J Korean Med Assoc.
2016 Nov;59(11):857-865. 10.5124/jkma.2016.59.11.857.
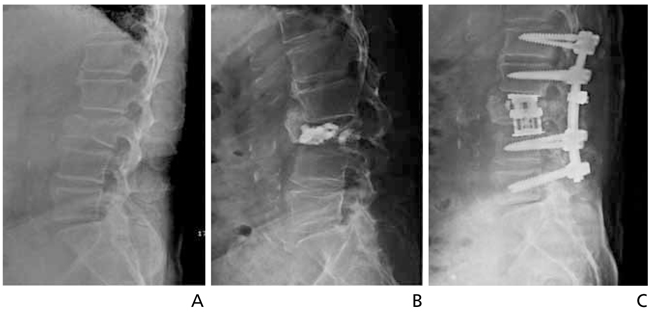
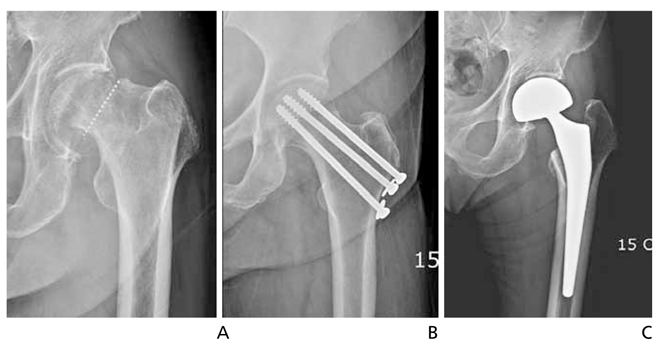
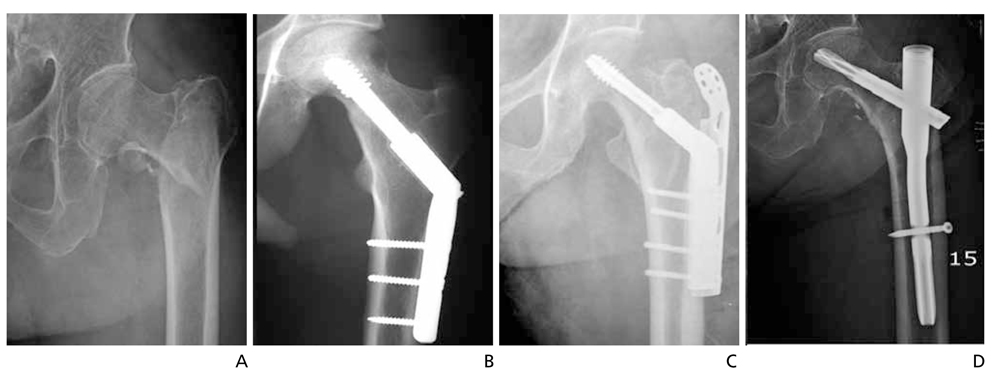
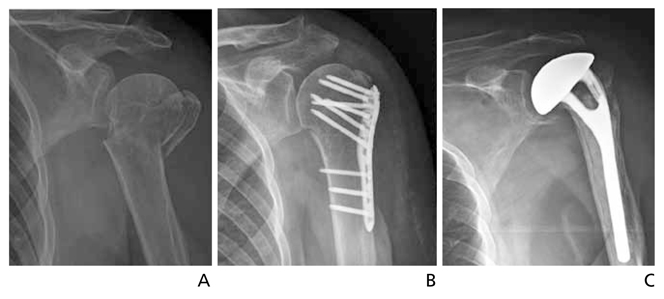
Surgical or nonsurgical treatment of osteoporotic fractures
- Affiliations
-
- 1Department of Orthopaedic Surgery, Korea University College of Medicine, Seoul, Korea. drspine90@gmail.com
- KMID: 2358433
- DOI: http://doi.org/10.5124/jkma.2016.59.11.857
Abstract
- The worldwide population of the elderly is steadily increasing, and even more so in Korea, thus causing an increase in the osteoporotic fracture prevalence. Osteoporotic fracture is a serious injury that can decrease quality of life, and can also produce major social problems when it causes mortality. Preventing such fractures from happening in the first place is of utmost importance but once a fracture does occur, it is important to select appropriate treatment modalities to prevent secondary fractures. Recently, with the increase of life expectancy, it has become favorable to perform surgical fixation for significantly displaced osteoporotic fractures and use early rehabilitation programs to return the patient to normal body performance as soon as possible. To do so, it is important to accurately assess the location and the degree of the fractures in order to select appropriate treatment modalities. Furthermore, it is important to prevent secondary fractures from happening once the previous fractures heal.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Ageing society and osteoporosis
Kyu Hyun Yang
J Korean Med Assoc. 2016;59(11):833-835. doi: 10.5124/jkma.2016.59.11.833.Safety and Effectiveness of the Anchor Augmentation with Bone Cement on Osteoporotic Femoral Fracture: A Systematic Reviews
So Young Kim
J Korean Fract Soc. 2019;32(2):89-96. doi: 10.12671/jkfs.2019.32.2.89.
