Korean J Neurotrauma.
2016 Oct;12(2):152-155. 10.13004/kjnt.2016.12.2.152.
Intracerebral Hemorrhagic Infarction after Cranioplasty in a Patient with Sinking Skin Flap Syndrome
- Affiliations
-
- 1Department of Neurosurgery, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea. mslee@chungbuk.ac.kr
- KMID: 2356791
- DOI: http://doi.org/10.13004/kjnt.2016.12.2.152
Abstract
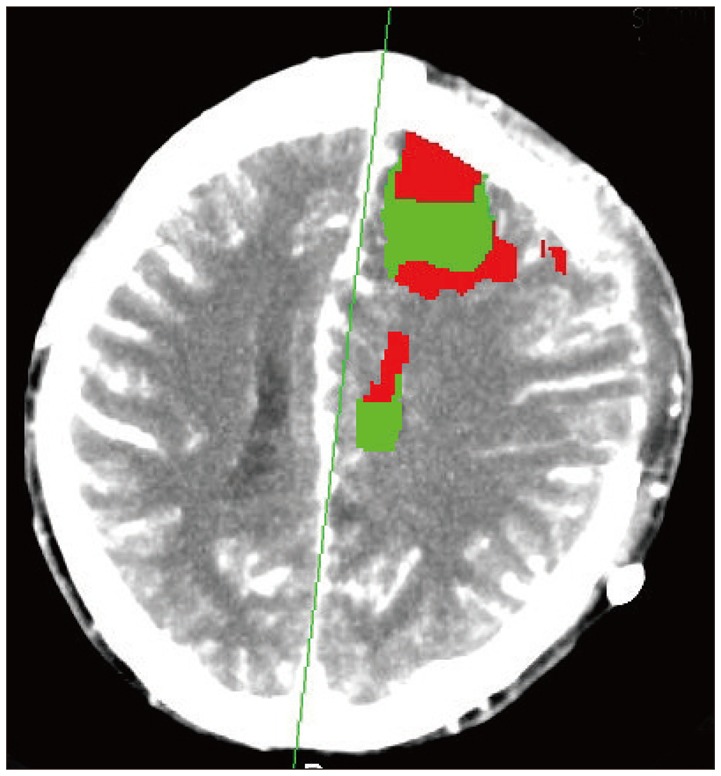
- The sinking skin flap syndrome (SSFS) is a rare complication after a large craniectomy. Hemorrhage infarction after a cranioplasty is a very rare complication with only 4 cases to date. We report a case of the patient who underwent an autologous cranioplasty to treat SSFS that developed intracerebral hemorrhage infarction. A 20-year-old male was admitted to our emergency department with stuporous mentality. Emergent decompressive craniectomy (DC) have done. He had suffered from SSFS and fever of unknown origin (FUO) since DC. After 7 months of craniectomy, cranioplasty was done. After 1 day of surgery, acute infarction with hemorrhagic transformation involved left cerebral hemisphere. We controlled increased intracranial pressure by using osmotic diuretics, steroid and antiepileptic drugs. After 14 day of surgery, he improved neurological symptoms and he had not any more hyperthermia. Among several complication of large cranioplasty only 4 cases of intracerebral hemorrhagic infarction due to reperfusion injury has been reported. In this case, unstable autoregulation system made brain hypoxic damage and then reperfusion and recanalization of cerebral vessels resulted in intracerebral hemorrhagic infarction. 7 month long FUO was resolved by cranioplasty.
MeSH Terms
Figure
Reference
-
1. Akins PT, Guppy KH. Sinking skin flaps, paradoxical herniation, and external brain tamponade: a review of decompressive craniectomy management. Neurocrit Care. 2008; 9:269–276. PMID: 18064408.
Article2. Annan M, De Toffol B, Hommet C, Mondon K. Sinking skin flap syndrome (or syndrome of the trephined): a review. Br J Neurosurg. 2015; 29:314–318. PMID: 25721035.
Article3. Cecchi PC, Rizzo P, Campello M, Schwarz A. Haemorrhagic infarction after autologous cranioplasty in a patient with sinking flap syndrome. Acta Neurochir (Wien). 2008; 150:409–410. discussion 411. PMID: 18246457.
Article4. Chitale R, Tjoumakaris S, Gonzalez F, Dumont AS, Rosenwasser RH, Jabbour P. Infratentorial and supratentorial strokes after a cranioplasty. Neurologist. 2013; 19:17–21. PMID: 23269102.
Article5. Creutzfeldt CJ, Vilela MD, Longstreth WT Jr. Paradoxical herniation after decompressive craniectomy provoked by lumbar puncture or ventriculoperitoneal shunting. J Neurosurg. 2015; 123:1170–1175. PMID: 26067613.
Article6. Eom KS, Kim DW, Kang SD. Bilateral diffuse intracerebral hemorrhagic infarction after cranioplasty with autologous bone graft. Clin Neurol Neurosurg. 2010; 112:336–340. PMID: 19896762.
Article7. Kwon SM, Cheong JH, Kim JM, Kim CH. Reperfusion injury after autologous cranioplasty in a patient with sinking skin flap syndrome. J Korean Neurosurg Soc. 2012; 51:117–119. PMID: 22500207.
Article8. Narro-Donate JM, Huete-Allut A, Escribano-Mesa JA, Rodríguez-Martínez V, Contreras-Jiménez A, Masegosa-González J. Paradoxical transtentorial herniation, extreme trephined syndrome sign: a case report. Neurocirugia (Astur). 2015; 26:95–99. PMID: 25455761.9. Ng D, Dan NG. Cranioplasty and the syndrome of the trephined. J Clin Neurosci. 1997; 4:346–348. PMID: 18638981.
Article10. Sakamoto S, Eguchi K, Kiura Y, Arita K, Kurisu K. CT perfusion imaging in the syndrome of the sinking skin flap before and after cranioplasty. Clin Neurol Neurosurg. 2006; 108:583–585. PMID: 15921849.
Article11. Sung JJ, Mapstone TB, El-Amm CA. Spontaneous resolution of diabetes insipidus after cranioplasty and cranial defect repair. J Craniofac Surg. 2011; 22:1536–1537. PMID: 21778861.
Article12. Wang QP, Zhou ZM, You C. Paradoxical herniation caused by cerebrospinal fluid drainage after decompressive craniectomy. Neurol India. 2014; 62:79–80. PMID: 24608467.
Article13. Winkler PA, Stummer W, Linke R, Krishnan KG, Tatsch K. The influence of cranioplasty on postural blood flow regulation, cerebrovascular reserve capacity, and cerebral glucose metabolism. Neurosurg Focus. 2000; 8:e9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reperfusion Injury after Autologous Cranioplasty in a Patient with Sinking Skin Flap Syndrome
- Bilateral Multiple Intracerebral Hemorrhagic Infarction after Cranioplasty in a Patient with Cerebral Infarction: Case Report
- "Syndrome of the Sinking Skin-Flap" Secondary to the Ventriculoperitoneal Shunt after Craniectomy
- Sinking Skin Flap Syndrome after Craniectomy in a Patient Who Previously Underwent Ventriculoperitoneal Shunt
- Sinking Skin Flap Syndrome after Decompressive Craniotomy