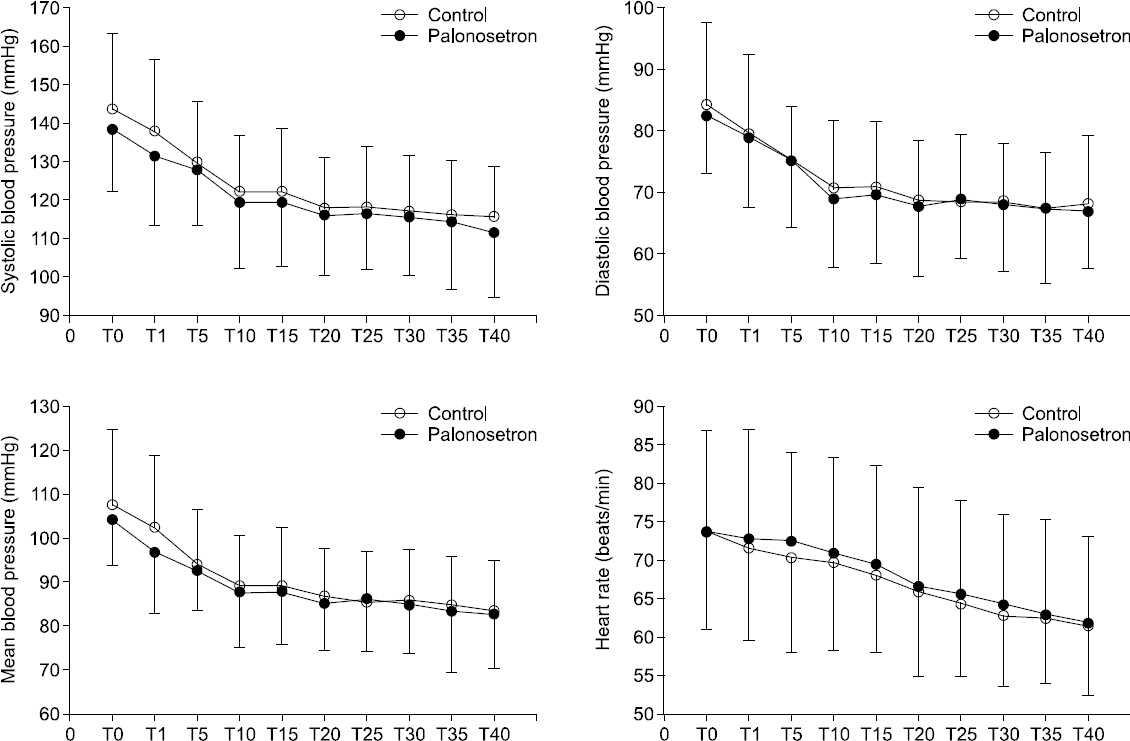
The mean blood pressure (MBP) were 89.2 ± 11.4 mmHg in the control group and 87.6 ± 12.1 mmHg in the palonosetron group at 10 min after intrathecal injection (P = 0.609). The median blocked levels of the control group and the palonosetron group were T10 (interquartile range, 9-10) and T10 (8-10) at 20 min after intrathecal injection (P = 0.939). Requirements for ephedrine, phenylephrine, and atropine were similar (P = 0.652, 0.533 and 0.417, respectively). The incidences of hypotension (40% vs. 41%) and bradycardia (7% vs. 17%) were comparable (P = 0.562, P = 0.198, respectively) between the control and the palonosetron group. There were no significances in the changes of systolic blood pressure, diastolic blood pressure, MBP and heart rate by the group (P = 0.632, 0.287, 0.556, 0.733, respectively).
CONCLUSIONS
Intravenous palonosetron (0.075 mg) prior to spinal anesthesia might not attenuate spinal anesthesia-induced hypotension during low level of neuroaxial block for lower limb surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Carpenter RL, Caplan RA, Brown DL, Stephenson C, Wu R. Incidence and risk factors for side effects of spinal anesthesia. Anesthesiology. 1992; 76:906–16. DOI: 10.1097/00000542-199206000-00006. PMID: 1599111.
Article2. Somboonviboon W, Kyokong O, Charuluxananan S, Narasethakamol A. Incidence and risk factors of hypotension and bradycardia after spinal anesthesia for cesarean section. J Med Assoc Thai. 2008; 91:181–7. PMID: 18389982.3. Rooke GA, Freund PR, Jacobson AF. Hemodynamic response and change in organ blood volume during spinal anesthesia in elderly men with cardiac disease. Anesth Analg. 1997; 85:99–105. DOI: 10.1097/00000539-199707000-00018. PMID: 9212130.
Article4. Butterworth J. Physiology of spinal anesthesia: what are the implications for management? Reg Anesth Pain Med. 1998; 23:370–3. DOI: 10.1016/S1098-7339(98)90008-6. PMID: 9690588.
Article5. Brooker RF, Butterworth JF 4th, Kitzman DW, Berman JM, Kashtan HI, McKinley AC. Treatment of hypotension after hyperbaric tetracaine spinal anesthesia. A randomized, double-blind, cross-over comparison of phenylephrine and epinephrine. Anesthesiology. 1997; 86:797–805. DOI: 10.1097/00000542-199704000-00009. PMID: 9105223.6. Critchley LA, Conway F. Hypotension during subarachnoid anaesthesia: haemodynamic effects of colloid and metaraminol. Br J Anaesth. 1996; 76:734–6. DOI: 10.1093/bja/76.5.734.