Reference
-
1. NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001; 285:785–795.2. Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE Jr, McLellan A, Mitchell PJ, Silverman S, Singleton R, Siris E. ASBMR Task Force on Secondary Fracture Prevention. Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res. 2012; 27:2039–2046.
Article3. Dell R, Greene D, Schelkun SR, Williams K. Osteoporosis disease management: the role of the orthopaedic surgeon. J Bone Joint Surg Am. 2008; 90:Suppl 4. 188–194.
Article4. Yoo JH, Moon SH, Ha YC, Lee DY, Gong HS, Park SY, Yang KH. Osteoporotic fracture: 2015 position statement of the Korean Society for Bone and Mineral Research. J Bone Metab. 2015; 22:175–181.
Article5. Haentjens P, Autier P, Collins J, Velkeniers B, Vanderschueren D, Boonen S. Colles fracture, spine fracture, and subsequent risk of hip fracture in men and women: a meta-analysis. J Bone Joint Surg Am. 2003; 85:1936–1943.
Article6. Lee YK, Jang S, Jang S, Lee HJ, Park C, Ha YC, Kim DY. Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int. 2012; 23:1859–1865.7. Park C, Ha YC, Jang S, Jang S, Yoon HK, Lee YK. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab. 2011; 29:744–751.
Article8. Ha YC, Park YG, Nam KW, Kim SR. Trend in hip fracture incidence and mortality in Korea: a prospective cohort study from 2002 to 2011. J Korean Med Sci. 2015; 30:483–488.
Article9. Matin P. The appearance of bone scans following fractures, including immediate and long-term studies. J Nucl Med. 1979; 20:1227–1231.10. Park SY, Lee SH, Suh SW, Park JH, Kim TG. Usefulness of MRI in determining the appropriate level of cement augmentation for acute osteoporotic vertebral compression fractures. J Spinal Disord Tech. 2013; 26:E80–E85.
Article11. Takahashi S, Hoshino M, Takayama K, Iseki K, Sasaoka R, Tsujio T, Yasuda H, Sasaki T, Kanematsu F, Kono H, Toyoda H, Nakamura H. Time course of osteoporotic vertebral fractures by magnetic resonance imaging using a simple classification: a multicenter prospective cohort study. Osteoporos Int. 2016; 08. 30. [Epub]. DOI: 10.1007/s00198-016-3737-x.
Article12. Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O. European Vertebral Osteoporosis Study. Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int. 2003; 14:61–68.
Article13. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006; 17:1726–1733.
Article14. Yoon SP, Lee SH, Ki CH, Lee YT, Hong SH, Lee HM, Moon SH. Quality of life in patients with osteoporotic vertebral fractures. Asian Spine J. 2014; 8:653–658.
Article15. Papaioannou A, Watts NB, Kendler DL, Yuen CK, Adachi JD, Ferko N. Diagnosis and management of vertebral fractures in elderly adults. Am J Med. 2002; 113:220–228.
Article16. Fahrleitner-Pammer A, Langdahl BL, Marin F, Jakob F, Karras D, Barrett A, Ljunggren O, Walsh JB, Rajzbaum G, Barker C, Lems WF. Fracture rate and back pain during and after discontinuation of teriparatide: 36-month data from the European Forsteo Observational Study (EFOS). Osteoporos Int. 2011; 22:2709–2719.
Article17. Tsuchie H, Miyakoshi N, Kasukawa Y, Nishi T, Abe H, Segawa T, Shimada Y. The effect of teriparatide to alleviate pain and to prevent vertebral collapse after fresh osteoporotic vertebral fracture. J Bone Miner Metab. 2016; 34:86–91.
Article18. Fujita T, Ohue M, Fujii Y, Miyauchi A, Takagi Y. Comparison of the analgesic effects of bisphosphonates: etidronate, alendronate and risedronate by electroalgometry utilizing the fall of skin impedance. J Bone Miner Metab. 2009; 27:234–239.
Article19. Kim HJ, Yi JM, Cho HG, Chang BS, Lee CK, Kim JH, Yeom JS. Comparative study of the treatment outcomes of osteoporotic compression fractures without neurologic injury using a rigid brace, a soft brace, and no brace: a prospective randomized controlled non-inferiority trial. J Bone Joint Surg Am. 2014; 96:1959–1966.
Article20. Gnanenthiran SR, Adie S, Harris IA. Nonoperative versus operative treatment for thoracolumbar burst fractures without neurologic deficit: a meta-analysis. Clin Orthop Relat Res. 2012; 470:567–577.
