Anesth Pain Med.
2016 Oct;11(4):354-358. 10.17085/apm.2016.11.4.354.
Effect of prolonged lateral position for 10-minutes following spinal anesthesia on hypotension and sensory blockade during cesarean delivery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. songoficu@gmail.com
- 2Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea.
- KMID: 2358330
- DOI: http://doi.org/10.17085/apm.2016.11.4.354
Abstract
- BACKGROUND
During cesarean delivery, hypotension is a frequently occurring adverse effect following spinal anesthesia. Our hypothesis was that hypotension could be avoided or delayed with a lateral decubitus position for 10 minutes after intrathecal injection, by reducing the detrimental effects of the aortocaval compression.
METHODS
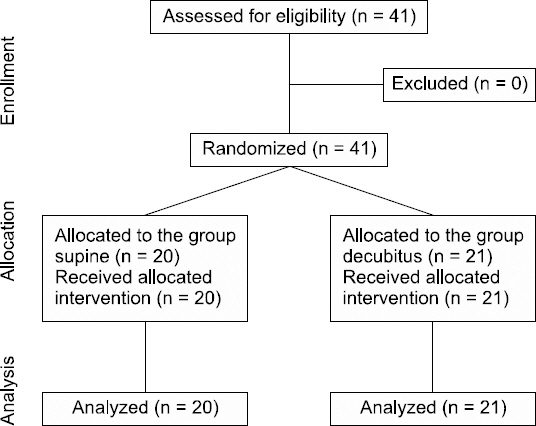
Spinal anesthesia was performed in the lateral decubitus position with 8 mg of 0.5% hyperbaric bupivacaine and 15 µg of fentanyl. Forty-one patients undergoing elective cesarean delivery were randomly assigned to one of two groups. In the experimental group, patients were maintained in the lateral position for 10 minutes following intrathecal injection (group Decubitus). In the control group, patients were repositioned to supine immediately after the injection (group Supine). Incidence of hypotension, the required dose of ephedrine, and characteristics of the sensory blockade, were subsequently investigated.
RESULTS
The incidence of hypotension, the incidence of nausea, and total amount of ephedrine, were not statistically different between the two groups. In group Decubitus, the onset of hypotension was delayed significantly (5.6 ± 1.7 min vs. 13.8 ± 1.7 min, P < 0.001), and the maximal blockade level was more cephalad (T3 [T1-T4] vs. T4 [T3-T5], P < 0.001) when compared to that of group Supine. Apgar scores were comparable in both groups.
CONCLUSIONS
Maintaining the lateral position for 10 min following intrathecal injection during cesarean delivery did not influence the incidence of maternal hypotension. However, it caused delayed onset of hypotension and higher cephalad spread of sensory block.
MeSH Terms
Figure
Reference
-
1. Simon L, Boulay G, Ziane AF, Noblesse E, Mathiot JL, Toubas MF, et al. Effect of injection rate on hypotension associated with spinal anesthesia for cesarean section. Int J Obstet Anesth. 2000; 9:10–4. DOI: 10.1054/ijoa.1999.0348. PMID: 15321104.
Article2. Rout CC, Rocke DA. Prevention of hypotension following spinal anesthesia for cesarean section. Int Anesthesiol Clin. 1994; 32:117–35. DOI: 10.1097/00004311-199432020-00010.
Article3. Bhagwanjee S, Rocke DA, Rout CC, Koovarjee RV, Brijball R. Prevention of hypotension following spinal anaesthesia for elective caesarean section by wrapping of the legs. Br J Anaesth. 1990; 65:819–22. DOI: 10.1093/bja/65.6.819. PMID: 2265052.
