J Korean Fract Soc.
2018 Jul;31(3):102-113. 10.12671/jkfs.2018.31.3.102.
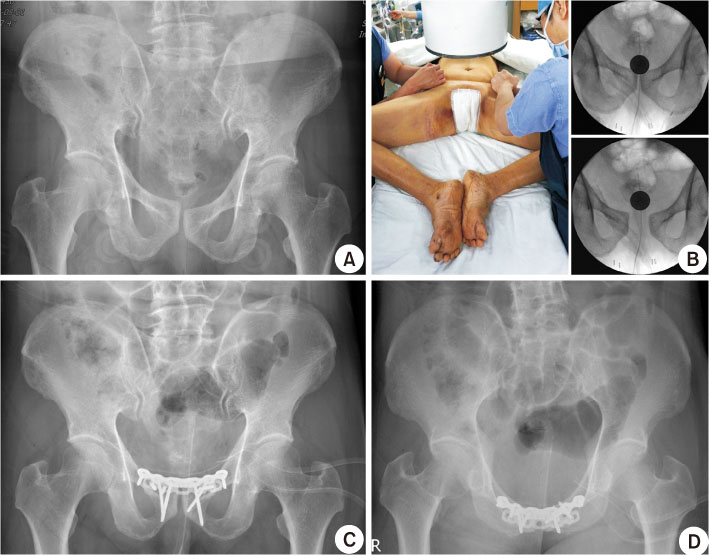
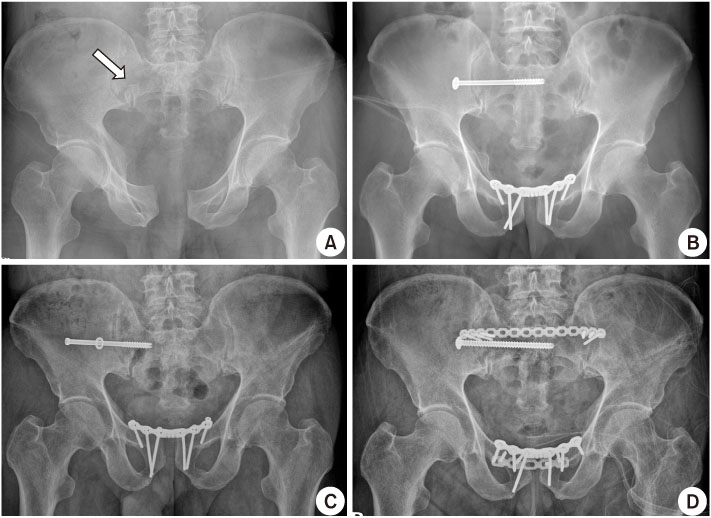
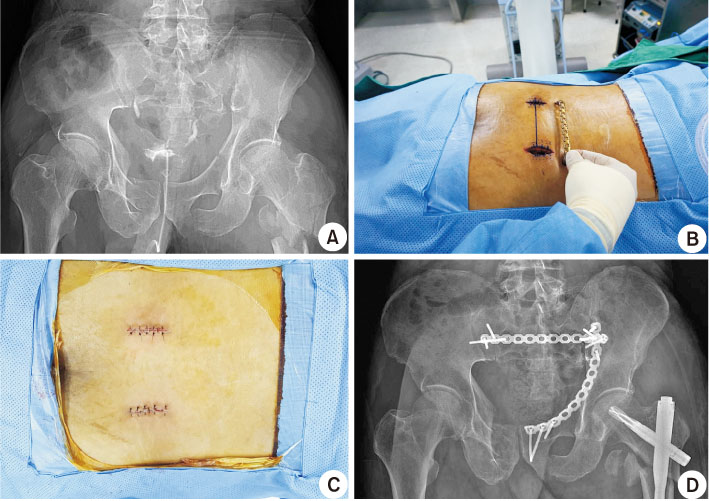
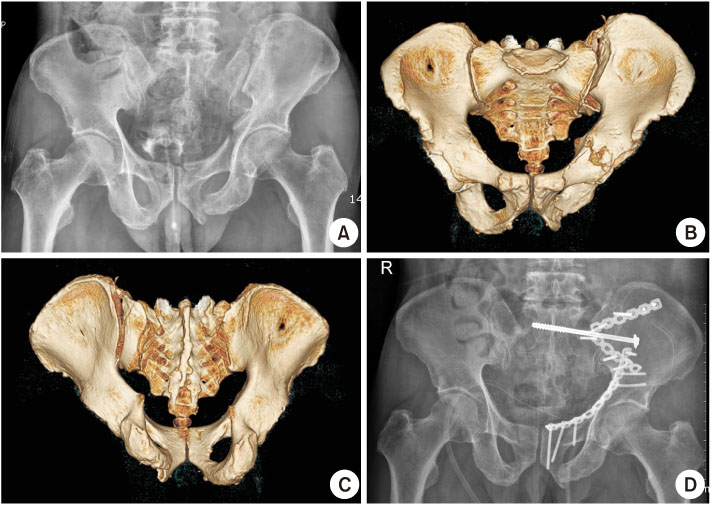
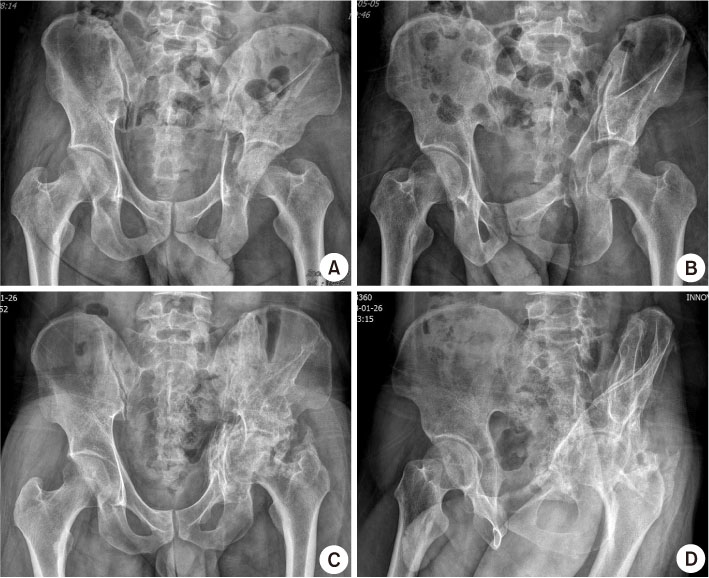
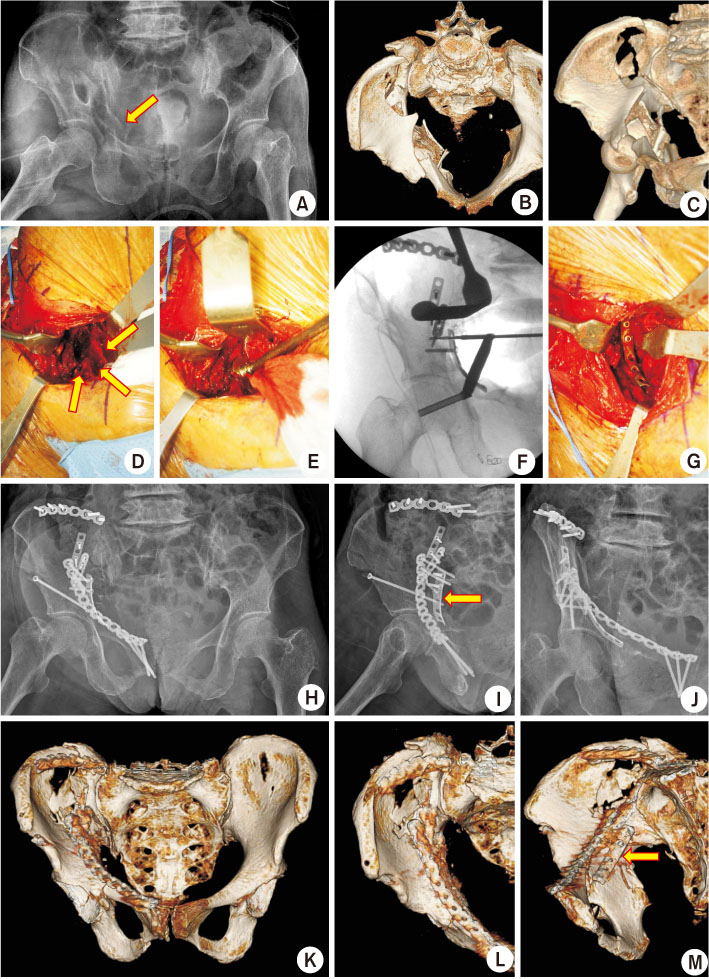
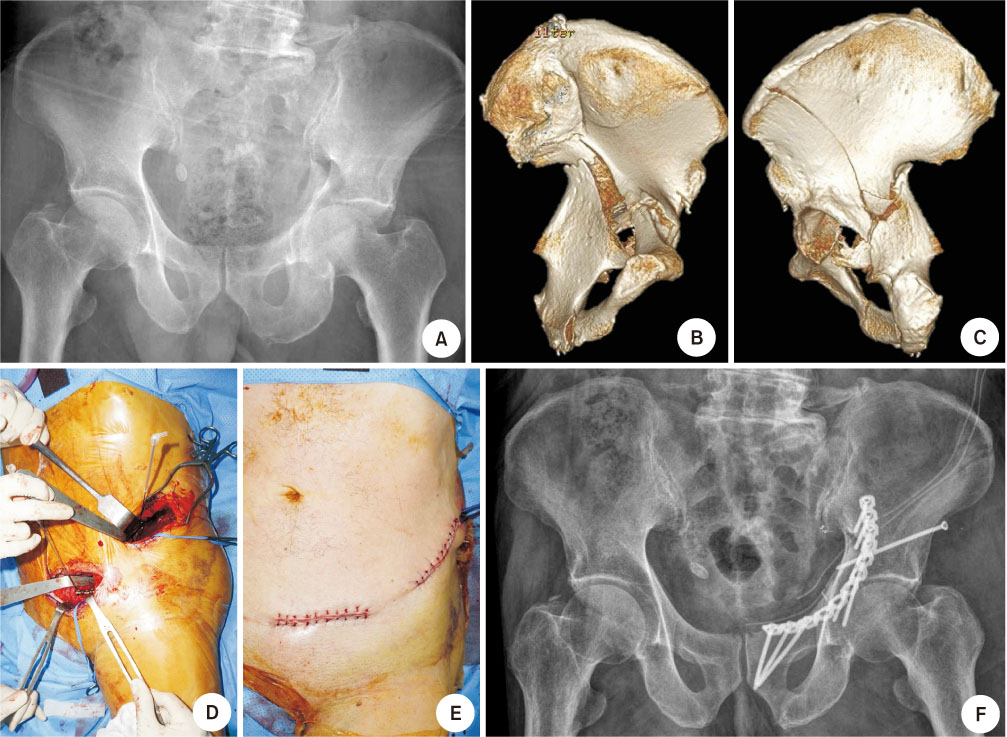
Pelvis/Acetabular Fractures in the Elderly: When and How to Fix?
- Affiliations
-
- 1Department of Orthopaedic Surgery, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Korea. joonwoo@knu.ac.kr
- KMID: 2417152
- DOI: http://doi.org/10.12671/jkfs.2018.31.3.102
Abstract
- Owing to the increase in life expectancy, the incidence of osteoporotic fracture of the pelvis and acetabulum is increasing. Fractures in the elderly population is different from those in younger patients. Pelvic ring and acetabular fractures in geriatric patients are more likely the result of low-energy trauma, but the outcomes are generally poorer than those of the younger population. Multiple management options are available, but no intervention has become the standard of care for these fractures in the elderly. A treatment strategy should be established depending on the state of the individual patient. Regardless of whether nonsurgical or surgical treatment is selected, early ambulation should be considered to avoid the complications associated with prolonged immobilization.