Article21. Lee HM, Park SY, Lee SH, Suh SW, Hong JY. Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs): conservative treatment versus balloon kyphoplasty. Spine J. 2012; 12:998–1005.
Article22. Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009; 361:557–568.
Article23. Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W, Ghdoke B, Annesley-Williams DJ, Ralston SH, Jarvik JG. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009; 361:569–579.
Article24. Itshayek E, Miller P, Barzilay Y, Hasharoni A, Kaplan L, Fraifeld S, Cohen JE. Vertebral augmentation in the treatment of vertebral compression fractures: review and new insights from recent studies. J Clin Neurosci. 2012; 19:786–791.
Article25. Healy WL, Iorio R. Total hip arthroplasty: optimal treatment for displaced femoral neck fractures in elderly patients. Clin Orthop Relat Res. 2004; (429):43–48.26. Kain MS, Marcantonio AJ, Iorio R. Revision surgery occurs frequently after percutaneous fixation of stable femoral neck fractures in elderly patients. Clin Orthop Relat Res. 2014; 472:4010–4014.
Article27. Park SY, Yang KH, Yoo JH, Yoon HK, Park HW. The treatment of reverse obliquity intertrochanteric fractures with the intramedullary hip nail. J Trauma. 2008; 65:852–857.
Article28. Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2005; (4):CD000093.
Article29. Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster DW, Ebeling PR, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O'Keefe R, Papapoulos S, Howe TS, van der Meulen MC, Weinstein RS, Whyte MP. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29:1–23.
Article30. Girgis CM, Sher D, Seibel MJ. Atypical femoral fractures and bisphosphonate use. N Engl J Med. 2010; 362:1848–1849.
Article31. Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005; 90:1294–1301.
Article32. Kim S, Yang KH, Lim H, Lee YK, Yoon HK, Oh CW, Park KK, Min BW, Ryu JA, Kwack KS, Lee YH. Detection of prefracture hip lesions in atypical subtrochanteric fracture with dual-energy X-ray absorptiometry images. Radiology. 2014; 270:487–495.
Article33. Yang KH, Min BW, Ha YC. Atypical femoral fracture: 2015 position statement of the Korean Society for Bone and Mineral Research. J Bone Metab. 2015; 22:87–91.
Article34. Lee YK, Ha YC, Kang BJ, Chang JS, Koo KH. Predicting need for fixation of atypical femoral fracture. J Clin Endocrinol Metab. 2013; 98:2742–2745.
Article35. Gong HS, Oh WS, Chung MS, Oh JH, Lee YH, Baek GH. Patients with wrist fractures are less likely to be evaluated and managed for osteoporosis. J Bone Joint Surg Am. 2009; 91:2376–2380.
Article36. Handoll HH, Vaghela MV, Madhok R. Percutaneous pinning for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2007; (3):CD006080.
Article37. Taras JS, Ladd AL, Kalainov DM, Ruch DS, Ring DC. New concepts in the treatment of distal radius fractures. Instr Course Lect. 2010; 59:313–332.38. Murray IR, Amin AK, White TO, Robinson CM. Proximal humeral fractures: current concepts in classification, treatment and outcomes. J Bone Joint Surg Br. 2011; 93:1–11.39. Xue Q, Li H, Zou X, Bunger M, Egund N, Lind M, Christensen FB, Bunger C. The influence of alendronate treatment and bone graft volume on posterior lateral spine fusion in a porcine model. Spine (Phila Pa 1976). 2005; 30:1116–1121.
Article40. Gong HS, Song CH, Lee YH, Rhee SH, Lee HJ, Baek GH. Early initiation of bisphosphonate does not affect healing and outcomes of volar plate fixation of osteoporotic distal radial fractures. J Bone Joint Surg Am. 2012; 94:1729–1736.
Article41. Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, Kuniyoshi K, Aoki Y, Nakamura J, Ishikawa T, Miyagi M, Kamoda H, Suzuki M, Kubota G, Sakuma Y, Oikawa Y, Inage K, Sainoh T, Takaso M, Ozawa T, Takahashi K, Toyone T. Teriparatide accelerates lumbar posterolateral fusion in women with postmenopausal osteoporosis: prospective study. Spine (Phila Pa 1976). 2012; 37:E1464–E1468.42. Hirsch BP, Unnanuntana A, Cunningham ME, Lane JM. The effect of therapies for osteoporosis on spine fusion: a systematic review. Spine J. 2013; 13:190–199.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osteoporotic Hip Fracture: How We Make Better Results?
- Pelvis/Acetabular Fractures in the Elderly: When and How to Fix?
- Nonsurgical Treatment Strategies after Osteoporotic Hip Fractures
- The Epidemiology and Importance of Osteoporotic Spinal Compression Fracture in South Korea
- Percutaneous Vertebral Augmentation for the Treatment of Osteoporotic Spinal Fractures