Article7. Løvstad RZ, Granhus G, Hetland S. Bradycardia and asystolic cardiac arrest during spinal anaesthesia: a report of five cases. Acta Anaesthesiol Scand. 2000; 44:48–52. DOI: 10.1034/j.1399-6576.2000.440109.x. PMID: 10669271.
Article8. Ou CH, Tsou MY, Ting CK, Chiou CS, Chan KH, Tsai SK. Occurrence of the Bezold-Jarisch reflex during Cesarean section under spinal anesthesia--a case report. Acta Anaesthesiol Taiwan. 2004; 42:175–8. PMID: 15551897.9. Saxena PR, Villalón CM. Cardiovascular effects of serotonin agonists and antagonists. J Cardiovasc Pharmacol. 1990; 15(Suppl 7):S17–34. DOI: 10.1097/00005344-199001001-00004. PMID: 1702484.
Article10. Owczuk R, Wenski W, Polak-Krzeminska A, Twardowski P, Arszułowicz R, Dylczyk-Sommer A, et al. Ondansetron given intravenously attenuates arterial blood pressure drop due to spinal anesthesia: a double-blind, placebo-controlled study. Reg Anesth Pain Med. 2008; 33:332–9. DOI: 10.1097/00115550-200807000-00008. PMID: 18675744.
Article11. Eldaba AA, Amr YM. Intravenous granisetron attenuates hypotension during spinal anesthesia in cesarean delivery: A double-blind, prospective randomized controlled study. J Anaesthesiol Clin Pharmacol. 2015; 31:329–32. DOI: 10.4103/0970-9185.161667. PMID: 26330710. PMCID: PMC4541178.
Article12. Kim YY, Song DU, Lee KH, Lee IJ, Song JW, Lim JH. Comparison of palonosetron with ondansetron in preventing postoperative nausea and vomiting after thyroidectomy during a 48-hour period. Anesth Pain Med. 2012; 7:312–6.13. Gupta K, Singh I, Gupta PK, Chauhan H, Jain M, Rastogi B. Palonosetron, Ondansetron, and Granisetron for antiemetic prophylaxis of postoperative nausea and vomiting - A comparative evaluation. Anesth Essays Res. 2014; 8:197–201. DOI: 10.4103/0259-1162.134503. PMID: 25886226. PMCID: PMC4173632.
Article14. Aviado DM, Guevara Aviado D. The Bezold-Jarisch reflex. A historical perspective of cardiopulmonary reflexes. Ann N Y Acad Sci. 2001; 940:48–58. DOI: 10.1111/j.1749-6632.2001.tb03666.x. PMID: 11458703.15. Kinsella SM, Tuckey JP. Perioperative bradycardia and asystole: relationship to vasovagal syncope and the Bezold-Jarisch reflex. Br J Anaesth. 2001; 86:859–68. DOI: 10.1093/bja/86.6.859.
Article16. Nichols DE, Nichols CD. Serotonin receptors. Chem Rev. 2008; 108:1614–41. DOI: 10.1021/cr078224o. PMID: 18476671.
Article17. Adams VR, Valley AW. Granisetron: the second serotonin-receptor antagonist. Ann Pharmacother. 1995; 29:1240–51. PMID: 8672830.
Article18. Rojas C, Stathis M, Thomas AG, Massuda EB, Alt J, Zhang J, et al. Palonosetron exhibits unique molecular interactions with the 5-HT3 receptor. Anesth Analg. 2008; 107:469–78. DOI: 10.1213/ane.0b013e318172fa74. PMID: 18633025.
Article19. Shin HJ, Choi ES, Lee GW, Do SH. Effects of Preoperative Serotonin-Receptor-Antagonist Administration in Spinal Anesthesia-Induced Hypotension: A Randomized, Double-blind Comparison Study of Ramosetron and Ondansetron. Reg Anesth Pain Med. 2015; 40:583–8. DOI: 10.1097/AAP.0000000000000300. PMID: 26263075.
Article20. Ortiz-Gómez JR, Palacio-Abizanda FJ, Morillas-Ramirez F, Fornet-Ruiz I, Lorenzo-Jiménez A, Bermejo-Albares ML, et al. The effect of intravenous ondansetron on maternal haemodynamics during elective caesarean delivery under spinal anaesthesia: a double-blind, randomised, placebo-controlled trial. Int J Obstet Anesth. 2014; 23:138–43. DOI: 10.1016/j.ijoa.2014.01.005. PMID: 24631057.
Article21. Singla D, Kathuria S, Singh A, Kaul T, Gupta S, Mamta . Risk factors for development of early hypotension during spinal anaesthesia. J Anaesthesiol Clin Pharmacol. 2006; 22:387–93.22. Owczuk R, Wenski W, Twardowski P, Dylczyk-Sommer A, Sawicka W, Wujtewicz MA, et al. Ondansetron attenuates the decrease in blood pressure due to spinal anesthesia in the elderly: a double blind, placebo-controlled study. Minerva Anestesiol. 2015; 81:598–607. PMID: 25220555.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of hypotension after spinal anesthesia administered for caesarean section
- Use of vasopressors to manage spinal anesthesia-induced hypotension during cesarean delivery
- Hemodynamic effects of norepinephrine versus phenylephrine infusion for prophylaxis against spinal anesthesia-induced hypotension in the elderly population undergoing hip fracture surgery: a randomized controlled trial
- Evaluation of the ability of continuous palonosetron infusion, using a patient-controlled analgesia device, to reduce postoperative nausea and vomiting
- The Effect of Preanesthetic Administration of Crystalloid for Prevention of Spinal Anesthesia-Induced Hypotension