Keyword
MeSH Terms
Figure
Reference
-
1. Fuchs T, Rottbeck U, Hofbauer V, Raschke M, Stange R. Pelvic ring fractures in the elderly. Underestimated osteoporotic fracture. Unfallchirurg. 2011; 114:663–670.2. Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010; 92:250–257.3. Gotis-Graham I, McGuigan L, Diamond T, et al. Sacral insufficiency fractures in the elderly. J Bone Joint Surg Br. 1994; 76:882–886.
Article4. Clement ND, Aitken S, Duckworth AD, McQueen MM, Court-Brown CM. Multiple fractures in the elderly. J Bone Joint Surg Br. 2012; 94:231–236.
Article5. Weber M, Hasler P, Gerber H. Sacral insufficiency fractures as an unsuspected cause of low back pain. Rheumatology (Oxford). 1999; 38:90–91.
Article6. Rommens PM, Wagner D, Hofmann A. Surgical management of osteoporotic pelvic fractures: a new challenge. Eur J Trauma Emerg Surg. 2012; 38:499–509.
Article7. Dalal SA, Burgess AR, Siegel JH, et al. Pelvic fracture in multiple trauma: classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma. 1989; 29:981–1000. discussion 1000–1002.8. Tile M. Pelvic ring fractures: should they be fixed. J Bone Joint Surg Br. 1988; 70:1–12.
Article9. Linstrom NJ, Heiserman JE, Kortman KE, et al. Anatomical and biomechanical analyses of the unique and consistent locations of sacral insufficiency fractures. Spine (Phila Pa 1976). 2009; 34:309–331.
Article10. Robles LA. Transverse sacral fractures. Spine J. 2009; 9:60–69.
Article11. Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 2013; 44:1733–1744.
Article12. Lustenberger T, Meier C, Benninger E, Lenzlinger PM, Keel MJ. C-clamp and pelvic packing for control of hemorrhage in patients with pelvic ring disruption. J Emerg Trauma Shock. 2011; 4:477–482.13. Vécsei V, Negrin LL, Hajdu S. Today's role of external fixation in unstable and complex pelvic fractures. Eur J Trauma Emerg Surg. 2010; 36:100–106.
Article14. Lau TW, Leung F. Occult posterior pelvic ring fractures in elderly patients with osteoporotic pubic rami fractures. J Orthop Surg (Hong Kong). 2010; 18:153–157.
Article15. Tosounidis G, Wirbel R, Culemann U, Pohlemann T. Misinterpretation of anterior pelvic ring fractures in the elderly. Unfallchirurg. 2006; 109:678–680.16. Culemann U, Scola A, Tosounidis G, Pohlemann T, Gebhard F. Concept for treatment of pelvic ring injuries in elderly patients. A challenge. Unfallchirurg. 2010; 113:258–271.17. Gänsslen A, Hüfner T, Krettek C. Percutaneous iliosacral screw fixation of unstable pelvic injuries by conventional fluoroscopy. Oper Orthop Traumatol. 2006; 18:225–244.18. Kim JW, Oh CW, Oh JK, et al. Percutaneous iliosacral screwing in pelvic ring injury using three-dimensional fluoroscopy. J Orthop Sci. 2013; 18:87–92.
Article19. Kraemer W, Hearn T, Tile M, Powell J. The effect of thread length and location on extraction strengths of iliosacral lag screws. Injury. 1994; 25:5–9.
Article20. Kim JW, Oh CW, Oh JK, et al. The incidence of and factors affecting iliosacral screw loosening in pelvic ring injury. Arch Orthop Trauma Surg. 2016; 136:921–927.
Article21. Tjardes T, Paffrath T, Baethis H, et al. Computer assisted percutaneous placement of augmented iliosacral screws: a reasonable alternative to sacroplasty. Spine (Phila Pa 1976). 2008; 33:1497–1500.