Article4. Hwang JW, Oh AY, Song IA, Na HS, Ryu JH, Park HP, et al. Influence of a prolonged lateral position on induction of spinal anesthesia for cesarean delivery: a randomized controlled trial. Minerva Anestesiol. 2012; 78:646–52. PMID: 22410469.5. Povey HM, Jacobsen J, Westergaard-Nielsen J. Subarachnoid analgesia with hyperbaric 0.5% bupivacaine: effect of a 60-min period of sitting. Acta Anaesthesiol Scand. 1989; 33:295–7. DOI: 10.1111/j.1399-6576.1989.tb02911.x. PMID: 2655366.6. Arai YC, Ueda W, Takimoto E, Manabe M. The influence of hyperbaric bupivacaine temperature on the spread of spinal anesthesia. Anesth Analg. 2006; 102:272–5. DOI: 10.1213/01.ANE.0000184252.16045.0E. PMID: 16368842.
Article7. Kuusniemi KS, Pihlajamäki KK, Pitkänen MT, Helenius HY, Kirvelä OA. The use of bupivacaine and fentanyl for spinal anesthesia for urologic surgery. Anesth Analg. 2000; 91:1452–6. DOI: 10.1097/00000539-200012000-00029. PMID: 11093999.
Article8. Hartmann B, Junger A, Klasen J, Benson M, Jost A, Banzhaf A, et al. The incidence and risk factors for hypotension after spinal anesthesia induction: an analysis with automated data collection. Anesth Analg. 2002; 94:1521–9. DOI: 10.1097/00000539-200206000-00027. PMID: 12032019.
Article9. Ohpasanon P, Chinachoti T, Sriswasdi P, Srichu S. Prospective study of hypotension after spinal anesthesia for cesarean section at Siriraj Hospital: incidence and risk factors, Part 2. J Med Assoc Thai. 2008; 91:675–80. PMID: 18672631.10. Carpenter RL, Caplan RA, Brown DL, Stephenson C, Wu R. Incidence and risk factors for side effects of spinal anesthesia. Anesthesiology. 1992; 76:906–16. DOI: 10.1097/00000542-199206000-00006. PMID: 1599111.
Article11. Brenck F, Hartmann B, Katzer C, Obaid R, Brüggmann D, Benson M, et al. Hypotension after spinal anesthesia for cesarean section: identification of risk factors using an anesthesia information management system. J Clin Monit Comput. 2009; 23:85–92. DOI: 10.1007/s10877-009-9168-x. PMID: 19277879.
Article12. Song IA, Shin WK, Hyun SJ, Park SJ, Ryu J, Jeon YT, et al. The impact of anthrometric measurements on hypotension during spinal anesthesia for cesarean delivery: comparison of body weight, body height, body mass index, and abdominal circumference. Anesth Pain Med. 2012; 7:355–8.13. Coppejans HC, Hendrickx E, Goossens J, Vercauteren MP. The sitting versus right lateral position during combined spinal-epidural anesthesia for cesarean delivery: block characteristics and severity of hypotension. Anesth Analg. 2006; 102:243–7. DOI: 10.1213/01.ane.0000189049.11005.26. PMID: 16368837.
Article14. Stoneham MD, Eldridge J, Popat M, Russell R. Oxford positioning technique improves haemodynamic stability and predictability of block height of spinal anaesthesia for elective caesarean section. Int J Obstet Anesth. 1999; 8:242–8. DOI: 10.1016/S0959-289X(99)80104-6.
Article15. Rucklidge MW, Paech MJ, Yentis SM. A comparison of the lateral, Oxford and sitting positions for performing combined spinal-epidural anaesthesia for elective Caesarean section. Anaesthesia. 2005; 60:535–40. DOI: 10.1111/j.1365-2044.2005.04178.x. PMID: 15918823.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minor Factors Influencint to the Sensory Blockade Level of Spinal Anesthesia at the L2, 3 Interspace
- Effects of fetal position on maternal hemodynamics after spinal anesthesia for cesarean delivery
- Intrathecal meperidine as the sole agent for cesarean section
- Spinal Anesthesia Using 0.5% Hyperbaric Bupivacine/Fentanyl Mixture for Cesarean Section
- The Analysis of Perfusion Index and Plethysmographic Variability Index During Elective Cesarean Section