Article22. Day AC, Kinmont C, Bircher MD, Kumar S. Crescent fracture-dislocation of the sacroiliac joint: a functional classification. J Bone Joint Surg Br. 2007; 89:651–658.23. Dienstknecht T, Berner A, Lenich A, Nerlich M, Fuechtmeier B. A minimally invasive stabilizing system for dorsal pelvic ring injuries. Clin Orthop Relat Res. 2011; 469:3209–3217.
Article24. Suzuki T, Hak DJ, Ziran BH, et al. Outcome and complications of posterior transiliac plating for vertically unstable sacral fractures. Injury. 2009; 40:405–409.
Article25. Moshirfar A, Rand FF, Sponseller PD, et al. Pelvic fixation in spine surgery. Historical overview, indications, biomechanical relevance, and current techniques. J Bone Joint Surg Am. 2005; 87:Suppl 2. 89–106.26. Keel MJ, Benneker LM, Siebenrock KA, Bastian JD. Less invasive lumbopelvic stabilization of posterior pelvic ring instability: technique and preliminary results. J Trauma. 2011; 71:E62–E70.
Article27. Carroll EA, Huber FG, Goldman AT, et al. Treatment of acetabular fractures in an older population. J Orthop Trauma. 2010; 24:637–644.
Article28. Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD. Acetabular fractures in patients aged > 55 years: a systematic review of the literature. Bone Joint J. 2014; 96:157–163.29. Butterwick D, Papp S, Gofton W, Liew A, Beaulé PE. Acetabular fractures in the elderly: evaluation and management. J Bone Joint Surg Am. 2015; 97:758–768.30. Kreder HJ, Rozen N, Borkhoff CM, et al. Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg Br. 2006; 88:776–782.
Article31. Bhandari M, Matta J, Ferguson T, Matthys G. Predictors of clinical and radiological outcome in patients with fractures of the acetabulum and concomitant posterior dislocation of the hip. J Bone Joint Surg Br. 2006; 88:1618–1624.
Article32. Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996; 78:1632–1645.33. Anglen JO, Burd TA, Hendricks KJ, Harrison P. The “Gull sign”: a harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma. 2003; 17:625–634.34. Mears DC. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg. 1999; 7:128–141.
Article35. Gänsslen A, Hildebrand F, Krettek C. Conservative treatment of acetabular both column fractures: does the concept of secondary congruence work. Acta Chir Orthop Traumatol Cech. 2012; 79:411–415.36. Helfet DL, Borrelli J Jr, DiPasquale T, Sanders R. Stabilization of acetabular fractures in elderly patients. J Bone Joint Surg Am. 1992; 74:753–765.
Article37. Laflamme GY, Hebert-Davies J. Direct reduction technique for superomedial dome impaction in geriatric acetabular fractures. J Orthop Trauma. 2014; 28:e39–e43.
Article38. Archdeacon MT, Kazemi N, Collinge C, Budde B, Schnell S. Treatment of protrusio fractures of the acetabulum in patients 70 years and older. J Orthop Trauma. 2013; 27:256–261.
Article39. Culemann U, Holstein JH, Köhler D, et al. Different stabilisation techniques for typical acetabular fractures in the elderly: a biomechanical assessment. Injury. 2010; 41:405–410.
Article40. Bellabarba C, Berger RA, Bentley CD, et al. Cementless acetabular reconstruction after acetabular fracture. J Bone Joint Surg Am. 2001; 83:868–876.
Article41. Tannast M, Najibi S, Matta JM. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am. 2012; 94:1559–1567.
Article42. Antell NB, Switzer JA, Schmidt AH. Management of acetabular fractures in the elderly. J Am Acad Orthop Surg. 2017; 25:577–585.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arthroscopic Reduction and Transportal Screw Fixation of Acetabular Posterior Wall Fracture: Technical Note
- Management of Intraoperative Acetabular Fractures in Total Hip Arthroplasty: A Current Concept Review
- Total Hip Arthroplasty after Acetabular Fracture: Acute Phase and Delayed Phase
- Acetabular Erosion after Peplacement of Femoral Head
- Surgical Treatment of Acetabular Posterior Wall Fracture with Hip Arthroscopy: A Case Report